Fig. 17.1
Ilioinguinal nerve stimulation
Chronic orchialgia may be caused by structural abnormalities including wallerian degeneration of the spermatic cord or vasal nerves. This may explain how neurostimulation of the spermatic nerves provides pain relief in patients with chronic testicular pain. Other causes of orchialgia include postoperative scarring, trauma, and chronic infection leading to nerve damage (Fig. 17.2).


Fig. 17.2
Spermatic nerve stimulation
17.2 Selection of Candidates
Pelvic, sacral, rectal, and groin pain are complicated patient complaints that can be experienced by an eclectic group of individuals. Some of these patients are excellent candidates for stimulation whereas other patient populations have a poor prognosis. Table 17.1 identifies the important factors to consider when selecting patients for this procedure and their predictive impact on outcome.
Table 17.1
Important factors to consider when selecting patients
Factor | Consideration | Predictor |
|---|---|---|
Pain generator is understood | Diagnostic workup has shown an objective abnormality | Positive |
History of sexual or mental abuse | Psychological evaluation and workup | Negative |
Disease is stable | No progressive condition is present | Positive |
Previous treatment | History suggests some relief from other treatments | Positive |
Coexisting disease | History of fibromyalgia, irritable bowel, fatigue | Negative |
Pain character | Pain is burning or stabbing in nature | Positive |
Drug abuse | Active drug abuse behavior | Negative |
Bleeding disorders | History of active coagulopathy | Negative |
17.3 Technical Overview
Traditionally four methods are used for percutaneous access to stimulate the sacral nerve roots. One surgical method to stimulate the nerves has been described.
17.3.1 Sacral Nerve Stimulation
17.3.1.1 The Retrograde Technique
The retrograde approach became very popular over the past 10 years. This method involves the placement of the epidural needle into the spinal canal, directing the bevel from a cephalad to a caudad position. The needle is placed under fluoroscopic guidance and thereafter the lead is directed from the epidural entry zone downward until it is secured in the area of the S2, S3, and S4 nerve roots unilaterally or bilaterally. The leads are then secured to the fascia and ligament at the needle entry site. This approach is usually attempted with a needle entry at L2–3 or L3–4. Entry at the LS–S1 level is difficult owing to spinal angulation and may lead to difficulty in advancing the lead into the dorsal epidural space. The disadvantage of the technique is the risk of wet tap, nerve irritation with lead placement, and potential inability to pass the lead distally (Fig. 17.3).
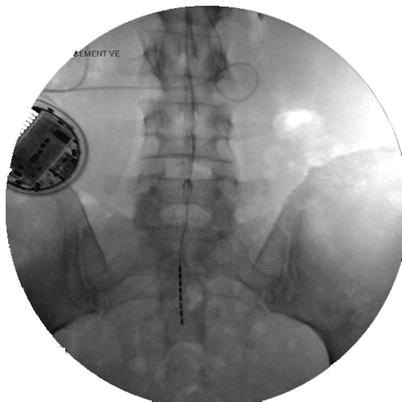
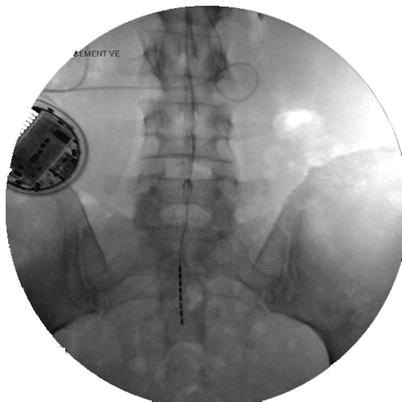
Fig. 17.3
Sacral stimulation with retrograde lead
17.3.1.2 The Lumbar Transforaminal Technique
The lumbar transforaminal approach involves placing a needle in the superior aspect of the lumbar nerve root foramen and then passing the lead inferiorly until the lead is satisfactorily placed over the sacral targets. This approach is technically difficult, may result in dorsal root entry zone injury, and may lead to difficulty in directing the lead inferiorly owing to an unsatisfactory entry angle of the lead at the foraminal entry zone. This method is covered in detail elsewhere in this Atlas.
17.3.1.3 The Sacral Transforaminal Technique
The sacral transforaminal approach involves placing the lead directly through the sacral foramen to the target nerve. This approach has been used to treat incontinence by direct nerve stimulation and to treat chronic pain. This approach is simple but has complication risks. The approach may lead to nerve injury and is difficult to anchor once the device is in place (Fig. 17.4).
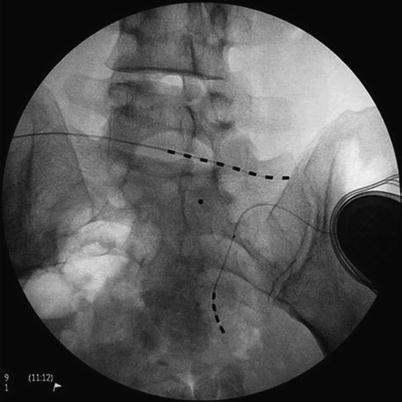
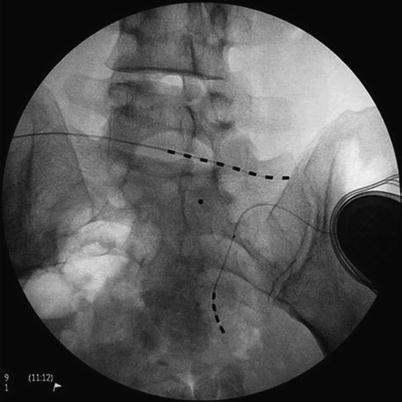
Fig. 17.4
Sacral transforaminal lead placement (lower lead)
17.3.1.4 The Sacral Hiatus or Caudal Approach Technique
The sacral hiatus can be entered by placing an epidural introducer needle into the caudal space and then driving the lead laterally to stimulate the sacral nerve targets. The target may be in the midline if the pain is in the rectum or coccyx. The advantage of this technique is the simple approach and ease of driving the lead. The disadvantage of the technique is the difficulty of anchoring the lead as it exits the sacral hiatus, especially if the body fat is not appropriate to give adequate coverage over the lead or anchor. If erosion is a risk, the permanent lead must be placed using the neurosurgical technique (Fig. 17.5).