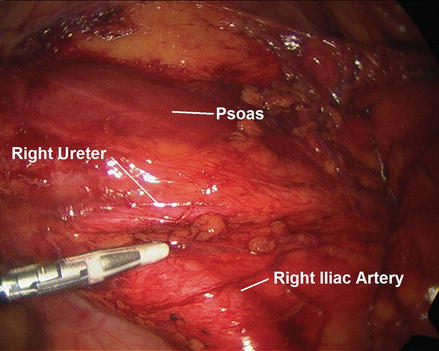
Figure 22.1
The right colon is retracted medial while dividing the lateral peritoneal attachments, taking care to identify and preserve the right ureter. As the dissection is carried superiorly, the duodenum must be identified and protected
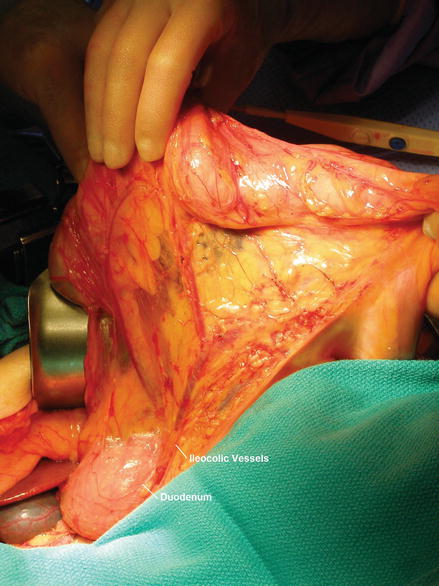
Figure 22.2
As the right colon is mobilized and rotated medially, the second and third portion of the duodenum should be identified and kept posterior
The omentum is dissected free from the transverse colon at the distal resection site and divided using either the clamp and tie technique, or using a vessel sealing device (ultrasonic coagulating shears or electrothermal bipolar vessel sealers). If performing the operation for benign disease, the mesenteric attachments of the right colon can be divided close to the mesenteric border of the colon. If the operation is performed for malignancy, the resection site should be chosen to ensure a luminal margin of at least 5 cm [11]. A window is created in the transverse mesocolon at the site where the colon will be divided, the marginal artery of Drummond is ligated and divided, and the transverse mesocolon is divided down to the base of the mesentery to identify the middle colic vessel bifurcation. The right branch of the middle colic is ligated and divided at its origin while the left branch is preserved. If the lesion is at the hepatic flexure or proximal transverse colon, the specimen can be extended by dividing the middle colic vessels at their base. If the right colic vessels are present, these are also divided at their origin, and the mesentery is divided down to the base of the ileocolic vessels (Fig. 22.3), which are also ligated and divided. The mesentery of the terminal ileum is divided, and the proximal margin of the specimen should include 5–10 cm of small bowel [11, 12], although more can be excised for cecal tumors. The specimen is opened on the back table and inspected to ensure that it contains the lesion of interest and margins are appropriate. It can then be passed off the table and sent to surgical pathology.
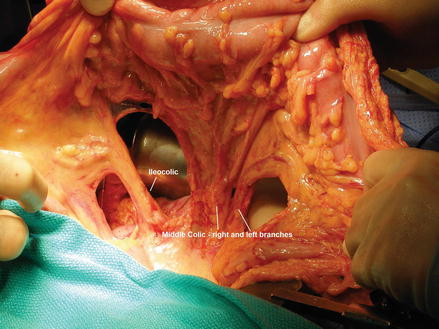
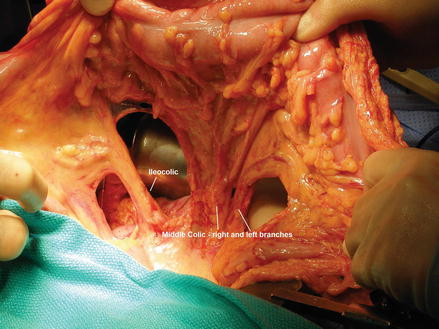
Figure 22.3
The mesentery of the right colon and, if necessary, the transverse colon is ligated. When malignant disease is resected, the ileocolic and right colic (if present) vessels are identified and divided near their origin to allow for adequate lymph node sampling. The right branch of the middle colic is usually divided at its bifurcation from the left branch
The ileocolic anastomosis can be created either in a hand-sewn or stapled fashion. We describe the side-to-side stapled approach. After initially dividing the mesentery as already described, the ileum and transverse colon are aligned side by side and enterotomies are made on the antimesenteric borders of both limbs of bowel. The two halves of a linear stapler (typically 75 or 80 mm) are passed into the lumen of both the large and small bowel (Fig. 22.4). After firing the stapler, the intraluminal staple lines are inspected for bleeding. The anterior and posterior staple lines should be slightly off-set, and a 60-mm transverse non-cutting stapler is used to close the end of the anastomosis distal to the prior enterotomies (Fig. 22.5). The bowel is divided sharply on the stapler. This staple line can be oversewn if desired with interrupted imbricating sutures, and the mesenteric defect can be closed with a running absorbable suture to prevent risk of internal hernia. The abdomen is irrigated, inspected for bleeding, and the fascia is closed with running absorbable suture. The subcutaneous tissue is again irrigated, and the skin is closed.
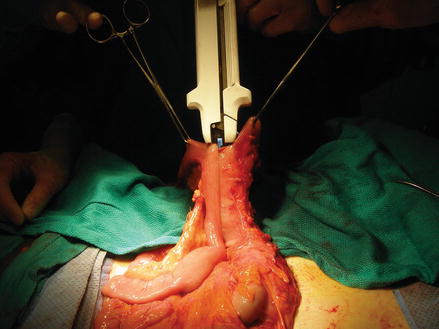
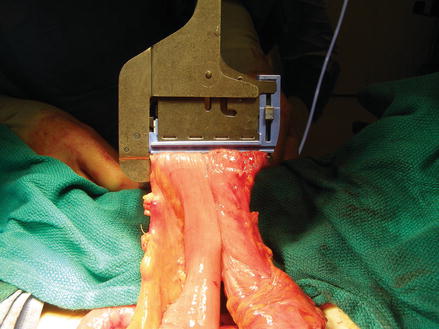
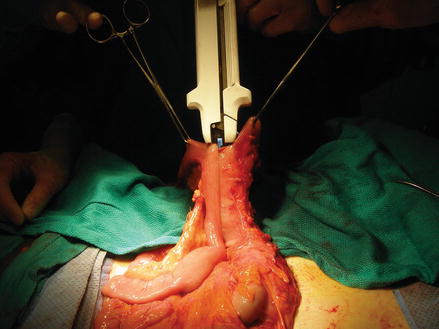
Figure 22.4
The side-to-side stapled anastomosis is constructed after resecting the specimen. Each half of the linear cutting stapler is passed through enterotomies in the terminal ileum (left) and transverse colon (right). Firing the stapler creates a lumen through the antimesenteric borders of the intestine
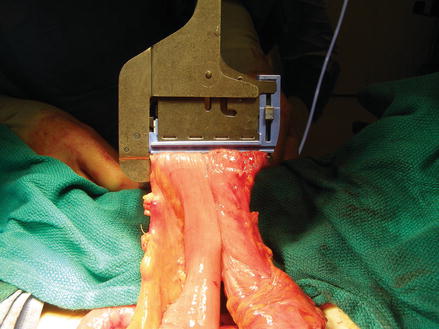
Figure 22.5
The common enterotomy from the side-to-side stapled anastomosis is closed using the transverse non-cutting stapler. Care is taken not to narrow the newly created lumen, and the staple line can be oversewn
Laparoscopic Assisted Right Hemicolectomy
Laparoscopic assisted right hemicolectomy can be performed under general anesthetic with similar preparation and positioning as described above. Because of the reduction of tactile sensation during the laparoscopic portion of the case, tattooing of the lesion colonoscopically takes on increased importance.
The abdomen can be entered using a Veress needle technique or the Hasson technique [13]. With the Hasson approach a 1–1.5 cm peri-umbilical incision is made and dissection is carried down until the linea alba can be identified and elevated. This is divided, and the peritoneum is sharply incised. Stay sutures are placed at the lateral edges of the fascia, and the 12 mm Hasson trocar is inserted into the abdomen. The stay sutures are used to secure the trocar in place, and the abdomen is insufflated to 15 mmHg with carbon dioxide. The laparoscope is inserted, and the abdomen is inspected for injury during insertion and for other intra-abdominal pathology which may preclude resection. In general, a 30 ° scope is utilized for this procedure. Additional 5 mm ports are placed in the supra-pubic midline and in the left lower quadrant; a third port can be placed in the left upper quadrant or in the right lower quadrant, depending on the need during dissection.
The colon may be mobilized using either a lateral to medial or medial to lateral approach. The lateral to medial approach is as follows: the patient is placed in Trendelenberg with tilt to elevate the right side. The terminal ileum is identified and retracted anteriorly, as is the appendix and cecum to allow incision of the peritoneal attachments. These are divided and dissection continues in a cephalad direction, taking care to identify the gonadal vessels and the right ureter as it passes over the right common iliac vessels and ensure that this remains posterior as the colon is mobilized anteriorly (Fig. 22.6). As the dissection approaches the hepatic flexure, the duodenum must be identified and protected (Fig. 22.7). The hepatocolic ligament and omental attachments are divided after placing the patient in a reverse Trendelenberg position. After completing the mobilization of the specimen, the terminal ileum and ascending colon are elevated to identify the ileocolic vessels at their origin (Fig. 22.8). A window is created on either side, and the vessels are divided using a vessel sealing or stapling device.