TOPICS
1. The clinical signs and symptoms of TV diseases
4. Echocardiography of right heart structures and right ventricular function.
5. Surgical approaches to TV diseases
6. Anesthetic implications of TV diseases, pulmonary hypertension, and RV failure.
Much as the mitral valve (MV) and aortic valve (AV) direct blood flow into the systemic circulation, the tricuspid valve (TV) and the pulmonic valve (PV) direct flow into the pulmonary circulation. A functioning right ventricle (RV) is critical to effective loading of the left ventricle (LV). Perioperative RV failure can be quite challenging for the anesthesiologist as it often occurs in the setting of pulmonary artery hypertension, which can be difficult to treat.
THE CLINICAL SIGNS AND SYMPTOMS OF TV DISEASES
The TV can develop both stenotic and regurgitant lesions. Tricuspid stenosis (TS) is most often secondary to rheumatic heart disease. Less encountered causes are carcinoid and endomyocardial fibrosis. Obstructing cardiac masses can also occlude the TV.1
Tricuspid regurgitation (TR) occurs secondary to pathologic processes affecting the valve itself or as a consequence of RV dilatation. RV dilatation may occur in the setting of pressure or volume overload. Increased RV systolic pressure develops when the RV must work against an increased resistance. This can occur in clinical situations, which increase pulmonary artery (PA) pressure such as mitral stenosis, severe mitral regurgitation, severe left ventricular dysfunction, pulmonary embolism, primary pulmonary hypertension, or lung disease.
Endocarditis, connective tissue diseases, carcinoid syndrome, anorectic drugs (fenfluramine), Ebstein abnormality (an apically positioned tricuspid valve), pergolide, and chest radiation therapy can likewise result in TR. Ebstein anomaly is due to apical displacement of the tricuspid valve leaflets especially the septal leaflet associated with TR and RV dysfunction.
Patients with TS frequently present with other valvular diseases associated with rheumatic heart disease (eg, mitral stenosis, aortic stenosis). Consequently, their clinical features often represent the impact of these lesions. Long before the patient presents for surgery, echocardiography will have diagnosed any associated lesions.
The patient with TR secondary to pulmonary hypertension is likely to present with signs of right heart failure and systemic venous engorgement. Peripheral edema, hepatic dysfunction, and ascites frequently occur. Systolic pulmonary pressures greater than 55 mm Hg1 will readily produce TR even with normal valve structure. Transvenous pacemaker wires or catheters can both cause a mild degree of TR as well. Additionally, many patients have echocardiographically detected TR without clinical significance.
RV FUNCTION
The right ventricle and the interaction between the right and left heart are critical to maintaining healthy cardiovascular function. Although patients can survive with only a single ventricle devoted to the systemic circulation (eg, Fontan circulation—Chapter 12), a functioning right heart effectively loads the LV so that the stroke volume (SV) is ejected systemically. When the RV fails, the LV may be inadequately loaded reducing SV.
RV failure can develop both acutely and chronically. Acute RV failure can be seen associated with sudden increases in pulmonary vascular resistance (eg, during a protamine reaction) or secondary to myocardial ischemia and infarction. Chronic RV failure presents secondary to progressive increases in pulmonary hypertension (eg, from mitral stenosis, lung diseases, etc) or volume overload as seen in intracardiac left-to-right shunts or primary tricuspid regurgitation.
Both acute and chronic RV failure lead to RV dilatation and TR. Moreover, as the RV dilates the flattening of the intraventricular septum can distort the LV cavity due to interventricular dependence, further impeding LV function. Consequently, failure of the RV reduces LV function leading to decreased cardiac output and hypotension. Acute RV failure during protamine administration for heparin reversal after discontinuation of cardiopulmonary bypass is a dramatic, life-threatening occurrence. As PA pressures increase, the RV distends unable to overcome the pressure load presented to it. The patient develops TR and the LV is severely underloaded. Systemic hypotension can be severe and circulatory collapse imminent. Often, it becomes necessary to reheparinize the patient and institute emergent cardiopulmonary bypass.
Therapy for RV failure is directed at the etiology whether it is restoration of myocardial perfusion in case of myocardial ischemia or decreasing PA pressures during acute increases of pulmonary vascular resistance.
There are no specific inotropic agents that directly target the right ventricle. Milrinone, dobutamine, levosimendan2–5 can all be employed to improve RV contractility. These agents have inotropic effects upon both the left and the right ventricle and will likewise vasodilate both the systemic and pulmonary circulations. Reduction of pulmonary vascular resistance can improve RV function, LV function, and RVLV interaction. Vasodilators including sodium nitroprusside and nitroglycerin will lower both systemic and pulmonary vascular resistance and can be useful assuming the impact upon systemic pressure does not outweigh any benefit resulting from the diminution of pulmonary vascular resistance.
Nitric oxide (NO) is the molecule by which both nitroprusside and nitroglycerin ultimately produce vasodilatation. NO is present only minimally in the circulation and produces an increase in cGMP in vascular smooth muscle.6–8 Inhaled NO has been available for a number of years and can be delivered to directly dilate the pulmonary vasculature with minimal effects upon the systemic circulation.
Unique right heart cardiomyopathies can also present. Arrhythmogenic right cardiomyopathy9 occurs when the right heart undergoes fatty infiltration. Patients are at risk for sudden death from ventricular dysrhythmias. Often these patients will have been treated with an implantable cardioverter/defibrillator device. Hypertrophic cardiomyopathy (HCM) can likewise present in the right heart although to a far lesser degree than that seen in left heart HCM. A pressure gradient can develop across the right ventricular outflow tract leading to RV failure. These patients too are at risk for sudden cardiac death (SCD).
THE PULMONIC VALVE
Like all other heart valves the pulmonic valve can develop both stenotic and regurgitant lesions; however, it is least likely to be affected by acquired heart disease.1 Pulmonary stenosis (PS) may be congenital or acquired as seen in carcinoid syndrome. PS results in RV failure and underloading of the LV. Pulmonary regurgitation is also unusual but may occur due to annular dilatation as a result of pulmonary hypertension or following balloon valvuloplasty of a stenotic pulmonary valve. Additionally, patients following tetrology of Fallot repair frequently developed pulmonary regurgitation.
ECHOCARDIOGRAPHY OF RIGHT HEART STRUCTURES AND RIGHT VENTRICULAR FUNCTION
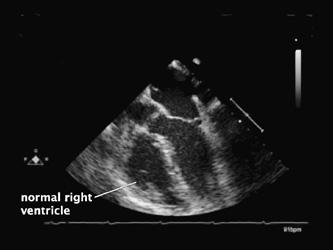
Right heart structures are located anteriorly and therefore away from the transesophageal echocardiography (TEE) probe. Consequently, they are less well visualized than those of the left ventricle. Nonetheless, TEE can assist in the perioperative discernment of both RV function and valvular integrity. The basic views of the right heart and its structures were discussed in the introduction to TEE.
RV function is not as easy to characterize on TEE as is that of the LV. Video 8–1 reveals a normally contracting RV. In contrast, Video 8–2 presents a dilated, dysfunctional RV. In this instance, the RV has dilated to overcome the increased resistance presented to it by chronic pulmonary hypertension eventually resulting in RV dilation and leftward movement of the intraventricular septum into the LV (Figures 8–1 and 8–2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree