CHAPTER 39
Rhinitis, Acute
(Runny Nose)
Presentation
In allergic rhinitis, patients typically complain of rhinorrhea (“runny nose”), nasal congestion, sneezing, nasal itching, and “itchy eyes.” There may be a problem with sleep disturbance (from nasal congestion), malaise, fatigue, irritability, and neurocognitive deficits.
Typically, patients with allergic rhinitis have clear discharge, swollen turbinates, and bluish or pale mucosa. There may be “allergic shiners”—infraorbital darkening thought to be caused by chronic venous pooling—or an “allergic salute” in children who rub their noses upward because of nasal discomfort, sometimes producing a persistent horizontal crease across the nose. Mild bilateral conjunctivitis with nonpurulent discharge is strongly suggestive of an allergic cause when it is accompanied by pruritus. The patient with a “summer cold” lasting a full month is likely to have allergic rhinitis.
Precipitating factors may be known or may be elicited from the patient. Common allergens include airborne dust-mite fecal particles, cockroach residues, animal danders (especially cats and dogs), molds, and pollens (hence the origin of the term hay fever). Vasomotor (idiopathic) rhinitis may occur in response to environmental conditions, such as changes in temperature or relative humidity, odors (e.g., perfume or cleaning materials), passive tobacco smoke, alcohol, sexual arousal, or emotional factors.
Drug-induced rhinitis may be caused by oral medications, including angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, various antihypertensive agents, chlorpromazine, aspirin, other nonsteroidal anti-inflammatory drugs (NSAIDs), and oral contraceptives as well as topical α-adrenergic decongestant sprays that have been used for more than 5 to 7 days (rhinitis medicamentosa). Repeated use of intranasal cocaine and methamphetamines may also result in rebound congestion and, on occasion, septal erosion and perforation.
In viral rhinitis, patients generally complain of an annoying, persistent mucoid nasal discharge accompanied by nasal and facial congestion, along with a constellation of viral symptoms, including low-grade fever, myalgias, and sore throat. These patients generally seek care, because they feel miserable, cannot sleep, and want relief. They often believe that antibiotics are needed to cure their problem.
On physical examination, there is only nasal mucous membrane congestion, which may appear erythematous, along with cloudy nasal secretions, which may become somewhat yellow and thick after several days. Resolution occurs within 10 days to 2 weeks.
Always keep in mind that young children may place intranasal foreign bodies in their noses (e.g., beads or beans), leading to foul-smelling, purulent, unilateral nasal discharge (see Chapter 29).
What To Do:
Allergic Rhinitis
 Determine which specific symptoms are most bothersome to the patient (e.g., nasal congestion, pruritus, rhinorrhea, sneezing), the pattern of the symptoms (e.g., intermittent, seasonal, perennial), any precipitating factors in the home or occupational environment, the response to previous medications, and any coexisting conditions.
Determine which specific symptoms are most bothersome to the patient (e.g., nasal congestion, pruritus, rhinorrhea, sneezing), the pattern of the symptoms (e.g., intermittent, seasonal, perennial), any precipitating factors in the home or occupational environment, the response to previous medications, and any coexisting conditions.
 Use a hand-held otoscope or headlamp with nasal speculum to view the anterior nasal airway. (A topical decongestant improves visualization of the nasal cavity.)
Use a hand-held otoscope or headlamp with nasal speculum to view the anterior nasal airway. (A topical decongestant improves visualization of the nasal cavity.)
 Educate the patient about avoidance of any known inciting factors. In particular, patients who are allergic to house dust mites should use allergen-impermeable encasings on the bed and pillows. For patients with seasonal allergies, pollen exposure can be reduced by having them keep windows closed, using an air conditioner, and limiting the amount of time spent outdoors.
Educate the patient about avoidance of any known inciting factors. In particular, patients who are allergic to house dust mites should use allergen-impermeable encasings on the bed and pillows. For patients with seasonal allergies, pollen exposure can be reduced by having them keep windows closed, using an air conditioner, and limiting the amount of time spent outdoors.
 Intranasal corticosteroids are the most effective medication class for treatment of allergic rhinitis and should be used as a single first-line agent; although, it should be kept in mind that these are generally expensive items. These preparations are generally not associated with significant systemic side effects in adults. Prescribe fluticasone (Flonase) nasal spray (which has been shown to be beneficial even when used on an as-needed basis) for adults and children older than 12 years of age, 2 sprays (50 µg/spray) in each nostril qd, or 1 spray in each nostril bid. Other options include flunisolide (Nasalide) nasal spray, 2 sprays in each nostril bid (may increase to tid to qid), or, for children 6 to 14 years old, 1 spray in each nostril tid or 2 sprays each nostril bid; mometasone furoate (Nasonex) for adults and children older than 12 years of age, 2 sprays in each nostril qd; and budesonide (Rhinocort Aqua) nasal spray for adults and children older than 6 years of age, 1 spray in each nostril qam.
Intranasal corticosteroids are the most effective medication class for treatment of allergic rhinitis and should be used as a single first-line agent; although, it should be kept in mind that these are generally expensive items. These preparations are generally not associated with significant systemic side effects in adults. Prescribe fluticasone (Flonase) nasal spray (which has been shown to be beneficial even when used on an as-needed basis) for adults and children older than 12 years of age, 2 sprays (50 µg/spray) in each nostril qd, or 1 spray in each nostril bid. Other options include flunisolide (Nasalide) nasal spray, 2 sprays in each nostril bid (may increase to tid to qid), or, for children 6 to 14 years old, 1 spray in each nostril tid or 2 sprays each nostril bid; mometasone furoate (Nasonex) for adults and children older than 12 years of age, 2 sprays in each nostril qd; and budesonide (Rhinocort Aqua) nasal spray for adults and children older than 6 years of age, 1 spray in each nostril qam.
 Patients should be instructed to direct sprays away from the nasal septum to avoid irritation and not to tilt the head back when spraying, to avoid having the drug run out of the nasal cavity and into the throat.
Patients should be instructed to direct sprays away from the nasal septum to avoid irritation and not to tilt the head back when spraying, to avoid having the drug run out of the nasal cavity and into the throat.
 Antihistamines are a second-line agent in allergic rhinitis treatment but have less effect on nasal congestion. Prescribe a nonsedating second-generation antihistamine, such as fexofenadine (Allegra), 180 mg qd (for children 6 to 11 years old, 30 mg bid); desloratadine (Clarinex), 5 mg qd; loratadine (Claritin), 10 mg qd, or syrup, 10 mg/10 mL (for children 2 to 5 years old, 5 mg qd; for children 6 to 11 years old, 10 mg qd); cetirizine (Zyrtec), 5 to 10 mg qd, or syrup, 5 mg/5 mL (for children 2 to 5 years old, ½ to 1 tsp [2 to 2.5 mg] qd; for children 6 to 11 years old, 1 to 2 tsp [5 to 10 mg] qd).
Antihistamines are a second-line agent in allergic rhinitis treatment but have less effect on nasal congestion. Prescribe a nonsedating second-generation antihistamine, such as fexofenadine (Allegra), 180 mg qd (for children 6 to 11 years old, 30 mg bid); desloratadine (Clarinex), 5 mg qd; loratadine (Claritin), 10 mg qd, or syrup, 10 mg/10 mL (for children 2 to 5 years old, 5 mg qd; for children 6 to 11 years old, 10 mg qd); cetirizine (Zyrtec), 5 to 10 mg qd, or syrup, 5 mg/5 mL (for children 2 to 5 years old, ½ to 1 tsp [2 to 2.5 mg] qd; for children 6 to 11 years old, 1 to 2 tsp [5 to 10 mg] qd).
 An alternative to oral antihistamines is the intranasal antihistamine azelastine (Astelin Nasal Spray) for adults and children older than 12 years of age, 2 sprays per nostril bid. Side effects many include a bitter taste in the mouth and sedation.
An alternative to oral antihistamines is the intranasal antihistamine azelastine (Astelin Nasal Spray) for adults and children older than 12 years of age, 2 sprays per nostril bid. Side effects many include a bitter taste in the mouth and sedation.
 Topical decongestant nasal sprays and oral decongestants can effectively reduce nasal congestion for both allergic and nonallergic forms of rhinitis, but they can cause side effects (especially the oral forms) of insomnia, nervousness, loss of appetite, and urinary retention in males. They should be used with caution or not at all in patients with arrhythmias, hypertension, or hyperthyroidism. Prescribe pseudoephedrine (Sudafed), 60 mg q6h; time-released version, 120 mg bid, or syrup, 3 mg/mL (for children 2 to 5 years old, 5 to 30 mg q4-6h; for children 6 to 12 years old, 30 mg q4-6h or 4 mg/kg/day divided q6h [1 mg/kg/dose]).
Topical decongestant nasal sprays and oral decongestants can effectively reduce nasal congestion for both allergic and nonallergic forms of rhinitis, but they can cause side effects (especially the oral forms) of insomnia, nervousness, loss of appetite, and urinary retention in males. They should be used with caution or not at all in patients with arrhythmias, hypertension, or hyperthyroidism. Prescribe pseudoephedrine (Sudafed), 60 mg q6h; time-released version, 120 mg bid, or syrup, 3 mg/mL (for children 2 to 5 years old, 5 to 30 mg q4-6h; for children 6 to 12 years old, 30 mg q4-6h or 4 mg/kg/day divided q6h [1 mg/kg/dose]).
 Two effective nasal decongestant sprays are oxymetazoline (Afrin) 0.05%, 2 sprays per nostril bid (or, for pediatric patients, 0.025%, 1 to 2 sprays per nostril bid), and phenylephrine (Neo-Synephrine Nasal) 0.025%, 0.05%, or 1%, 1 to 2 sprays per nostril q3-4h (or, for pediatric patients older than 2 years, 0.125% or 0.25%). Use must be limited to 3 to 5 days to avoid rebound nasal congestion (rhinitis medicamentosa).
Two effective nasal decongestant sprays are oxymetazoline (Afrin) 0.05%, 2 sprays per nostril bid (or, for pediatric patients, 0.025%, 1 to 2 sprays per nostril bid), and phenylephrine (Neo-Synephrine Nasal) 0.025%, 0.05%, or 1%, 1 to 2 sprays per nostril q3-4h (or, for pediatric patients older than 2 years, 0.125% or 0.25%). Use must be limited to 3 to 5 days to avoid rebound nasal congestion (rhinitis medicamentosa).
 The same cautions and contraindications exist for nasal decongestants as for the oral medications. Because of the use of pseudoephedrine in the illegal manufacture of amphetamine drugs, it now must be purchased behind the counter.
The same cautions and contraindications exist for nasal decongestants as for the oral medications. Because of the use of pseudoephedrine in the illegal manufacture of amphetamine drugs, it now must be purchased behind the counter.
 Other products that have some efficacy in allergic rhinitis are cromolyn sodium, a mast cell stabilizer, and montelukast (Singulair), a leukotriene receptor antagonist, for adults, 10 mg qhs (for children 2 to 5 years old, 4 mg chewable tab qhs; for children 6 to 14 years old, 5 mg chewable tab qhs).
Other products that have some efficacy in allergic rhinitis are cromolyn sodium, a mast cell stabilizer, and montelukast (Singulair), a leukotriene receptor antagonist, for adults, 10 mg qhs (for children 2 to 5 years old, 4 mg chewable tab qhs; for children 6 to 14 years old, 5 mg chewable tab qhs).
 In addition, ipratropium bromide (Atrovent Nasal Spray) 0.06%, two sprays per nostril tid to qid have been shown to help but works best in vasomotor (idiopathic) rhinitis.
In addition, ipratropium bromide (Atrovent Nasal Spray) 0.06%, two sprays per nostril tid to qid have been shown to help but works best in vasomotor (idiopathic) rhinitis.
Viral Rhinitis
 Determine which specific symptoms are most bothersome to the patient (e.g., nasal congestion, rhinorrhea, scratchy throat, general aches, fever, or cough).
Determine which specific symptoms are most bothersome to the patient (e.g., nasal congestion, rhinorrhea, scratchy throat, general aches, fever, or cough).
 Perform a general examination, including a careful nasal examination, to exclude any associated diseases, such as rhinosinusitis, otitis media, bacterial pharyngitis, and asthmatic bronchitis.
Perform a general examination, including a careful nasal examination, to exclude any associated diseases, such as rhinosinusitis, otitis media, bacterial pharyngitis, and asthmatic bronchitis.
 For nasal congestion, prescribe oral or topical decongestants, as you would for allergic rhinitis (described earlier). For rhinorrhea, you can prescribe ipratropium bromide (Atrovent Nasal Spray) 0.06%, 2 sprays per nostril tid to qid.
For nasal congestion, prescribe oral or topical decongestants, as you would for allergic rhinitis (described earlier). For rhinorrhea, you can prescribe ipratropium bromide (Atrovent Nasal Spray) 0.06%, 2 sprays per nostril tid to qid.
 Although antihistamines are effective for treatment of rhinitis related to allergy, they are much less effective for rhinitis related to the common cold. The side effects often outweigh the benefit and thus are not recommended.
Although antihistamines are effective for treatment of rhinitis related to allergy, they are much less effective for rhinitis related to the common cold. The side effects often outweigh the benefit and thus are not recommended.
 Nasal saline irrigation has been shown to have some efficacy in the relief of viral rhinitis. This can easily be accomplished with a commercially available neti pot.
Nasal saline irrigation has been shown to have some efficacy in the relief of viral rhinitis. This can easily be accomplished with a commercially available neti pot.
 Provide symptomatic relief for associated symptoms (e.g., acetaminophen [Tylenol] or ibuprofen [Motrin] for fever, general aches, and scratchy throat, or albuterol [Ventolin] metered-dose inhaler for cough).
Provide symptomatic relief for associated symptoms (e.g., acetaminophen [Tylenol] or ibuprofen [Motrin] for fever, general aches, and scratchy throat, or albuterol [Ventolin] metered-dose inhaler for cough).
 When pain, redness and tender swelling around the nostrils occur because of nose picking or excessive rubbing or blowing of the nose (nasal vestibulitis) (Figure 39-1), treat with an antistaphylococcal antibiotic ointment—mupirocin (Bactroban) 2%, apply tid × 2 weeks—and recommend warm compresses. Patients with diabetes, immune deficiency, or progressive infection should be placed on a systemic antistaphylococcal antibiotic to avoid potential spread to the cavernous sinus.
When pain, redness and tender swelling around the nostrils occur because of nose picking or excessive rubbing or blowing of the nose (nasal vestibulitis) (Figure 39-1), treat with an antistaphylococcal antibiotic ointment—mupirocin (Bactroban) 2%, apply tid × 2 weeks—and recommend warm compresses. Patients with diabetes, immune deficiency, or progressive infection should be placed on a systemic antistaphylococcal antibiotic to avoid potential spread to the cavernous sinus.
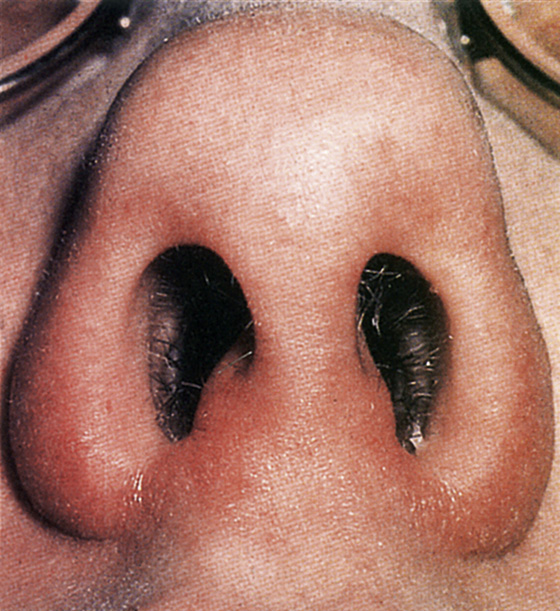
Figure 39-1 Example of nasal vestibulitis. (Adapted from Park YW, Littlejohn R, Eley J: Diagnosis at a glance. Emerg Med 5:9, 2002.)
What Not To Do:
 Do not prescribe sedating antihistamines for symptoms of hay fever.
Do not prescribe sedating antihistamines for symptoms of hay fever.
 Do not prescribe antihistamines or nasal steroids for the common cold.
Do not prescribe antihistamines or nasal steroids for the common cold.
 Do not obtain imaging studies of the sinuses unless the criteria for bacterial rhinosinusitis are met (symptoms lasting more than 7 days and including facial or dental pain or tenderness along with purulent nasal drainage).
Do not obtain imaging studies of the sinuses unless the criteria for bacterial rhinosinusitis are met (symptoms lasting more than 7 days and including facial or dental pain or tenderness along with purulent nasal drainage).
 Do not prescribe antibiotics for cold symptoms. Antibiotics should only be considered if symptoms persist for more than 7 days and are accompanied by signs of rhinosinusitis (see Chapter 40).
Do not prescribe antibiotics for cold symptoms. Antibiotics should only be considered if symptoms persist for more than 7 days and are accompanied by signs of rhinosinusitis (see Chapter 40).
 Do not bother recommending the use of zinc lozenges. Despite numerous randomized trials, the evidence for their effectiveness in reducing the duration of common cold symptoms is still lacking.
Do not bother recommending the use of zinc lozenges. Despite numerous randomized trials, the evidence for their effectiveness in reducing the duration of common cold symptoms is still lacking.
Discussion
Rhinitis is an inflammation of the nasal mucous membranes. Allergic rhinitis triggers a systemic increase in inflammation. Within minutes of allergen exposure, immune cells release histamine, proteases, cysteinyl leukotrienes, prostaglandins, and cytokines. Systemic circulation of inflammatory cells permits their infiltration into other tissues where chemoattractant and adhesion molecules already exist. Consequently, allergic rhinitis is linked to comorbid conditions: asthma, chronic hyperplastic eosinophilic sinusitis, nasal polyposis, and serous otitis media. Effective therapy should ideally be directed at the underlying inflammation and its systemic manifestations. It should improve the rhinitis and the comorbid conditions.
Antihistamines relieve early symptoms, but they do not significantly influence the proinflammatory loop. Oral corticosteroids provide the systemic anti-inflammatory effect needed, but their toxicity precludes extended routine use. Intranasal corticosteroids effectively target the local inflammatory processes of rhinitis, but they only reduce the local inflammatory cells within the nares. Leukotriene modifiers have both systemic anti-inflammatory effects and an acceptable safety profile.
Immunotherapy (allergy shots) is the only treatment that produces long-term relief of symptoms. Patients should be considered candidates for these treatments, based on the severity of their symptoms and the failure or unacceptability of the other treatment modalities.
Nasal polyps are benign inflammatory growths that arise from the inflamed mucosa lining the paranasal sinuses. They are frequently associated with sinus disease. Unilateral nasal polyps should raise consideration of a possible neoplasm.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



