CHAPTER 5 RESPIRATORY SYSTEM
INTERPRETATION OF BLOOD GASES
Most ICUs now have a blood gas analyser for ‘point of care testing’ (POCT). These are expensive to maintain and repair. You will be unpopular if you damage it by, for example, blocking the sample channels with clotted blood. If you do not know how to use it, ask for help. Normal blood gas values are as shown in Table 5.1.
TABLE 5.1 ‘Normal’ blood gas values
| pH | 7.35–7.45 |
| PaO2 | 13 kPa |
| PaCO2 | 5.3 kPa |
| HCO3 | 22–25 mmol/L |
| Base deficit or excess | −2 to +2 mmol/L |
 Note the inspired oxygen concentration (FiO2). The higher the FiO2 required to achieve any given PaO2 the more significant the problem (see below).
Note the inspired oxygen concentration (FiO2). The higher the FiO2 required to achieve any given PaO2 the more significant the problem (see below). Look again at the PaCO2. Is the PaCO2 consistent with the change in pH, i.e. if the patient is acidotic, is the PaCO2 raised? If the patient is alkalotic, is the PaCO2 low? If so the primary abnormality is likely to be respiratory.
Look again at the PaCO2. Is the PaCO2 consistent with the change in pH, i.e. if the patient is acidotic, is the PaCO2 raised? If the patient is alkalotic, is the PaCO2 low? If so the primary abnormality is likely to be respiratory. If the PaCO2 is normal or does not explain the abnormality in pH, look at the base deficit / base excess.
If the PaCO2 is normal or does not explain the abnormality in pH, look at the base deficit / base excess. If the base deficit / base excess is consistent with the abnormality in pH then the primary abnormality is metabolic.
If the base deficit / base excess is consistent with the abnormality in pH then the primary abnormality is metabolic. If both the PaCO2 and the base excess/base deficit are both altered in a way that is consistent with the abnormality in pH then a mixed picture is present.
If both the PaCO2 and the base excess/base deficit are both altered in a way that is consistent with the abnormality in pH then a mixed picture is present. If the PaCO2 and base excess / deficit are both altered in such a way that one is consistent with the change in pH and the other is not, then it is likely that a compensated acidosis / alkalosis is present (see descriptions below).
If the PaCO2 and base excess / deficit are both altered in such a way that one is consistent with the change in pH and the other is not, then it is likely that a compensated acidosis / alkalosis is present (see descriptions below).A number of patterns of disturbance of acid–base balance are recognized.
Respiratory acidosis
Hypoventilation from any cause results in accumulation of CO2 and respiratory acidosis. Over time, the bicarbonate concentration may rise (base excess) in an attempt to balance this and a compensated respiratory acidosis may develop, in which the pH is nearly normal.
DEFINITIONS OF RESPIRATORY FAILURE
Type 1 (hypoxic) respiratory failure
PaO2 < 8 kPa with normal or low PaCO2
Type 1 respiratory failure is caused by disease processes that directly impair alveolar function, e.g. pneumonia, pulmonary oedema, adult respiratory distress syndrome (ARDS) and fibrosing alveolitis. Progressive hypoxaemia is accompanied initially by hyperventilation. The physiological benefit of hyperventilation is that it lowers alveolar carbon dioxide tension and allows for a modest increase in alveolar oxygen concentration, as can be demonstrated from the alveolar gas equation:
Type 2 (hypercapnic) respiratory failure
PaO2 < 8 kPa and PaCO2 > 8 kPa
(in absence of metabolic acidosis)
Quantifying the degree of hypoxia
The definitions above relate to patients breathing air at normal atmospheric pressure. When interpreting blood gases the inspired oxygen concentration (FiO2) must be known. Clearly a patient who is already receiving significant oxygen therapy and still has poor PaO2 is considerably worse than a patient with the same PaO2 on air. For this reason, PaO2/FiO2 ratio, alveolar–arterial (A–a) gradient, and shunt fraction (see below) have all been used to describe the severity of hypoxia.
Normal and abnormal values for PaO2/FiO2 ratio, A–a gradient and shunt fraction are shown in Table 5.2.
TABLE 5.2 Measures of hypoxia in respiratory failure
| Normal | Severe hypoxia | |
|---|---|---|
| PaO2/FiO2 ratio | >40 kPa | <27 kPa |
| A–a gradient* | <26 kPa | &45 kPa |
| Shunt fraction | 0–8% | >30% |
MANAGEMENT OF RESPIRATORY FAILURE
Common causes of respiratory failure are listed in Table 5.3.
TABLE 5.3 Common causes of respiratory failure
| Loss of respiratory drive | CVA/brain injury Metabolic encephalopathy Effects of drugs |
| Neuropathy and neuromuscular conditions | Critical illness neuropathy Spinal cord injury Phrenic nerve injury Guillain–Barré syndrome Myasthenia gravis |
| Chest wall abnormality | Trauma Scoliosis |
| Airway obstruction | Foreign body Tumour Infection Sleep apnoea |
| Lung pathology | Asthma Pneumonia COPD Acute and chronic fibrosing conditions ALI/ARDS |
 Is the patient using accessory muscles of respiration and making adequate respiratory effort, or exhausted with minimal respiratory effort? Is there an adequate cough?
Is the patient using accessory muscles of respiration and making adequate respiratory effort, or exhausted with minimal respiratory effort? Is there an adequate cough? If possible, take a history. If the patient is too short of breath to talk, the history may be obtained from the notes, staff or relatives. Try to obtain some idea of the patient’s normal respiratory reserve. How far can the patient walk? Are they oxygen dependent? Can they leave the house?
If possible, take a history. If the patient is too short of breath to talk, the history may be obtained from the notes, staff or relatives. Try to obtain some idea of the patient’s normal respiratory reserve. How far can the patient walk? Are they oxygen dependent? Can they leave the house? Examine the patient, particularly the cardiovascular and respiratory systems, bearing in mind the causes of respiratory failure. Note:
Examine the patient, particularly the cardiovascular and respiratory systems, bearing in mind the causes of respiratory failure. Note: If there is wheeze, peak flow measurement may help to document severity but is often unrecordable in the critically ill.
If there is wheeze, peak flow measurement may help to document severity but is often unrecordable in the critically ill.Management is based around correction of hypoxia, ventilatory support if required, and treatment of the underlying condition.
Hypoxaemia
Hypoxaemia is the primary concern and should be corrected:
 If there is evidence of chronic CO2 retention, (raised bicarbonate on blood gas) give controlled oxygen therapy 24–28%, via a Venturi system. While it may be appropriate to give higher oxygen concentrations this should only be done in a controlled environment where advanced respiratory support and close observation are available (see COPD, p. 152).
If there is evidence of chronic CO2 retention, (raised bicarbonate on blood gas) give controlled oxygen therapy 24–28%, via a Venturi system. While it may be appropriate to give higher oxygen concentrations this should only be done in a controlled environment where advanced respiratory support and close observation are available (see COPD, p. 152). In all other cases, give high flow oxygen via a face mask, preferably via a humidified system. Higher inspired oxygen can be achieved with a reservoir mask (plastic bag attached to mask acts as an oxygen reservoir)
In all other cases, give high flow oxygen via a face mask, preferably via a humidified system. Higher inspired oxygen can be achieved with a reservoir mask (plastic bag attached to mask acts as an oxygen reservoir)Treatment of the underlying condition
 Bronchodilators. If there is wheeze, nebulized salbutamol may help. In more severe cases consider intravenous bronchodilators and steroids (see Asthma, p. 149).
Bronchodilators. If there is wheeze, nebulized salbutamol may help. In more severe cases consider intravenous bronchodilators and steroids (see Asthma, p. 149). Physiotherapy may help clear secretions and re-expand areas of collapse. If possible sit patients upright or in a chair.
Physiotherapy may help clear secretions and re-expand areas of collapse. If possible sit patients upright or in a chair. Antibiotic therapy is best directed on the basis of Gram stains of sputum and on subsequent culture results. Seek microbiological advice. In the first instance broad-spectrum cover, e.g. with a cephalosporin is reasonable. A macrolide antibiotic such as clarithromycin should be added if there is a possibility of an atypical chest infection (see Pneumonia, p. 141).
Antibiotic therapy is best directed on the basis of Gram stains of sputum and on subsequent culture results. Seek microbiological advice. In the first instance broad-spectrum cover, e.g. with a cephalosporin is reasonable. A macrolide antibiotic such as clarithromycin should be added if there is a possibility of an atypical chest infection (see Pneumonia, p. 141). Diuretics. If there is evidence of congestive cardiac failure and pulmonary oedema, then diuretics may help. Frusemide (furosemide) 40 mg or bumetanide 1–2 mg i.v.
Diuretics. If there is evidence of congestive cardiac failure and pulmonary oedema, then diuretics may help. Frusemide (furosemide) 40 mg or bumetanide 1–2 mg i.v. Intravenous or nebulized steroids, nebulized adrenaline and helium oxygen mix may be of value in upper airway obstruction.
Intravenous or nebulized steroids, nebulized adrenaline and helium oxygen mix may be of value in upper airway obstruction.Continually reassess response to treatment. If there is no improvement or if the patient’s condition worsens, tracheal intubation and assisted ventilation may become necessary. Possible indications for intervention are shown in Box 5.1.
CONTINUOUS POSITIVE AIRWAY PRESSURE (CPAP)
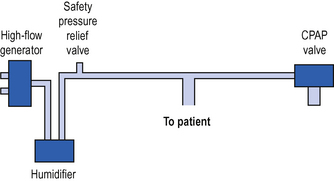
Continuous positive airway pressure (CPAP) is a system for spontaneously breathing patients which is analogous to PEEP in ventilated patients (see p. 126). It may be provided either through a tight-fitting face mask or via connection to an endotracheal / tracheostomy tube. Newly developed full hood systems are useful for the claustrophobic / confused patient. A high gas flow (which must be greater than the patient’s peak inspiratory flow rate) is generated in the breathing system. A valve on the expiratory port ensures that pressure in the system, and the patient’s airways, never falls below the set level. This is usually +5 to +10 cm H2O (Fig. 5.1).
The application of CPAP has a number of effects:
 Increased functional residual capacity (FRC) allows the lung to function on a more favourable part of the compliance curve and may therefore reduce the work of breathing.
Increased functional residual capacity (FRC) allows the lung to function on a more favourable part of the compliance curve and may therefore reduce the work of breathing.NON-INVASIVE POSITIVE PRESSURE VENTILATION
Biphasic positive airways pressure (BIPAP)
The most commonly used form of NIPPV is biphasic positive airway pressure (BIPAP). A high flow of gas is delivered to the airway via a tight fitting face or nasal mask, to create a positive pressure (see CPAP above). The ventilator alternates between higher inspiratory and lower expiratory pressures. The higher inspiratory pressure augments the patient’s own respiratory effort and increases tidal volume, while the lower expiratory pressure is analogous to CPAP / PEEP. Typical initial settings are shown in Table 5.4.
TABLE 5.4 Typical initial settings for BIPAP non-invasive ventilation
| Inspiratory pressure (IPAP) | 10–12 cm H2O |
| Expiratory pressure (EPAP) | 4–5 cm H2O |
| Inspiratory time (It) | 1–2 s |
| FiO2 | As required to maintain oxygen saturation |
Once established, the inspiratory pressure and inspiratory time can be adjusted to create the optimal ventilatory pattern for the patient.
INVASIVE VENTILATION
Volume controlled ventilation
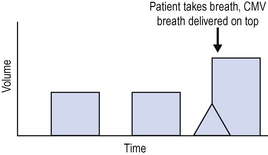
The simplest form of volume controlled ventilation is controlled mandatory ventilation (CMV) (Fig. 5.2).
The patient is ventilated at a preset tidal volume and rate (for example, tidal volume 500 mL and rate 12 breaths/min). The tidal volume delivered is therefore predetermined and the peak pressure required to deliver this volume varies depending upon other ventilator settings and the patient’s pulmonary compliance. One disadvantage, therefore, of volume controlled modes of ventilation is that high peak airway pressures may result and this can lead to lung damage or barotrauma.
Pressure controlled ventilation
It is important when using pressure controlled ventilation to understand the relationship between rate, inspiratory time and the I:E ratio (ratio of inspiratory time to expiratory time). Rate determines the total time period for each breath (60 s divided by rate = duration in seconds for each breath). The I:E ratio then determines how this time is apportioned between inspiration and expiration.
If respiratory rate is 10/min, total time for breath 60/10 s = 6 s.
If I:E ratio 1:2, then inspiratory time = 2 s and expiratory time = 4 s.
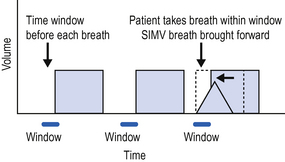
Synchronized intermittent mandatory ventilation (SIMV)
Although historically a volume controlled mode of ventilation, the equivalent of SIMV is now available in both volume controlled and pressure controlled modes (Fig. 5.3). Immediately before each breath there is a small time window during which the ventilator can recognize a spontaneous breath and respond by delivering the set (SIMV) breath early.
Pressure support / assisted spontaneous breathing (ASB)
Breathing through a ventilator can be difficult because respiratory muscles may be weak and ventilator circuits and tracheal tubes provide significant resistance to breathing. These problems can be minimized by the provision of pressure support. The ventilator senses a spontaneous breath and augments it by addition of positive pressure. This reduces the patient’s work of breathing and helps to augment the tidal volume. Pressure support modes are available on all modern ventilators and can be used in conjunction with both volume and pressure controlled modes of ventilation.
Triggering
Both SIMV and pressure support modes of ventilation require the ventilator to be able to detect the patient’s own respiratory effort in order to trigger the appropriate ventilator response. Historically triggering was achieved by detection of pressure changes in the circuit. There was no gas flow in the breathing circuit between ventilator delivered breaths and the patient’s inspiratory effort was detected as a drop in pressure in the breathing circuit. This was an inefficient method of triggering which was uncomfortable and exhausting for patients. Modern ventilators rely on flow triggering. There is a constant low level of gas flow in the circuit at all times. Flow sensors detect small changes in flow in the circuit in response to spontaneous respiratory effort by the patient, triggering the appropriate ventilator response. This is a more efficient and comfortable method of triggering.
VENTILATION STRATEGY AND VENTILATOR SETTINGS
Ventilation strategy
In most patients an SIMV volume controlled mode of ventilation with added pressure support will be adequate. Typical initial ventilator settings for an adult are as shown in Table 5.5.
TABLE 5.5 Typical ventilator settings (SIMV, volume control and pressure support)
| Tidal volume | 6–10 mL/kg |
| Rate | 8–14 breaths/min |
| I:E ratio | 1:2 |
| PEEP | 5–10 cm H2O |
| Pressure support | 15–20 cm H2O |
| FiO2 | As required to maintain oxygenation |
Pressure controlled ventilation can be used for all patients, although it is frequently reserved for those with poor pulmonary compliance (see ALI, p. 154). Typical initial settings are as shown in Table 5.6.
TABLE 5.6 Typical ventilator settings (SIMV, pressure control and pressure support)
| Peak inspiratory pressure | 20–35 cm H2O |
| Rate | 8–14 breaths/min |
| Inspiratory time | 1.5–2 s |
| PEEP | 5–10 cm H2O |
| Pressure support | 15–20 cm H2O |
| FiO2 | As required to maintain oxygenation |
CARE OF THE VENTILATED PATIENT
Ventilator care bundles
The ventilator care bundle is designed to reduce the incidence of ventilator associated pneumonia and other complications with their attendant prolongation of intensive care unit stay and increased mortality (NICE National patient safety agency. Technical patient safety solutions for ventilator-associated pneumonia in adults 2008. www.nice.org.uk/guidelines). The elements of the ventilator care bundle are:
In addition, a number of other factors are important in the ventilated patient.
Monitoring
 Tidal volume and minute volume delivered and expired. A discrepancy between the two indicates a leak in the circuit.
Tidal volume and minute volume delivered and expired. A discrepancy between the two indicates a leak in the circuit. Peak airway pressure. If the peak airway pressure does not reach a predetermined value, the breathing circuit may have become disconnected. If the peak pressure is too high this may indicate obstruction of the airway or breathing circuit, or poor compliance. The patient may be at risk of barotrauma.
Peak airway pressure. If the peak airway pressure does not reach a predetermined value, the breathing circuit may have become disconnected. If the peak pressure is too high this may indicate obstruction of the airway or breathing circuit, or poor compliance. The patient may be at risk of barotrauma.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





 When looking at a compensated acid / base disturbance remember that the compensatory mechanisms are never sufficient to completely return the pH to normal. Therefore if the pH is acidotic ( < 7.4) the underlying problem is acidosis, if the pH is alkalotic ( > 7.4) the underlying problem is alkalosis.
When looking at a compensated acid / base disturbance remember that the compensatory mechanisms are never sufficient to completely return the pH to normal. Therefore if the pH is acidotic ( < 7.4) the underlying problem is acidosis, if the pH is alkalotic ( > 7.4) the underlying problem is alkalosis.

















 Sudden loss of ETCO2 indicates either failure of ventilation (e.g. obstruction of the endotracheal tube / disconnection of the breathing circuit) or loss of cardiac output.
Sudden loss of ETCO2 indicates either failure of ventilation (e.g. obstruction of the endotracheal tube / disconnection of the breathing circuit) or loss of cardiac output.
