Immediate Management of Life-Threatening Problems
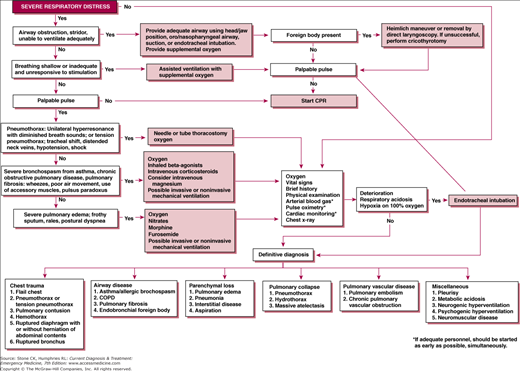
Patients in severe respiratory distress should receive simultaneous evaluation and therapy (see Figure 13–1). Providing and maintaining an adequate airway is the first consideration. Quickly assess the severity of distress by noting the patient’s general appearance. Patients struggling to breathe demonstrate a greater use of chest and accessory muscles than the normal quiet use of the diaphragm. Any patient with severe respiratory distress should receive immediate oxygen supplementation during assessment and treatment. Rapidly perform a focused examination of the oropharynx, neck, lungs, heart, chest, and extremities. A plain film chest X-ray (CXR) with PA and lateral views, if possible, provides valuable information and should be obtained as soon as possible.
Bedside pulse oximeters measure the percent saturation of oxygen in capillary blood. Pulse oximetry is particularly useful during procedural sedation and during attempts at endotracheal intubation because of the real-time availability of the information. However, this information is incomplete because pulse oximeters do not measure the pCO2 or detect the presence of hypoventilation leading to respiratory acidosis.
Arterial blood gases provide, in essence, the same information about arterial oxygen saturation as does pulse oximetry, but are necessary to provide valuable information about the effectiveness of ventilation. The blood gas provides measurement of pH, pO2, and pCO2. Arterial blood gases should be obtained in patients who are in severe respiratory distress, especially if pulse oximetry identifies that they require high concentrations of oxygen.
In unresponsive patients, check for airway patency and properly position the head and jaw to open the airway (Chapter 9). Evaluate respiratory effort and assist ventilations if inadequate. Ventricular fibrillation results in rapid loss of consciousness usually within 5–10 seconds. Such patients usually become apneic but may have perfunctory respiratory effort while unconscious. Such agonal breathing will be shallow and ineffective. It is important to recognize the situation as a primary cardiac event. The treatment is immediate defibrillation.
Basic and advanced life support is covered in Chapter 9.
See also Chapter 10.
Unless the patient has progressed to apnea unwitnessed, high-grade upper airway obstruction is usually obvious from pronounced stridorous respirations. Retractions of the supraclavicular and suprasternal areas of the chest indicate that there is significant obstruction. Patients with complete airway obstruction will not be able to breathe or speak. Patients may have a visible swelling or mass in the neck. The tongue may be swollen, as may other structures in the mouth. Laryngoscopy may reveal a foreign body, tumor, or other obstruction in the larynx or trachea.
(See also Chapter 9). Upper airway obstruction is most often due to soft tissue swelling secondary to infection or angioedema. Therapy should be directed to reduce the edema either by cooling or by vasoconstriction and treating the underlying infection or allergy. Epinephrine, either topically, by inhalation, or parentally, is the most effective medication for angioedema but caution should be exercised because of the associated cardiovascular effects. Direct laryngoscopy coupled with the use of forceps is the best method of removing obstructing foreign bodies. Obstructing liquids and particulate matter can be removed with a rigid suction device with a blunt tip (Yankauer). Foreign bodies such as meat may be removed by the Heimlich maneuver. A physician skilled in difficult airway management should care for these patients and may use adjuncts such as fiberoptic intubating bronchoscopy for diagnosis or securing the airway. If less invasive methods fail, immediate cricothyrotomy or tracheostomy is required (Chapter 7).
Patients with easy, uncomplicated removal of an obstructing foreign body may be sent home following a period of observation with instructions to eat more slowly, chew more thoroughly, and swallow more carefully. Patients who have lost consciousness but otherwise appear well should be examined and observed in the emergency department and hospitalized only if symptoms develop or persist. Some patients will have aspirated some material into the lungs, and hospitalization is appropriate if significant aspiration is suspected.
Altered mental status in a patient with obvious respiratory distress may be due to carbon dioxide retention or profound tissue hypoxia. However, the patient may have unlabored shallow respirations. Absence of a gag reflex (unprotected airway) or severe hypercapnia or hypoxemia on arterial blood gas studies (ie, respiratory failure) together with clinical assessment of underlying causes of altered mental status support the necessity for endotracheal intubation in the emergency department.
Ventilatory support should be given until endotracheal intubation can be accomplished. Provide high-flow (10–15 L/min) supplemental oxygen by nonrebreather mask or bag-valve-mask ventilation, as indicated.
As soon as oxygenation and carbon dioxide exchange have been partially corrected by assisted ventilation, the patient should be intubated. An endotracheal tube provides a definitive airway by preventing aspiration and facilitating effective respiratory support. If there is doubt about the need for intubation, err on the side of intubation. Evaluation and treatment of other causes of altered mental status should follow airway management (Chapters 17, 18, 19, and 20 and 37).
Hospitalize these patients for further diagnosis and treatment.
Tension pneumothorax may develop as a result of trauma or may occur during positive pressure ventilation. Spontaneous pneumothorax (SP) rarely produces a tension pneumothorax. Specific physical signs of tension pneumothorax include shift of the trachea to the contralateral side, and distended neck veins. Often these signs are difficult to appreciate, especially during a tense and sometimes chaotic trauma resuscitation. Clinical suspicion is the key to the diagnosis.
Provide supplemental oxygen 100% by mask. Tube thoracostomy (Chapter 7) is the definitive treatment. Needle decompression should be rarely, if ever, be required. Tube thoracostomy can be justified by clinical examination without a CXR and is usually preferable to needle decompression. If a delay in performing tube thoracostomy is unavoidable and the patient is in severe distress, a large-bore (14–16-guage) needle may be placed through the second intercostal space in the midclavicular line. A rush of air verifies successful decompression of the hemithorax. Follow needle decompression with tube thoracostomy when the situation permits.
Hospitalize these patients for further treatment.
If the patient with severe respiratory distress has vomitus with particulate matter in the oropharynx, significant aspiration is likely. Aspiration may be observed sometimes during airway procedures. Vomitus, tube feedings, or particulate food particles may be observed in the oropharynx or suctioned from the airway. Following such an episode, the patient with aspiration will typically become hypoxic with tachypnea and respiratory distress. Fever and tachycardia frequently occur. Hypotension may develop. An infiltrate, sometimes extensive, usually appears on CXR especially in the dependent areas of the lungs. Aspiration pneumonia is a common cause of respiratory morbidity and mortality in elderly and debilitated patients.
The airway should be suctioned to clear the aspirated material. Administer oxygen to correct hypoxia. Chemical pneumonitis resulting from aspiration does not require antibiotics but there is usually such difficulty in distinguishing aspiration pneumonitis from bacterial pneumonia that most clinicians begin treatment with broad-spectrum antibiotics. Corticosteroids have no proven value in the treatment of aspiration pneumonia and, in fact, may be deleterious.
Hospitalize these patients for definitive treatment.
See also Chapters 33 & 35.
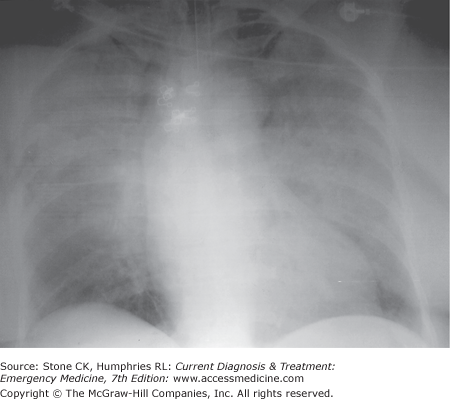
Patients with acute pulmonary edema present with severe dyspnea and labored breathing. This may be the presenting manifestation of cardiac disease, may represent decompensation of previously managed congestive heart failure (CHF), or be noncardiac in origin. Most patients have rales at the base of both lungs but in some cases, all one can appreciate is wheezing, prolonged expiration, and diminished breath sounds. Most of these patients are elderly or have known cardiac disease such as cardiomyopathy, coronary artery, or valvular heart disease. Jugular venous distension and lower extremity edema are unreliable predictors of the presence and severity of pulmonary congestion. The CXR will usually demonstrate interstitial (Figure 13–2) and sometimes alveolar edema. The work of breathing is greatly increased when the lungs are congested and edematous. Varying degrees of hypoxia are usually present. Brain natriuretic peptide (BNP) testing is helpful, especially in differentiating CHF from COPD. A level of greater than 100 pg/dL is consistent with acute decompensated heart failure. The level of BNP correlates with the severity of CHF.
Patients should be treated with 100% oxygen by a nonrebreather mask. Furosemide should be given with the initial dose of 40 mg. Doses of 80–160 mg should be used if the patient already takes diuretics or has renal insufficiency. Severe hypertension is usually present and is responsible for much of the reduced cardiac output and high left atrial pressure. Reducing it rapidly is a priority. Nitroglycerin by intravenous infusion is the best choice of a vasodilator in this setting starting at 5–10 μg/min. A higher dose may be used if the blood pressure is very high. Sublingual nitroglycerin should be used prior to establishing the infusion.
Angiotensin-converting enzyme inhibitors are important in the long-term management of heart failure but their role in the acutely decompensated patient is yet unclear. β blockers are useful in the long-term management of CHF but are best avoided in the acutely decompensated patient. Bilevel positive airway pressure (BiPAP) with an expiratory level of 5 cm H2O and an inspiratory level of 15 cm H2O is most commonly used to provide noninvasive ventilatory support and my obviate the need for endotracheal intubation.
Many of these patients are severely ill on presentation but improve dramatically with treatment. Most will still need to be hospitalized. The presence of chest pain, hypotension, or arrhythmia increases the risk of complications. Some patients with mild exacerbations of CHF that are referable to an easily reversible cause, such as medication noncompliance, may be discharged if they respond well to treatment.
See also Chapter 33.
Patients with asthma or chronic obstructive pulmonary disease may present with severe dyspnea and respiratory distress. However, dyspnea in this group of patients is less likely to be postural and cough is more common and troublesome. Patients with asthma or chronic obstructive pulmonary disease usually have wheezing on auscultation of the chest. Also common are tachypnea, tachycardia, cyanosis, chest hyperexpansion, and globally diminished breath sounds. Severe episodes are characterized by inability to speak in full sentences, oxygen saturations < 92%, use of accessory muscles, pulsus paradoxus, confusion, and a quiet chest on auscultation. CXR shows only hyperexpanded lung fields unless another pathologic process such as bacterial pneumonia is present. These patients frequently have viral or (rarely) bacterial tracheobronchitis, or exposure to an allergen has exacerbated their chronic underlying disease. Peak expiratory flow rate is the most practical objective test of airway obstruction and the response to treatment available.
Give oxygen, 1–3 L/min, to raise arterial saturation to at least 95% or Po2 to between 60 and 80 mm Hg without causing respiratory depression and a marked increase in arterial pCO2. Pulse oximetry is preferred, but arterial blood gas analysis may be indicated to help direct therapy. Noninvasive ventilation may be attempted to avoid tracheal intubation and mechanical ventilation. However, intubation may be necessary if a patient is in acute respiratory failure.
In adults, β-adrenergic sympathomimetic bronchodilators should be given in aerosol form if possible; otherwise, they may be given parenterally. A typical regimen is albuterol, 0.2–0.3 mL in 3 mL normal saline, delivered by nebulizer every 20–30 minutes. β-agonists may be nebulized in combination with ipratropium bromide (0.5 mg, up to three doses). For patients who are able to use them properly, metered-dose inhalers are as efficacious as nebulized therapy.
In general, parenteral therapy offers little benefit over nebulization, except in the most extreme cases. If used, parenteral therapy includes epinephrine, 0.2–0.3 mL (1:1000 dilution) every 20–30 minutes subcutaneously, or terbutaline, 0.25 mg subcutaneously every 2–4 hours. Parenteral therapy may have value in younger patients with severe exacerbation. However, parenteral administration of sympathomimetics can produce marked tachycardia and may induce myocardial ischemia, especially in elderly patients or those with preexisting coronary artery disease. Therefore, they should be used cautiously in this group and be withheld if chest pain or extreme tachycardia develops.
Corticosteroids should be given early to patients who do not respond adequately to nebulized or parenteral β-adrenergic agents. The recommended regimen is methylprednisolone, 125 mg intravenously initially, or prednisone, 60 mg orally. If the patient is to be discharged from the emergency department, a short course of oral steroids may be considered.
Magnesium sulfate has a bronchodialiting effect that may be of benefit in asthma. Its use should be reserved for life-threatening bronchospasm, which is refractory to all other interventions. Adult dosing of magnesium sulfate is 1–2 g intravenously over 15–30 minutes; pediatric dosage is 40 mg/kg intravenously. Effects are short-lived after the infusion is discontinued. Blood pressure should be monitored and the infusion stopped if hypotension occurs. Intravenous calcium should be immediately available to counteract cardiac dysrhythmias related to magnesium. Deep tendon reflexes will be lost once serum magnesium concentration reaches 7–10 mEq/L (normal concentration is 1.5–2.0 mEq/L); the infusion should be stopped if reflexes are lost. At higher concentrations, respiratory depression and cardiac arrest may occur. However, the dose used for asthma is relatively low (approximately one-fourth the dose used in preeclampsia).
Hospitalize patients with significant bronchospasm that does not respond promptly to treatment, or those with moderate bronchospasm that fails to improve after several hours of treatment.
Further management of patients with these disorders is discussed in Chapter 33.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree