Chapter Two Research supporting massage for pain management
Chapter contents
Introduction
This chapter will focus on understanding and justifying massage as a treatment approach for pain management. Current research will be analyzed to support the premise that massage is a valuable intervention for pain management.
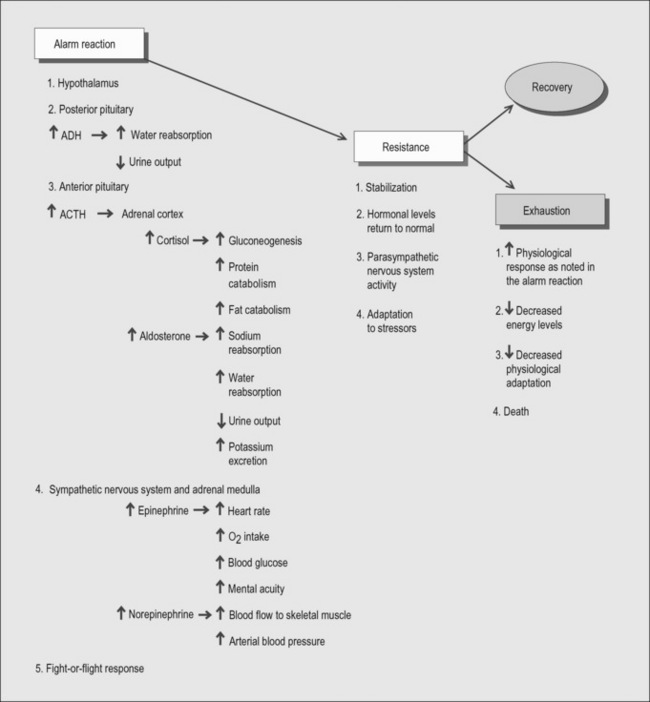
In review of Chapter 1, pain is usually described as acute or short term and as chronic or long term. Acute pain arises from sudden injury to the structures of the body (e.g. skin, muscles, viscera). The intensity of pain is usually proportional to the extent of tissue damage. The sympathetic nervous system is activated, resulting in an increase in the heart rate, pulse, respirations, and blood pressure. This also causes nausea, diaphoresis, dilated pupils, and elevated glucose. Continuing or persistent pain results from ongoing tissue damage or from chemicals released by the surrounding cells during the initial trauma (e.g. a crushing injury). The intensity diminishes as the stimulus is removed or tissue repair and healing take place. Acute pain serves an important protective physiologic purpose that warns of potential or actual tissue damage. Chronic pain has slower onset and lasts longer than 3 months beyond the healing process. Chronic pain does not relate to an injury or provide physiologic value. Depending upon the underlying etiology, it is often subdivided into malignant (cancer) or nonmalignant (causes other than cancer) pain. It may arise from visceral organs, muscular and connective tissue, or neurologic causes such as diabetic neuropathy, trigeminal neuralgia, or amputation. As chronic pain progresses, especially poorly treated pain, other physical and emotional factors come into play affecting almost every aspect of a patient’s life – physical, mental, social, financial, and spiritual – causing additional stress, anger, chronic fatigue, and depression. Whereas pain has always been viewed as a symptom of a disease or a condition, chronic pain and its harmful physiologic effects are being looked upon as a disease itself.
As presented in Chapter 1, pain is caused by the stimulation of nociceptors. These receptors are usually stimulated by chemicals such as substance P, bradykinin, and histamine, which excite the nerve endings. Pain is elicited by three different classes of stimuli: mechanical, chemical, and thermal. Soft tissue pain is caused by the chemicals released from illness, injury, or from mechanical irritation caused by cumulative stress, microinflammation, or extreme heat or cold. Emotional or psychological stress, called autonomic disturbances, can cause pain by causing hypertonic muscles and shifts in fluid flow affecting oxygen and nutrient delivery and waste removal.
How does massage work?
Treatment modalities in interdisciplinary pain management may include:
1. Education in pain mechanisms, physiology, and psychological aspects of pain.
2. Psychological interventions targeting cognitive and behavioral aspects of adaptation to pain and the relation between chronic pain and the effects of prolonged stress.
3. Physiotherapy with the principal goal of enhancing overall physical functioning and reducing musculoskeletal impairment caused by the pain experience. Pain mechanisms underlying chronic pain conditions include physical and emotional trauma, illness and deconditioning.
4. Pharmacological treatment to minimize symptoms and problems associated with pain. See: http://www.iasp-pain.org/AM/AMTemplate.cfm?Section=Home&TEMPLATE=/CM/ContentDisplay.cfm&CONTENTID=7626
Massage therapy needs to function to interface with one or more of these four points.
The most commonly used complementary modalities in the research are:
• Removal or reduction in the stress load to which the local tissues (or the body as a whole) is adapting.
• Improvement in the way(s) the local tissues (or the body as whole) is coping and adapting.
• Symptomatic treatment to make the recovery period more comfortable – without adding to the adaptive load.
• Sometimes all three elements can be achieved, sometimes only one.
What research shows us
Research is mixed for the efficacy of massage for pain. Generally massage for pain management was not found to be a definitive treatment on its own but was supportive of many other interventions either enhancing effects or managing side effects of other treatments. Massage was found to be generally safe. Some benefits of massage related to other conditions such as low back or neck pain can be logically applied to pain in general. Other researchers have looked at massage for pain in general and others delved into the general benefits of massage.
Massage benefits and safety in general
When looking at any treatment, safety is a primary concern, i.e. do no harm. If harm is possible, then the benefits of receiving massage must exceed the potential for harm. A summary of a review of massage safety by Ernst (2006) concludes that massage is generally safe (Box 2.1). Massage is not entirely risk free. However, serious adverse effects are rare. The majority of adverse effects from massage were associated with aggressive types of manual massage or massage delivered by untrained individuals. Serious adverse effects were associated mostly with massage techniques other than ‘Swedish’(classic) massage.
Box 2.1 Who is Edzard Ernst?
Professor Ernst qualified as a physician in Germany in 1978 where he also completed his MD and PhD theses. He has received training in acupuncture, autogenic training, herbalism, homoeopathy, massage therapy, and spinal manipulation. He was Professor in Physical Medicine and Rehabilitation (PMR) at Hannover Medical School and Head of the PMR Department at the University of Vienna. In 1993 he established the Chair in Complementary Medicine at the University of Exeter. He is founder/Editor-in-Chief of two medical journals (Perfusion and FACT). He has published more than 40 books and in excess of 1000 articles in the peer-reviewed medical literature and has been given visiting professorships in Canada and the USA. His work has been awarded with 13 scientific prizes. In 1999 he took British nationality. His unit’s research is funded from two endowments by the late Sir Maurice Laing, by research grants and fellowships (not, however, by ‘Big Pharma’ as sometimes speculated). See: http://sites.pcmd.ac.uk/compmed/ernst.htm
Contact: Complementary Medicine, Peninsula Medical School, Universities of Exeter and Plymouth, Exeter, UK. Edzard.Ernst@pms.ac.uk
Information provided by Moyer and others (2006) indicates that massage is effective as a treatment in some instances but they did not investigate why. The ‘why massage works’ remains elusive but there are reoccurring findings indicating possible physiologic mechanisms for massage benefit. One study by Field and her associates (2005) is particularly relevant for the topic of this text since it deals with serotonin, which is associated with the body pain modulation mechanisms. In the other studies (2004) Diego speaks of how massage needs to be applied with sufficient compressive force to stimulate antiarousal response and that massage that is considered light can be arousing (Moyer 2006).
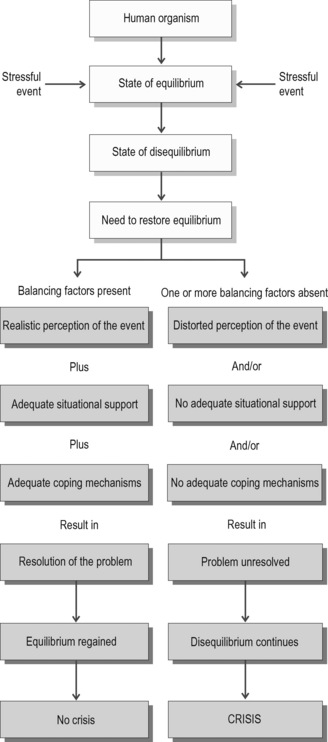
Massage therapy appears to affect anxiety levels (Fig. 2.1). The therapeutic relationship established between massage therapist and client is similar to psychotherapy: a treatment that relies on communication and therapeutic relationship to provide effects. It is possible that massage effects related to the affective category are related to the therapeutic relationship (Fellowes 2004, Moyer 2006). As described it is common to find a correlation between stress, anxiety, depression, and pain. According to Hanley et al (2003) despite very strong patient preference for therapeutic massage, it did not show any benefits over either a relaxation tape used in the surgery or a relaxation tape used at home. This study indicates that massage is effective but no more effective than other relaxation interventions.
A key is that people liked massage, which is important in compliance with treatment. Muller-Oerlinghausen et al (2004) concluded that slow-stroke massage is suitable for adjuvant intervention for depression and is readily accepted by very ill patients. Currin and Meister (2008) found that reduction in oncology patient distress was observed regardless of gender, age, ethnicity, or cancer type and therefore supported massage therapy for hospitalized oncology patients as a means of enhancing their course of treatment. Sturgeon et al (2009) found that therapeutic massage shows potential benefits for reducing breast cancer treatment side effects of chemotherapy and radiation and improving perceived quality of life and overall functioning.
Box 2.2 Factors influencing the response to stressors
(From Potter & Perry 2005).
Mechanical effects related to massage benefits
Massage benefits appear to be related to mechanical forces applied to soft tissue which:
• alter pliability in connective tissue
• stimulate neuro signaling in fascia
• create changes in circulation
Let’s look at each of these areas. As presented later in this text, massage methods apply mechanical forces to the soft tissue. According to Langevin and Sherman (2007) pain related fear leads to a cycle of decreased movement, connective tissue remodeling, inflammation and nervous system sensitization which combine into a cycle resulting in further decreased mobility. The mechanisms of a variety of treatments such as massage may reverse these abnormalities by applying mechanical forces to soft tissues. Based on a tensegrity principle, direct or indirect connections between fascia or muscles which stretch the aponeurosis or intermuscular septum may allow the transfer of tension over long distances. Massage applied in such a way to deform the soft tissue has an effect on electrical (EMG) and mechanical (MMG) activities of a muscle lying distant, but indirectly connected to, the massaged muscle. It was concluded that there was an electrical as well as a mechanical response of muscle connected indirectly by structural elements with the muscle being massaged, indicating an application for the tensegrity principle in massage therapy and influence on adverse muscle tension by massaging another distant muscle (Kassolik et al 2009).
Day et al (2009) found that deep muscular fascia design supports the premise that the myofascial system is a three-dimensional continuum, including the epimysium and the retinacula. Dr Carla Stecco and Dr Antonio Stecco have carried out extensive research into the anatomy and histology of the fascia via dissection of unembalmed cadavers. This technique presents a complete biomechanical model that assists in deciphering the role of fascia in musculoskeletal disorders.
The mainstay of this manual technique lies in the identification of a specific, localized area of the fascia in connection with a specific limited movement. Once a limited or painful movement is identified, then a specific point on the fascia is implicated and, through the appropriate manipulation of this precise part of the fascia, movement can be restored. These dissections have enhanced the pre-existing biomechanical model already elaborated by Luigi Stecco (2004, 2009) by providing new histological and anatomical data.
While part of the fascia is anchored to bone, part is also always free to slide.
The method used in the Stecco studies involves a deep kneading of muscular fascia at specific points, termed centers of coordination (cc) and centers of fusion (cf), along myofascial sequences, diagonals, and spirals, and is called fascial manipulation technique. Visual analogue scale (VAS) measurement of pain administered prior to the first session and after the third session was compared with a follow-up evaluation at 3 months. Results suggested that the application of fascial manipulation technique may be effective in reducing pain in chronic situations (Pedrelli et al 2009).
Box 2.3 Interview of Luigi Stecco
Curing the fascia. Interview of Luigi Stecco by Massimo Ilari. Published April 2003, Vita & Salute magazine. Translation: Julie Ann Day
Recent studies suggest that cyclic stretching of fibroblasts contributes to antifibrotic processes of wound healing by reducing connective tissue growth factor (CTGF) production (Kanazawa et al 2009). Robert Schleip (2003) indicates that fascia is imbedded with sensory mechanoreceptors, making fascia a sensory organ, and free nerve endings which respond to mechanical force stimulation. The intrafascial mechanoreceptors consist of four groups:
1. Golgi organs, which are found mostly in myotendinous junctions.
2. Large Pacini corpuscles, which respond to rapid changes in pressure.
3. Smaller and more longitudinal Ruffini organs, which do not adapt quickly to pressure.
Schleip (2006) indicates soft tissue strain involves a stimulation of intrafascial mechanoreceptors. This stimulation leads to an input to the central nervous system, altering the tone of motor units associated with the tissue. Combined with Ruffini organs and interstitial receptors, it can trigger changes in the autonomic nervous system.
The European Fascia Group (Schleip et al 2006) found that when fascia is stretched there are longitudinal relaxation changes in the collagen fibers and the water is squeezed out. Fascia seems to adapt with very complex and dynamic water changes to mechanical stimuli and the matrix reacts in smooth muscle-like contraction and relaxation responses of the whole tissue due to the sponge effect of fascia, like squeezing and refilling effects in the semiliquid ground substance.
Dr Leon Chaitow (2009) indicates that key fascia related topics are:
• The presence of contractile smooth muscle cells (SMCs/myofibroblasts) that are embedded in most connective tissues. For example, SMCs have been located widely in connective tissues including cartilage, ligaments, spinal discs, and lumbodorsal fascia (Ahluwalia 2001, Hastreite et al 2001). The extracellular matrix (ECM) plays a key role in the transmission of forces generated by the organism (e.g. muscle contraction) or externally applied (e.g. gravity, or by means of manually applied therapy).
• Cell-matrix adhesion sites appear to host a ‘mechanosensory switch’ as they transmit forces from the ECM to the cytoskeleton, and vice versa, triggering internal signals following mechanical stimulation, such as occurs in manual therapy (Chen & Ingber 1999). There appear to be forms of communication within the fascial matrix, for example caused by tugging in the mucopolysaccharides, created by twisting acupuncture needles (Langevin et al 2005).
German researchers, Robert Schleip et al (2005), note that:
Several years ago Klingler and Schleip (2004) showed that the water content of fascia partially determines its stiffness, and that stretching, or compression, of fascia (as occurs during almost all manual therapies) causes water to be extruded (like a sponge) – making the tissues more pliable and supple. After a while the water is taken up again and stiffness returns, but in the meantime structures can be mobilized and stretched more effectively and comfortably than when were they still densely packed with water.
• Klingler et al measured wet and dry fresh human fascia, and found that during an isometric stretch, water is extruded, refilling during a subsequent rest period.
• As water extrudes during stretching, temporary relaxation occurs in the longitudinal arrangement of the collagen fibers.
• If the strain is moderate, and there are no micro-injuries, water soaks back into the tissue until it swells, becoming stiffer than before.
Since we already know that approximately 80% of the main trigger point sites lie on points located on the meridian maps (Wall & Melzack 1990), the conjunction of these two areas of study (TCM/acupuncture points and myofascial trigger points) should not come as a surprise. Indeed, many experts believe that trigger points and acupuncture points are the same phenomenon (Kawakita et al 2002). Whether this is so or not, it suggests that in trying to understand trigger points better, we need to pay attention to research that tries to explain the processes of acupuncture, and the structural aspects of these invisible points.
Dr Langevin and her research colleagues have helped to clarify the situation, having shown that acupuncture points, and many of the effects of acupuncture, seem to relate to the fact that most of these localized ‘points’ lie directly over areas where there is a fascial cleavage, where sheets of fascia diverge to separate, surround, and support different muscle bundles (Langevin et al 2001).
‘Loose’ connective tissue forms a network extending throughout the body including subcutaneous and interstitial connective tissues. The existence of a cellular network of fibroblasts within loose connective tissue may have considerable significance as it may support yet unknown body-wide cellular signaling systems …Our findings indicate that soft tissue fibroblasts form an extensively interconnected cellular network, suggesting they may have important, and so far unsuspected integrative functions at the level of the whole body. (Langevin et al 2004)
To understand how this signaling system works we need to be aware of the role of integrins – tiny projections emerging from each cell, that act like mini-transmitters and receivers. What Helene Langevin and her colleagues are now showing is that when deformation of cells and tissues occurs – such as that which happens to all of us when areas of the body are chronically shortened, crowded, compressed, stretched, or twisted due to age, disease, trauma, or progressive adaptation – the cells cannot function or communicate normally, or even demonstrate normal gene expression. And consider, from the bodyworker’s point of view, the reverse of that scenario. When we normalize tissues that are tense/tight/deformed/compressed by means of massage, stretching, mobilizing, etc., we are not just normalizing the biomechanical aspects of the function of those tissues – so that, for example, the shoulder or elbow or neck or whatever ‘feels’ better – we are also improving internal cellular function, enhancing cellular communication and gene expression. If that’s not a ‘wow’ I don’t know what is!
The Amazing Fascial Web, Leon Chaitow
The observation of Langevin et al (2005) is:
The dynamic, cytoskeleton-dependent responses of fibroblasts to changes in tissue length demonstrated in this study have important implications for our understanding of normal movement and posture, as well as therapies using mechanical stimulation of connective tissue including physical therapy, massage and acupuncture. (Langevin et al 2005)
1. The fascial cleavage planes seem to have a great deal to do with where acupuncture points (and many or most trigger points) are situated.
2. Cells communicate via (among other methods) mini-projections (integrins) that are capable of becoming deformed and distorted though age, overuse, misuse, abuse, and disuse (and loss of gravity!), with negative effects on cellular (and therefore tissue) function, including communication, nutrition, and reproduction (gene expression).
3. The function of tissues, down to the cellular level, can be enhanced by appropriate massage, bodywork, movement, and manipulation (and, it seems, by acupuncture).
What type of methods influence fascia?
Fischer et al (2009) confirmed the interconnectedness of body areas with a study that suggests that temporomandibular joint dysfunction plays an important role in the restriction of hip motion experienced by patients with complex regional pain syndrome, which indicated a connectedness between these two regions of the body.
Circulation is also affected by massage. Castro-Sánchez et al (2009) found that connective tissue massage improves blood circulation in the lower limbs of type 2 diabetic patients at stage I or II-a and may be useful to slow the progression of peripheral artery disease. A different study lead by Castro-Sánchez indicated that a combined program of exercise and massage improves arterial blood pressure and ankle brachial index values in type 2 diabetics with peripheral arterial disease. Walton (2008) investigated efficacy of myofascial release techniques in the treatment of primary Raynaud’s phenomenon and found that releasing restricted fascia using myofascial techniques may influence the duration and severity of the vasospastic episodes.
Arroyo-Morales et al (2008) found that massage reduces EMG amplitude and vigor when applied as a passive recovery technique after a high-intensity exercise protocol. Massage may induce a transient loss of muscle strength or a change in the muscle fiber tension–length relationship, influenced by alterations of muscle function and a psychological state of relaxation.
Research related to massage and pain
Existing research provides fairly robust support for the analgesic effects of massage for nonspecific low back pain, but only moderate support for such effects on shoulder pain and headache pain. There is only modest, preliminary support for massage in the treatment of fibromyalgia, mixed chronic pain conditions, neck pain, and carpal tunnel syndrome. Thus, research to date provides varying levels of evidence for the benefits of massage therapy (MT) for different chronic pain conditions (Tsao 2007).
Ho et al (2009) studied massage for adhesive capsulitis (AC), shoulder impingement syndrome (SIS) and nonspecific shoulder pain/dysfunction. For SIS, there was no clear evidence to suggest additional benefits of MT to other interventions. MT was not shown to be more effective than other conservative interventions for AC; however, massage and mobilizations-with-movement may be useful in comparison to no treatment for short-term outcomes for shoulder dysfunction. Massage is safe and may have clinical benefits for treating chronic neck pain at least in the short term (Sherman et al 2009). The application of a single session of manual therapy program produces an immediate increase of index heart rate variability (HRV) and a decrease in tension, anger status, and perceived pain in patients with chronic tension-type headache (CTTH), HRV, mood states, and pressure pain thresholds (PPTs) in patients with CTTH (Toro-Velasco et al 2009).
Pain relief by topic