FIGURE 75.1 Algorithm for the management of low urine output following renal transplant.
Postoperative evaluation of electrolytes should include monitoring of serum sodium, potassium, bicarbonate, calcium, magnesium, and phosphorous. Although some patients require bicarbonate supplements, potassium supplements are usually not necessary. However, supplementation may be required in patients with large-volume posttransplant diuresis.
Prophylaxis with subcutaneous heparin to prevent deep venous thrombosis and with H2 receptor blockers or proton pump inhibitors to prevent gastric and/or duodenal ulcers is often administered. Patients should be evaluated for the need for dialysis based on their electrolyte, metabolic, and volume status.
EARLY COMPLICATIONS
The most common complication early posttransplant is an inappropriately low urine output. The differential diagnosis includes obstruction of urine flow anywhere between the renal pelvis and the collection bag; graft hypoperfusion; urinary leak; renal parenchymal disease, usually ATN; and acute rejection in immunologically sensitized patients. If a brisk diuresis was observed in the operating room or has been recorded in previous hours, a sudden reduction in urine flow should immediately raise suspicion of a mechanical problem.
Frequently, blood clots obstruct the urinary catheter. The patient complains of a sense of fullness and need to urinate. “Milking” the urinary catheter tubing poses no risk of contaminating the closed system and usually dislodges the clots. If catheter irrigation is necessary, meticulously sterile technique is used. Sterile saline, 20 to 30 mL, should be instilled retrograde to facilitate mechanically breaking up the clot. Avoid overdistention of the bladder, which risks rupture of the ureteroneocystostomy or bladder closure. If irrigation fails to evacuate the clot, removal of the Foley catheter and replacement with a larger catheter (number 18 through 20 French) is recommended. If clots still accumulate, a triple-lumen urinary catheter permits continuous bladder irrigation; rarely, cystoscopy is required to evacuate clots.
Other mechanical problems include obstruction of the ureter or urine leak (17). These should always be suspected when there has been a history of brisk urine flow noted at surgery, but little or none has been noticed since bladder closure. Urine leak can present as severe wound pain, ascites, scrotal or labial edema, and fluid draining from the wound or operative drains with urea nitrogen and creatinine concentrations much higher than serum. Ultrasonography is particularly useful in diagnosing hydroureter or perinephric fluid collections (18). These problems require immediate operative correction.
After exclusion of outflow problems, factors that determine allograft perfusion should be addressed. Norms for “adequate” blood pressure are higher after transplantation, especially in children receiving adult kidneys and patients with limited cardiac contractility. To some degree, all transplanted kidneys have sustained predonation procurement and reperfusion injuries (19). There is an increase in interstitial edema and increased venocapillary resistance, endothelial swelling and denuding, and activation of vasoactive mediators. The resistance of the renal vascular bed is increased. Renal plasma flow requires a higher mean arterial pressure in this setting. The renal transplant recipient usually requires a blood pressure greater than 120/80 mmHg. The patient’s history of average pretransplant pressures is valuable in targeting perfusion pressure.
Unless there is clear evidence of intravascular volume overload, fluid boluses with normal saline are usually required. A transient response may justify further volume expansion. Most dialysis-dependent patients have total-body fluid overload. Their “dry weight,” used to calculate an end point on dialysis, is always in excess of the dry weight they reach with normal renal function. Several centers use low-dose dopamine (2.5 μg/kg/min) in an attempt to improve renal perfusion, although it is most unlikely that any increased perfusion actually occurs. In rare circumstances, the intrarenal vascular resistance may be excessively high, and adequate perfusion pressures do not produce sufficient intrarenal blood flow. This problem dramatically increases the risk of further ischemic injury or even thrombosis. Grafts from pediatric donors, especially those younger than 4 years, are prone to thrombosis. As an additional safeguard, in recipients of pediatric en bloc kidneys, low-dose aspirin therapy immediately after surgery to minimize the risk of thrombosis should be considered. Graft thrombosis is rare, but any hope of graft salvage requires immediate return to the operating room.
DELAYED GRAFT FUNCTION AND ACUTE TUBULAR NECROSIS
Delayed graft function (DGF) or acute renal dysfunction in the immediate posttransplant period has been a serious and frequent problem in cadaveric renal transplantation, occurring in up to 30% of the recipients (20), and in up to 35% to 40% in ECD and DCD kidney recipients, respectively. However, this diagnosis should be considered only after all other causes are eliminated. ATN is the most common histologic feature in patients with DGF. The risk factors associated with an increased incidence of DGF include donor hypovolemia or hypotension, particularly in the presence of nephrotoxic drugs or vasopressors; prolonged cold or warm ischemia times; kidneys procured from older donors and from donors with hypertension or vascular occlusive disease; injury incurred during procurement, preservation, or implantation; and a high (>50%) panel reactive antibody (PRA) level in the recipient (21–23). Living-donor kidneys are much less likely to have DGF than deceased donor kidneys. The pathophysiology leading to DGF is complex and incompletely understood, but appears to be due to ischemia–reperfusion injury. The short- and long-term deleterious effects on graft survival that have been demonstrated in patients developing this disorder relate to its association with acute and chronic rejection (23,24). Therefore, protocols were developed to administer antilymphocyte antibodies for the preemptive treatment of acute rejection, during this period of graft dysfunction, when a diagnosis of rejection could be difficult. This led to the development of protocols termed sequential quadruple immunosuppressive therapy, where patients receive antibody induction followed by maintenance immunosuppression, usually with three agents.
IMMUNOLOGIC CAUSES OF EARLY GRAFT DYSFUNCTION
Hyperacute rejection is a rare and largely preventable cause of immediate graft failure. It is caused by preformed antibodies present in the recipients’ serum at the time of transplantation against donor antigens. These antibodies are the consequence of previous exposure to donor antigens due to blood transfusions, prior transplantation, or pregnancy. It also occurs when transplantation is attempted across ABO-incompatible barriers. The events that lead to hyperacute rejection may occur with such rapidity that the kidney becomes visibly ischemic while the patient is still on the operating table. It always occurs within 24 hours of transplantation. Renal histology shows fibrin thrombi occluding the glomerular capillaries and small vessels with extensive tissue necrosis. Although plasmapheresis and anticoagulation have been advocated, there is no established effective treatment and interventions are seldom successful. A kidney with hyperacute rejection should always be removed promptly. The current cross-match techniques, because of their increased sensitivity, have greatly diminished the incidence of hyperacute rejection.
Antibody-mediated (C4D+) acute rejection is another form of early rejection that can occur in previously sensitized patients, but who have an initial negative cross-match. This form of acute rejection is potentially reversible if diagnosed early and treated aggressively with plasmapheresis and intravenous immunoglobulin (25). Eculizumab a humanized monoclonal antibody that specifically binds to the complement protein C5, thereby inhibiting its cleavage to C5a and C5b and preventing the generation of the terminal complement complex C5b-9 is currently in studies for the prevention of antibody mediated rejection (AMR) in renal transplant recipients. Eculizumab is approved for the treatment of patients with paroxysmal nocturnal hemoglobinuria (PNH) and another rare disease, atypical hemolytic uremic syndrome (aHUS) and currently available commercially. It is being evaluated in Phase 2 clinical studies in kidney transplant recipients for prophylaxis of AMR and also for the prevention of DGF (26). Patients receiving eculizumab may have increased susceptibility to infections, especially those with encapsulated bacteria. Life-threatening and fatal meningococcal infections have been reported. Children treated with eculizumab may also be at increased risk of developing serious infections due to Streptococcus pneumoniae and Haemophilus influenzae type b (Hib) (27).
IMMUNOSUPPRESSION
The different phases of immunosuppressive therapy after transplantation are as follows:
- Induction immunosuppression in the immediate posttransplantation period when potent therapy is required to prevent rejection.
- Maintenance immunosuppression for long-term therapy to prevent allograft rejection, but at the same time preserving host defense mechanisms against infections.
- Intensification of the immunosuppressive therapy for the treatment of an acute rejection episode.
Antilymphocyte antibodies—available as immunosuppressive agents since the late 1960s—are ideally suited for use as induction immunosuppressive agents and, to some extent, for the treatment of acute rejection. All early forms of antilymphocyte antibodies were polyclonal, made by injecting human lymphocytes into horses, goats, rabbits, or sheep. In contrast to polyclonal antibodies, a monoclonal antibody is highly specific, and recognizes a single antigen epitope. They have a greater potency at lower doses, and have a more predictable and consistent effect. Monoclonal antibodies that have been approved for use in transplantation are directed either at cell surface receptors such as the CD3/T-cell receptor (TCR) complex (OKT3), or the interleukin-2 (IL-2) receptor (IL-2R; daclizumab and basiliximab). OKT3 and daclizumab have been withdrawn and are no longer available. These immunosuppressive agents are classified as depleting-antibody or nondepleting antibody, depending on their ability to deplete lymphocytes from the peripheral circulation.
Current maintenance immunosuppression protocols often use the combination of a calcineurin inhibitor, an antimetabolite, and corticosteroids. However, the principles of the different regimens are similar: more intense immunosuppression in the induction phase with gradual reduction in immunosuppression in the maintenance phase. The immunosuppression protocol an institution implements should provide a balance between preventing rejection and avoiding the consequences of overimmunosuppression such as infection and malignancy.
Induction Agents
Depleting Antibodies
Rabbit antithymocyte globulin (thymoglobulin), a polyclonal antilymphocyte antibody, is produced by the immunization of rabbits with human thymocytes. Several mechanisms of action have been proposed to explain the immunosuppressive effect of thymoglobulin. These include complement-mediated cell lysis, clearance of lymphocytes by opsonization and subsequent phagocytosis by macrophages, and antibody-dependent cell-mediated cytolysis (28).
Polyclonal antibody treatment induces marked lymphocyte depletion that persists during the entire treatment period. The number of circulating T cells will gradually increase after the cessation of treatment and reach pretreatment levels in several weeks, with significant variability among patients. Each polyclonal antilymphocyte preparation varies in its constituent antibodies. Due to this unpredictable antibody mixture and batch-to-batch variability, treatment responses and side effects are variable between the different preparations (29).
Thymoglobulin (antithymocyte globulin) is the only polyclonal agent currently available for use in the United States. Thymoglobulin consists of antibodies specific for T-cell epitopes, including CD2, CD3, CD4, CD8, CD11a, CD18, CD25, HLA-DR, and HLA class I. An uncommon, but serious, side effect of thymoglobulin treatment is the cytokine release syndrome, which usually occurs after the administration of the first few doses. This syndrome includes the development of skin rashes, hypotension, acute respiratory distress, and anaphylaxis. Polyclonal antibodies often cross-react with antigens on unrelated cells, resulting in such side effects as granulocytopenia, thrombocytopenia, arthralgia, serum sickness, phlebitis, and immune complex glomerulonephritis. Because these agents severely impair cell-mediated immunity, patients are prone to develop opportunistic infections and posttransplantation malignancies, especially posttransplantation lymphoproliferative disorders (PTLDs).
Thymoglobulin is dosed at 1.5 mg/kg/day for a total dose of 6 mg/kg. It is administered as an IV infusion over a period of about 6 hours. Premedication is recommended using high-dose methylprednisolone, an antihistamine, and acetaminophen 1 hour prior to its administration.
Alemtuzumab (Campath-1H) is a humanized monoclonal antibody directed against the CD52 antigen (30,31); it is not approved by the Food and Drug Administration for use in kidney transplant patients but is used off-label in approximately 15% of these recipients. Targeting of CD52 with antibody has shown to be exceptionally lytic of lymphocytes. The mechanism of action of alemtuzumab includes complement-mediated lysis, cell-mediated killing (antibody-dependent cellular cytotoxicity [ADCC]), and induction of apoptosis of targeted cells. Alemtuzumab is a relatively low-affinity antibody, requiring 20 to 50 μg/mL to saturate its receptors (32). Because of the humanization of alemtuzumab, the first-dose effect is relatively mild; there is an associated tumor necrosis factor (TNF)-α and interferon-γ (IFN-γ) release that can be reduced with steroids. First infusion reactions such as fever, rash, nausea, vomiting, headache, and rigors due to a cytokine release syndrome have been reported with alemtuzumab treatment; however, these effects have been of a low-grade nature and limited with steroid pretreatment (32,33). Alemtuzumab effectively depletes immune cells, namely T and B lymphocytes, some natural killer (NK) cells, and some monocyte/macrophage lineage. Results from a number of single-center trials (34,35) and a multicenter trial (36) comparing alemtuzumab induction with that of basiliximab in low–immunologic-risk recipients and with thymoglobulin for high–immunologic-risk recipients have confirmed the efficacy of alemtuzumab as an induction agent.
Rituximab (Rituxan) antibody is a genetically engineered chimeric (human and mouse) monoclonal antibody directed against the CD20 antigen found on the surface of normal and malignant B lymphocytes (37). Rituximab is approved for the treatment of patients with relapsed or refractory, low-grade or follicular, CD20-positive, B-cell, non-Hodgkin lymphoma (38,39). Because of its effects on the B lymphocytes, rituximab is believed to be effective in the treatment of patients with antibody-mediated (humoral) acute rejection and is also thought to have a role in decreasing the PRA level in sensitized patients. However, it is not FDA approved for the latter indications and has not gained widespread support for use in transplant recipients, except for treatment in patients with PTLD (40).
Nondepleting Antibody
Basiliximab is an anti–interleukin-2α receptor antibody that is currently used as an induction agent in kidney transplant recipients that are unsensitized and are immunologically at a lower risk for acute rejection. IL-2 is a cytokine responsible for the growth and proliferation of activated T cells. During an immune response, IL-2 exerts its effects by binding to the IL-2R on the surface of the antigen-activated T cell; anti–interleukin-2α receptor antibodies are monoclonal antibodies directed against the IL-2R on activated T cells. These antibodies are used as induction agents for prophylaxis against acute rejection in renal transplant recipients (41).
Basiliximab (Simulect) is a chimeric (human and mouse) IgG1κ monoclonal antibody that is administered as an IV infusion of two doses of 20 mg each. The first dose is given within 2 hours before transplantation, and the second dose is administered 4 days after transplantation. Adverse effects of the IL-2R antibodies are minimal and equivalent to placebo in controlled trials; hypersensitivity reactions have been reported.
Maintenance Agents
Calcineurin Inhibitors
Calcineurin inhibitors are currently considered to be the mainstay of immunosuppression regimens following transplantation. They are potent immunosuppressants, inhibiting T-cell activation by inhibiting calcineurin phosphatase, a key step in the regulation of cytokine expression. The introduction of calcineurin inhibitors in the mid-1980s revolutionized the field of transplantation by dramatically reducing acute rejection rates and improving short-term allograft survival (42).
Cyclosporine A (CsA), the first calcineurin inhibitor approved for use in transplant recipients for maintenance immunosuppression, binds to cyclophilin in the T cell. The CsA/cyclophilin complex, in turn, inhibits calcineurin phosphatase, which is responsible for the transcription of IL-2. CsA is highly lipophilic and water insoluble. Early formulations (Sandimmune) were administered orally as an oil-based solution. In this form, bioavailability was erratic, highly variable, and bile dependent for its absorption. This erratic absorption profile led to the development of a microemulsion formulation (modified cyclosporine, Neoral) that demonstrated a more reliable and predictable absorption. These two formulations are not bioequivalent and are thus not interchangeable. CsA is available in an IV formulation, as an oral solution, and in a capsule form. The IV formulation should be administered as a continuous infusion and should be limited to patients unable to take CsA orally; the patient should be monitored closely during the infusion process. The CsA dosage should be titrated based on whole blood concentration; the recommended starting dose of oral solution or capsules is 10 to 14 mg/kg/day for the nonmodified CsA and 6 to 12 mg/kg/day of the modified CsA, administered 12 hours apart in divided doses. In the United States, use of CsA has been superseded by that of tacrolimus in the majority of kidney transplant recipients and in almost all pancreas transplant recipients.
Tacrolimus (Prograf, FK-506) is a macrolide agent that inhibits IL-2 production in a similar fashion as CsA in the T lymphocyte. However, instead of binding to cyclophilin, tacrolimus binds to the FK-binding protein 12 (FKBP-12), with the resulting complex inhibiting calcineurin phosphatase. Tacrolimus is available in IV injection and oral capsule dosage forms. The IV form of tacrolimus is also administered as a continuous infusion and, because of the risk of neurotoxicity, should be limited to select patients unable to take tacrolimus orally. Tacrolimus is readily absorbed in the stomach and should be given orally or through nasogastric tube whenever feasible. The recommended starting dose of oral tacrolimus is 0.2 mg/kg/day administered 12 hours apart in divided doses.
Astagraf XL is an extended-release formulation of tacrolimus capsule that is indicated for the prevention of rejection in kidney transplant recipients. It shares the same efficacy and side-effect profile as that of immediate-release tacrolimus. It provides a once-daily dosing option and, as a result, may improve compliance (43,44).
Envarsus is also an extended-release formulation of tacrolimus utilizing the proprietary MeltDose drug-delivery technology that significantly increases the bioavailability of tacrolimus; it is designed for once a day administration. In a large-phase III study it showed comparable efficacy to that of immediate-release twice a day tacrolimus. Because of its improved absorption, patients required lower doses of Envarsus than immediate-release tacrolimus (45). Envarsus is currently available for use in Europe. Final regulatory approval and marketing of this agent in the United States are currently pending and is expected to be available for use soon.
Adverse Effects of the Calcineurin Inhibitors
Both calcineurin inhibitors have a narrow therapeutic window, multiple side effects, and drug interactions. Both drugs are metabolized by the cytochrome P450–3A4 enzyme system; their blood concentrations are affected by drugs that block or induce this cytochrome enzyme system. These drugs interact with some of the commonly used antibiotics, antifungal agents, and antihypertensive agents (Table 75.1).
Both drugs cause acute and chronic nephrotoxicity; the acute nephrotoxicity is due in part to hemodynamic changes secondary to their vasoconstrictor effects on the afferent arteriole of the glomerulus. This results in a reduction in the glomerular filtration rate, manifested by an increase in the serum creatinine concentration. This acute change is dose related and reversible. However, the lesions associated with calcineurin inhibitor–induced chronic nephropathy may lead to end-stage renal failure. These lesions, which consist of tubulointerstitial-striped fibrosis, tubular atrophy, afferent arteriolopathy, and global or focal glomerular sclerosis or collapse, have been well demonstrated in patients with autoimmune diseases treated with cyclosporine, as well as in the various organ transplant recipients: heart, liver, renal, and bone marrow (46,47). The other reported adverse effects of CsA and tacrolimus include hypertension, hyperkalemia, hyperlipidemia, and headache. Adverse effects unique to CsA include hirsutism and gingival hyperplasia, whereas those unique to tacrolimus include alopecia, fine tremor, and hyperglycemia. The adverse-effect profiles of both CsA and tacrolimus are compared in Table 75.2.
| TABLE 75.1 Common Drug Interactions with Cyclosporine and Tacrolimus |
 |
| TABLE 75.2 Adverse Effect Profile of Cyclosporine A and Tacrolimus | |||
 | |||
Dose modifications of both CsA and tacrolimus are based on whole blood trough concentrations. Monitoring of the respective drug concentrations is an essential aid in the management of a transplant recipient for the evaluation of rejection, toxicity, dose adjustments, drug interactions, and compliance. Two methods for monitoring CsA levels in whole blood include high-pressure liquid chromatography (HPLC) and radioimmunoassay, or TDx. For tacrolimus, a microparticle enzyme immunoassay (MEIA) or an enzyme-linked immunosorbent assay (ELISA)-based IMx assay are utilized. Target levels of either drug vary, based on the type of assay used, the type of monitoring (trough vs. C2 [drug level 2 hours postdose] vs. AUC [area under the curve]), transplant center standards, time posttransplantation, and the recipients’ risk for acute rejection.
Antimetabolites
Mycophenolate mofetil (MMF) (CellCept) and enteric-coated mycophenolate sodium (MPS) (Myfortic) contain the active moiety mycophenolic acid (MPA), a reversible inhibitor of inosine monophosphate dehydrogenase (IMPDH), a key, rate-limiting step in the de novo pathway of guanosine nucleotide synthesis. Depletion of the guanosine nucleotides inhibits T- and B-cell proliferation as they are dependent on the de novo pathway of purine synthesis rather than salvage pathways.
The recommended dose of MMF is 1,000 mg orally or IV twice daily, divided 12 hours apart. MMF is the prodrug of MPA and allows for increased oral bioavailability. Some centers monitor MPA drug levels for dose adjustments. The MPS equivalent is 720 mg orally twice daily, 12 hours apart, although due to differences in absorption, these two formulations are not interchangeable. MPS is not available for IV infusion and the enteric-coated tablets should not be cut, crushed, or chewed.
Adverse effects of MPA include gastrointestinal effects (dyspepsia, nausea, vomiting, diarrhea, and constipation) and bone marrow suppression (leukopenia and thrombocytopenia). Diarrhea, leukopenia, and thrombocytopenia are often dose limiting requiring dose reduction to ameliorate the toxic effects. These patients, however, should be monitored closely, as a relationship exists between an increased incidence of acute rejection and decreased MPA doses (48,49).
Azathioprine (Imuran)—a purine analog that inhibits DNA and RNA production in the T cell—is an imidazole derivative of 6-mercaptopurine. The initial recommended dose of azathioprine is 3 to 5 mg/kg/day, administered orally or IV once daily. Adverse effects of azathioprine include hematologic toxicities (pancytopenia, macrocytic anemia, thrombocytopenia, and leukopenia), alopecia, pancreatitis, and hepatotoxicity. Dose reductions may be required for myelosuppressive toxicities. A potent drug interaction may be seen with the coadministration of azathioprine and allopurinol (a xanthine oxidase inhibitor). Although it is recommended that the dose of azathioprine should be reduced by 75% when coadministered with allopurinol, it is more prudent to avoid the use of these two agents together.
mTOR Inhibitors
Sirolimus (Rapamune) is a macrolide antibiotic produced by Streptomyces hygroscopicus and is structurally similar to tacrolimus. Like tacrolimus, sirolimus also binds to FKBP-12. However, unlike tacrolimus, this complex binds to and inhibits the activation of the mammalian target of rapamycin (mTOR). This interferes with biochemical signal transductions from the cell membrane to the nucleus by inhibiting the stimulation of T cells by IL-2, -4, and -6 and by blocking the CD28 costimulatory signal. Sirolimus is available in oral tablets and solution. The recommended initial dose of sirolimus is approximately 6-mg (5 to 10 mg) loading dose, followed by 2-mg once-daily maintenance dose. Dose adjustments are made based on weekly or biweekly trough level monitoring (t1/2 = 62 hours).
Adverse effects of sirolimus include anemia, leukopenia, thrombocytopenia, hyperlipidemia, prolongation of delayed graft function, impaired wound healing, pneumonitis, arthralgia, aphthous mouth ulcers, lymphocele, and diarrhea. The advantage of sirolimus is due to its lack of nephrotoxicity (50,51). However, when coadministered with CsA, the nephrotoxic effect of CsA can be potentiated (52). Sirolimus is metabolized by the cytochrome P450–3A4 enzyme system and has a similar drug interaction profile as that of the calcineurin inhibitors.
Everolimus (Zortress) is a rapamycin derivative with increased oral bioavailability and a shorter half-life. The recommended initial dose of everolimus is 0.75 mg orally twice daily with dose adjustments made weekly or biweekly to target trough levels between 3 and 8 ng/mL. Everolimus shares some of the same advantages and adverse effects associated with sirolimus; everolimus is used in combination with cyclosporine or tacrolimus and appears to be efficacious even with lower tacrolimus doses (53).
Costimulation Blockade
Belatacept represents a new class of immunosuppressive therapy for renal transplantation. It is a selective costimulation blocker that binds to the B7 receptors on the surface of antigen-presenting cells and provides effective immunosuppression while avoiding the toxicities associated with calcineurin inhibitors. It is administered intravenously at monthly intervals in the long term. Although there is a trend toward higher rates of early rejection episodes in patients treated with belatacept, longer-term data have shown superior graft function and reduction of death or graft loss with belatacept (54). A safety issue that must be considered when using belatacept is the potential for increased risk of posttransplant lymphoproliferative disease (PTLD), especially in Epstein–Barr virus (EBV) seronegative recipients or patients treated with lymphocyte-depleting agents. Therefore, belatacept is contraindicated in kidney transplant recipients who are EBV seronegative or serologic status is unknown.
Corticosteroids
Corticosteroids exert their immunosuppressive effects through multiple pathways, the most important of which is through their ability to inhibit cytokine and cytokine receptor transcription. Corticosteroids inhibit the expression of various cytokines responsible for the activation of T cells including IL-1, -2, -3, -6, TNF-α, and IFN-γ. Corticosteroids function as both induction and maintenance immunosuppressive agents, as well as for the treatment of acute rejection episodes. Typical induction protocols call for high-dose methylprednisolone, the first dose administered intraoperatively prior to organ perfusion with tapering doses for the first few days posttransplantation. This is followed by oral prednisone with continued tapering to a baseline maintenance dose. Corticosteroids are typically administered once a day in the morning concurrent with intrinsic cortisol release.
Adverse effects of corticosteroids are numerous and include cosmetic changes, avascular necrosis, cataracts, osteoporosis, impaired wound healing, glucose intolerance, hypertension, hyperlipidemia, increased appetite, hypothalamic–adrenal axis (HPA) suppression, and mood swings.
Corticosteroids were the first immunosuppressants used when renal transplants were done in the 1960s. Because of numerous adverse effects, steroid withdrawal has been attempted, but only with moderate success because of increased acute rejection. However, with the advent of newer and more effective immunosuppressive therapy, there has been a renewed interest in early withdrawal or complete elimination of corticosteroids. Short-term success has been achieved in several small single-center trials and a few larger multicenter trials. Early corticosteroid withdrawal has also been associated with a more favorable cardiovascular risk profile, as evidenced by less hypertension, posttransplant diabetes mellitus (PTDM), and hyperlipidemia (55).
MINIMIZING OPPORTUNISTIC INFECTIONS IN THE TRANSPLANT
Recipient
Within the first month following transplantation, surgical wound-related and nosocomial infections are the most common infections observed in renal allograft recipients. As a result, bacterial infections involving the urinary tract, the respiratory tract, the surgical wound, and/or intravenous lines are the ones frequently encountered. In a few instances, infections may be due to reactivation of pre-existing infection in the recipient such as subclinical bacterial infections, especially urinary tract infections (UTIs) and tuberculosis, or transmission of infections from the donor to the recipient.
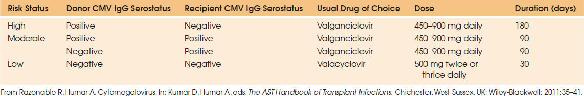
Infections in the 1- to 6-month period after transplantation are due to opportunistic organisms, most notably viruses belonging to the herpes group, especially cytomegalovirus (CMV), and due to Candida species and Pneumocystis jiroveci. Antimicrobial prophylaxis specific to these opportunistic organisms should be given to all renal allograft recipients early posttransplantation. Prophylaxis protocols differ among centers in antimicrobial selection and duration of therapy. Prophylaxis with antifungals such as clotrimazole, nystatin, or fluconazole may be used against Candida infections of the mouth and throat (thrush). Prophylaxis against P. jiroveci pneumonia (PCP) includes sulfamethoxazole/trimethoprim; for those patients with a sulfa allergy, monthly inhaled pentamidine or oral dapsone will provide adequate prophylaxis against PCP. Drug and dose selection of antiviral prophylaxis against CMV infection can be stratified by infection risk based on previous CMV exposure, or the presence of anti-CMV antibodies in the recipient (Table 75.3). Valganciclovir is currently the drug of choice for antiviral prophylaxis against CMV.
| TABLE 75.3 Cytomegalovirus (CMV) Risk Stratification and Treatment Options |
 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








