Lidocaine toxicity
Cardiovascular and central nervous system toxicity depend on the mass of drug reaching the systemic circulation. The transfer of drug (by diffusion) from the circulation to organs is determined by the Fick principle (see Chapter 14). The mass of drug reaching the circulation after peripheral administration is influenced by the following factors:
Mass of drug administered
Site of injection
Tissue protein binding and metabolism
Vascularity of the injection site
Dose
The volume and concentration of local anaesthetic agents, considered individually, have little influence on systemic spread. Systemically the mass of drug rather than its administered concentration is more important.
Absorption
Absorption from different sites is influenced by the blood flow to the tissue and the uptake of the drug into the vascular compartment, which is a function of solubility. Absorption occurs in the following order of magnitude:
Absorption is particularly high when agents are applied topically to mucosa (such as lidocaine spray in the oropharynx). A vasoconstrictor may be added to reduce absorption. Cocaine produces vasoconstriction in its own right and is used on the nasal mucosa to reduce vascularity before some ENT procedures.
Accidental IV injection bypasses the absorption process and subjects the patient to potentially toxic levels of drug. Intravenous regional anaesthesia (IVRA) involves the deliberate introduction of local anaesthetic into the venous system of a limb isolated by tourniquet. The safety of this procedure is dependent on the drug becoming predominantly tissue-bound by the time the tourniquet is released, which should not be for at least 20 minutes. Further improvements in safety can be achieved by using relatively non-cardiotoxic drugs, typically prilocaine.
Distribution
Absorbed drug passes through the lungs, where a large amount of the local anaesthetic agent may become tissue-bound and in some cases metabolised. However, this ability is soon saturated by direct IV injection. After passing through the lungs, local anaesthetic drugs reach vessel-rich tissues which have a high affinity. Some is distributed to muscle and fat, and later gradually released for subsequent metabolism.
Metabolism
Ester local anaesthetics are rapidly metabolised by plasma cholinesterase, and systemic toxicity is rarely a problem. Amide local anaesthetics are metabolised by the liver, but hepatic failure must be very severe before local anaesthetic breakdown is compromised. Lidocaine has a high extraction ratio, and metabolism is therefore dependent on hepatic blood flow, which may be particularly relevant when IV lidocaine is used to stabilise ventricular myocardium in low-cardiac-output states.
Plasma protein binding
α1-Acid glycoprotein and albumin are the main sites for local anaesthetic binding within the plasma. α1-Acid glycoprotein has a high affinity but a low capacity, while albumin has a low affinity but a high capacity for local anaesthetics. Figure 7.4 shows the plasma protein binding of drugs at different plasma concentrations.
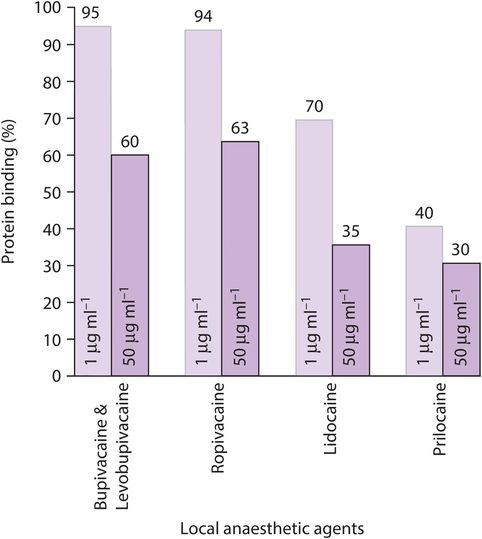
Plasma protein binding of drugs at different plasma concentrations
Protein binding acts as a buffer to changes in plasma concentration. The chemical bonds are weak and the protein readily releases the local anaesthetic as concentration falls. Toxicity is therefore not directly linked to plasma protein binding, and tissue binding is the more important factor.
Pregnancy
Fetal blood rapidly equilibrates with maternal blood levels of free local anaesthetic agent, but as there is more α1-acid glycoprotein in fetal blood the overall concentration will be higher. Metabolism is less well developed in the fetus, but the drug rapidly passes back to the mother as maternal levels decline; therefore this does not present a problem. The pH of the fetal fluids is lower than maternal, which acts to increase the proportion of ionised local anaesthetic agent.
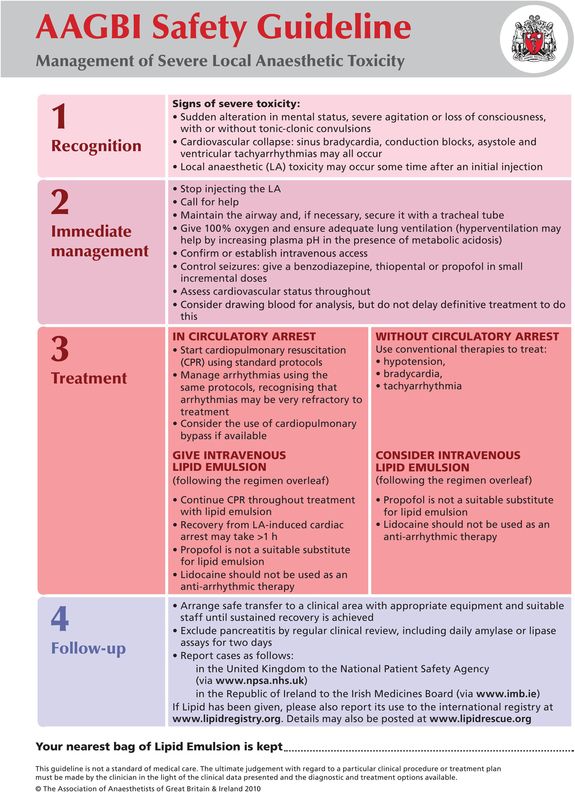
Management of local anaesthetic toxicity
Guidelines are available from the Association of Anaesthetists of Great Britain and Ireland (2010) (Figure 7.5).
AAGBI guidelines on the management of local anaesthetic toxicity
Prevention
Careful observation of patients receiving local anaesthetic agents, and a high degree of suspicion both during and after administration, is essential. Make use of the maximum recommended doses as a guide, and combine that with careful technique and an appreciation of the anatomy. If any suspicion of central toxicity arises then stop the injection and re-evaluate.
Treatment
If toxicity does occur, then first stop injecting the local anaesthetic. Call for help. Supportive measures for airway and circulation are the mainstay of successful treatment. Seizures should be controlled with incremental midazolam, thiopental or propofol. Sodium channel blocking agents should not be used, as they will only worsen the situation. If cardiac arrest occurs then inotropes, vasopressors and vagolytics may help. Lidocaine, of course, must be avoided. Bupivacaine is particularly tissue-bound, and cardiac massage for an hour or more may be required.
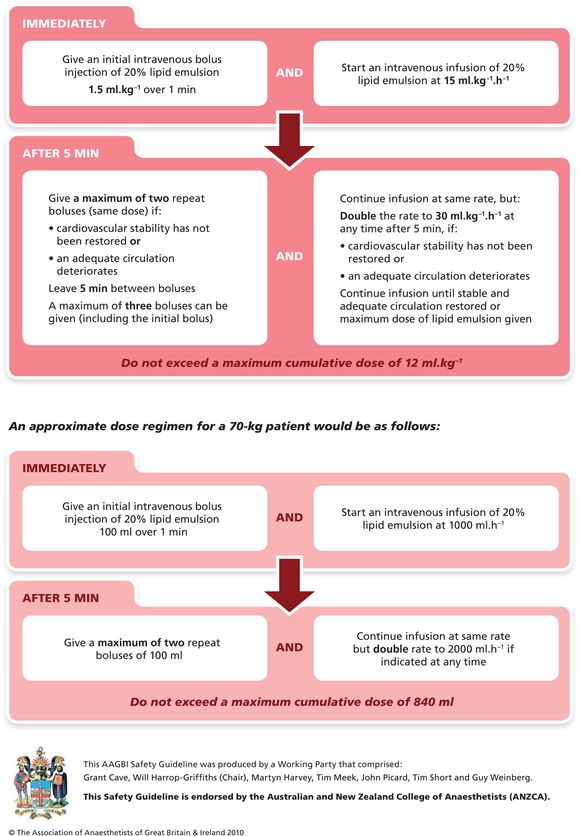
Lipid emulsion
The use of lipid emulsion is primarily based on animal studies, although case reports have appeared for bupivacaine, levobupivacaine and ropivacaine. Although the exact mechanism of action is unknown, the following have been postulated:
Intravascular bupivacaine is absorbed into the lipid (very slow for removing myocardial bupivacaine).
The lipid delivers a significant concentration of fatty acids to the energy-starved myocardium, allowing replenishment of the ATP as cardiac resuscitation continues.
Picard & Meek (2006) provide a useful discussion of the potential benefits. Uptake into the lipid phase is dependent on the lipid/aqueous plasma partition coefficient, which varies with Intralipid mixture and species. It is important to appreciate that propofol, while useful to treat convulsions, in the volumes that could be given has too little lipid to make any impact on treating toxicity. Intralipid 20%, by comparison, would be given in a bolus of the order of 100 mL followed by an infusion.
Insulin/glucose/potassium infusions
This method has not become part of the management of local anaesthetic toxicity, but the underlying mechanism may be of relevance. Kim et al. (2004) induced cardiovascular collapse without arrest in dogs using a bupivacaine infusion. They then stopped the bupivacaine and gave one group a bolus of insulin. Potassium and glucose were then infused. All the dogs in the insulin group gradually improved and survived while the entire control group died. It is postulated that the successful resuscitation using insulin was due to a reversal of bupivacaine-induced changes to potassium ion flux, calcium ion transport in the sarcoplasmic reticulum and maybe improved mitochondrial glucose and pyruvate levels as well.
Performing the block
Major regional anaesthetic techniques require formal sterile precautions, especially central nerve blocks, where meningitis and epidural abscess are rare but definite risks. Direct contact of chlorhexidine skin preparation with neural tissue has been implicated in cases of permanent neurological harm following neuraxial block. Scrupulous attention should be paid to avoiding contact of chlorhexidine with equipment and gloves, and it should be given time to dry before beginning the procedure. Chlorhexidine 0.5% is as effective as a 2% preparation in achieving asepsis and is theoretically less toxic.
In addition to the potentially toxic properties of local anaesthetic drugs discussed above, all regional anaesthesia techniques have associated complications. Airway and resuscitation skills are essential to the practice of regional anaesthesia. Figure 7.6 describes the general requirements for successful practice.
| Secure intravenous access |
| Full resuscitation apparatus |
| Adequate patient monitoring equipment |
| Ability to administer general anaesthesia rapidly |
| Fully trained anaesthetic assistance |
| Suitable sterile packs (reusable or disposable) |
| A full range of sterile needles and other necessary equipment |
| Adequate space to maintain sterility |
| Surroundings that offer privacy, good lighting and warmth |
Perioperative management
During performance of the block verbal contact with the patient should be maintained to offer reassurance and explanation of the unfolding events. Staff within the operating theatre must be aware of the impact of their noise and activity on the patient. Patients who have received premedication or intravenous sedation often sleep during surgery once the block is fully established and the initial surge of activity during preparation for surgery has subsided. Occasional verbal contact should still be maintained as part of the routine monitoring of the patient. Central neural blocks have the potential to cause hypotension due to peripheral vasodilatation and reduced venous return. Hypotension responds to changes in posture. Slight head-down tilt with elevation of the legs will restore venous return, and intravenous fluids may be required. Bradycardia should be treated with appropriate vagolytic therapy (e.g. glycopyrrolate 200–400 μg IV), and vasopressors (e.g. ephedrine 3–6 mg IV or metaraminol 0.25–0.5 mg IV) may be necessary if hypotension does not respond to the above measures.
The patient will be unable to protect anaesthetised limbs from pressure or extremes of posture and, if the procedure is prolonged, may become distressed by being unable to change position. It is therefore important to protect the anaesthetised parts of the body and to maintain a comfortable posture for the patient. Postoperatively, the affected limbs need protection from injury and pressure, and patients should be mobilised with care to guard against postural hypotension until the effects of the block have worn off.
Central neural blockade
There are three neuraxial techniques in common use, and their terminology can confuse because terms are used interchangeably. Spinal (synonym: intrathecal or subarachnoid), epidural (synonym: extradural or peridural) and caudal (synonym: sacral epidural) are the preferred terms for anaesthesia and analgesia within the boundaries of the spinal column.
Spinal anaesthesia
Indications for spinal anaesthesia
Spinal anaesthesia is used for a wide variety of both elective and emergency surgical procedures below the level of the umbilicus. For surgery above the umbilicus, high spinals are now rarely used because of associated difficulties of maintaining spontaneous ventilation and abolishing the painful stimuli from traction on the peritoneum and pressure on the diaphragm.
Anatomy
Spinal anaesthesia requires the injection of a small volume of local anaesthetic agent directly into the cerebrospinal fluid (CSF) in the lumbar region, below the level of L1/2, where the spinal cord ends. Figure 7.7 shows the typical anatomy of the lumbar spine in cross-section.
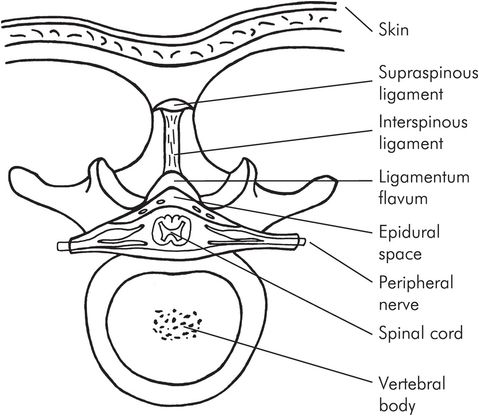
Cross-section of the lumbar spine at L1
The meninges surround the spinal cord from the foramen magnum as far down as the second sacral segment (S2). The dura mater is a tough fibroelastic membrane, beneath which lies the delicate arachnoid mater. The dura mater invests the spinal cord and the spinal nerve roots, forming the dural cuffs which extend laterally as far as the intervertebral foramina. Although the arachnoid is attached to the dura there is a potential space between the layers (the subdural space), and inadvertent injection into this space is a recognised complication of both spinal and epidural injections. The pia mater is a delicate vascular layer closely adherent to the spinal cord. Lateral projections of the pia form the dentate ligaments, which attach to the dura and stabilise the spinal cord. The filum terminale is the caudal extension of the pia that anchors the spinal cord and dura to the periosteum of the coccyx. There are 31 pairs of spinal nerves (8 cervical, 12 thoracic, 5 lumbar, 5 sacral, 1 coccygeal) arising from the spinal cord, which extends from the foramen magnum to the L1/2 vertebral level. Below this level, the lumbar and sacral nerves form the cauda equina, which offers a large surface area of nerve roots covered only by the pia mater and accounts for the sensitivity of these nerves to local anaesthetic agents administered centrally.
Physiology
Cerebrospinal fluid (CSF) is a clear fluid with a mean specific gravity of 1.006 at 37 °C, which is actively secreted by the choroid plexi in the lateral and fourth ventricles at a rate of up to 500 mL per day. With a CSF volume of 150 mL that means that the total volume changes 3–4 times a day. There is no active flow, movement occurring by diffusion and changes in posture. Absorption occurs (at equilibrium with production) via the arachnoid villi of the major cerebral sinuses. The typical composition of CSF is shown in Figure 7.8. A number of factors affect the spread of local anaesthetic within the CSF, and these are listed in Figure 7.9.
| Total volume (brain and spinal cord) approximately 130 mL | |
| Volume around spinal cord approximately 35 mL | |
| CSF pressure in lumbar region | 6–10 cmH2O (lateral position) |
| 20–25 cmH2O (sitting) | |
| Hydrogen ion concentration 40–45 nmol L–1 | |
| Protein content 20–40 mg L–1 | |
| Major influence |
|
| Minor influence |
|
The maximal spread, duration and quality of the block is mostly influenced by the posture of the patient during and immediately after the injection, and the density of the solution. The ratio of the density of the solution to that of CSF is expressed as baricity (where isobaricity = 1.0). If the injection is made at the L3/4 interspace with the patient in the left lateral position and the patient is then immediately turned supine, hypo- and hyperbaric solutions produce different effects due to their distribution patterns. Hypobaric solutions are not commonly available in the UK now but have been used in the past for lower abdominal and lower extremity surgery, as they tend to be restricted to the top of the lumbar lordosis when the patient lies supine. With the use of head-up tilt, the height of the block can be encouraged in a cephalad direction but at the expense of a patchy quality of anaesthesia and an unpredictable height. Head-down tilt will restrict the caudad limit of the block. Commercially produced bupivacaine (normally described as isobaric) is slightly hypobaric (0.999) at body temperature and can produce unpredictable results with changing posture. Hyperbaric bupivacaine is commonly used for spinal anaesthesia in the UK at present. As hyperbaric solutions are hypertonic they remain affected by posture for up to 30 minutes after injection, and so sensory levels may change within that time. This explains why so-called saddle blocks and unilateral spinals can rarely, if ever, be achieved with hyperbaric solutions. Isobaric solutions (chirocaine) are also being increasingly used. The block in this case is not influenced by posture, but mainly determined by level of injection and volume.
The effects of a spinal anaesthetic on the physiology of the major organ systems are related primarily to the height of the block. Specific organ systems affected are detailed below.
Nervous system
As a rule there is total neural blockade caudad to the injection site while cephalad to it the concentration of local anaesthetic decreases, producing a differential nerve block of the sensory, motor and autonomic fibres. Sympathetic fibres are most sensitive and may be blocked two to six segments higher than sensory fibres, which in turn may be blocked a few segments higher than the associated motor block.
Respiratory system
Below the thoracic nerves, spinal anaesthesia has no clinical effect on respiratory function but as the intercostal nerves become progressively blocked, active expiratory mechanics are impaired, producing a reduction in vital capacity and expiratory reserve volume. Tidal volume and other inspiratory mechanics remain normal due to increased diaphragm movement. Patients may complain of dyspnoea and may lose the ability to cough effectively. If there is exceptional cephalad spread and the cervical nerves become affected, apnoea due to phrenic nerve blockade can occur.
Cardiovascular system
Progressive blockade of the thoracolumbar sympathetic outflow produces increasing vasodilatation of the resistance and capacitance vessels and a reduction of 15–18% in systemic vascular resistance. If the cardiac output is maintained, there will be a similar fall in mean arterial pressure. If, however, the cardiac output falls due to a reduction in preload (for example due to hypovolaemia or a reduction in venous return due to postural changes) then hypotension may develop rapidly, especially if the block reaches the cardioaccelerator fibres above the level of T4/5, when a reflex bradycardia may occur. Above the level of the block there is usually compensatory vasoconstriction, but this is not sufficient to prevent significant falls in arterial pressure if the block is extensive.
Gastrointestinal system
Sympathetic blockade allows vagal parasympathetic activity to predominate. Gastric emptying and peristalsis continue, sphincters relax and the bowel is generally contracted. This may preclude the use of central blockade in patients with obstructed bowel, at least until the obstruction has been relieved. However, the incidence of postoperative ileus is reduced by spinal and epidural blockade, and this is one of their main benefits. Nausea and vomiting can occur as a result of the unopposed vagal activity, if the peritoneal contents are stimulated in the awake patient.
Equipment
Spinal anaesthesia requires specialised needles and introducers in addition to the general equipment necessary for central nerve blocks (Figure 7.10). There is an inevitable incidence of post-dural puncture headache (PDPH) with spinal anaesthesia, ranging from 0.2% to 24%, and many designs of needle have been introduced to try and reduce this problem. Currently the lowest incidence of PDPH is associated with narrow-gauge, short-bevel needles (26–29 G) and 24 G pencil-point Whitacre tip designs, or the more specialised Sprotte designs with a large side-opening hole. The narrow gauge and relatively blunt tips of these needles necessitate insertion through a properly designed introducer, which should be closely matched to the type of spinal needle being used, to avoid tip damage.
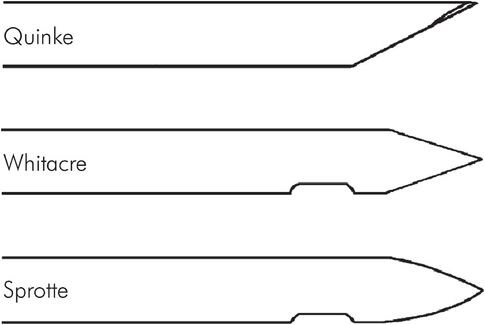
Tip designs of spinal needles
Technique
Successful spinal anaesthesia depends on a reliable lumbar puncture technique. First establish venous access with a wide-bore cannula and then position the patient either in the lateral position with the spine flexed maximally to open up the gaps between the vertebral spines or in the sitting position with the feet placed on a low stool at the side of the bed and the elbows resting on the thighs (Figure 7.11). Each position has drawbacks and advantages, and the choice is usually made on personal preference. In either case, a skilled assistant is necessary to position the patient correctly, maintain and support the posture and establish a rapport with the patient during the conduct of the block.
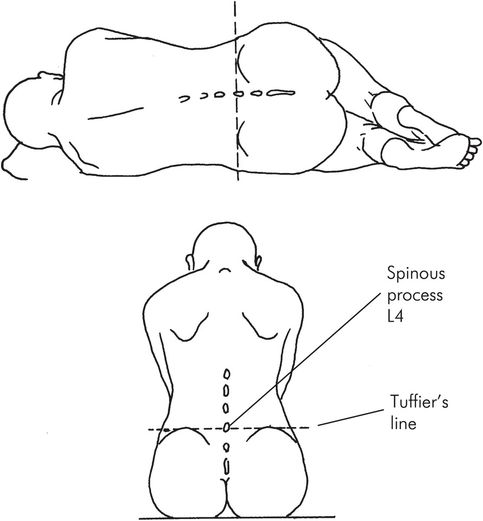
Patient positions for spinal anaesthesia
A line joining both iliac crests (Tuffier’s line) passes across the spine of L4 and is a useful topographical landmark for locating the L3/4 interspace, which is usually easily defined and is the one most often used. Ultrasound can be used to assist identification of the midline and lumbar interspaces in patients with poorly recognizable landmarks.
The technique for spinal anaesthesia is described in Figure 7.12.
| Sterilise the skin over the lumbar spine with a spirit-based antiseptic and raise a skin weal with lidocaine 1% over the appropriate interspace. Inject 2–3 mL more lidocaine into the subcutaneous tissue. Anchor the skin over the interspace by pressing the non-dominant index finger on the spine of the cephalad vertebra and insert the needle or introducer in the midline at 90° to the skin. Feedback from the needle tip will monitor the progress of the needle through the supraspinous and interspinous ligaments, the ligamentum flavum and sometimes the dura mater. If bone is contacted, withdraw the needle to the subcutaneous tissue and redirect slightly cephalad in the first instance. Puncture of the dura is usually obvious, and when the stylet is removed CSF should flow freely. |
Note that 22 G needles are robust enough to be used in patients with calcified ligaments or other anatomical difficulties, and they are recommended for elderly patients, where these problems are more common and the risk of PDPH is very low. If an introducer is required, it should be inserted into the deep layers of the interspinous ligament, so that the needle has only a short distance to travel. Narrow-gauge needles may deviate or be damaged by the ligamentum flavum, calcified ligaments or osteophytes and also will give little feedback. After performing the block the blood pressure, pulse rate and ECG should be monitored, as the onset of sympathetic nerve blockade is quite rapid. When using 3 mL bupivacaine 0.5% in 8% glucose (so-called hyperbaric solution), motor and sensory loss will be apparent within a few minutes but the block may not be fully complete for up to 25 minutes. Sensory block can be tested using a blunt pinprick or loss of temperature sensation with an alcohol swab. Dermatomes should be tested bilaterally starting in the dermatome nearest to the level of injection. Motor loss is usually estimated using the Bromage scale (Figure 7.13).
| Degree of motor block | Bromage criterion | % score |
|---|---|---|
| (1) No block | Full flexion of knees and feet | 0 |
| (2) Partial block | Just able to flex knees plus full flexion of feet | 33 |
| (3) Almost complete | Unable to flex knees, some foot flexion still | 66 |
| (4) Complete | Unable to move legs or feet | 100 |
Normally, the whole procedure is conducted with the patient conscious or lightly premedicated, so as to maintain verbal contact and cooperation. If turning the patient is likely to be painful (for example in those with fractured neck of femur) then intravenous ketamine 0.5 mg kg–1 may be administered to provide analgesia during insertion of the spinal.
Drugs, doses and volumes
Figure 7.14 gives a guide to drug administration for various operative sites, based on a fit adult of normal stature (70 kg); smaller volumes may be necessary for higher-risk patients. Hyperbaric bupivacaine 0.5% gives a reliable surgical block for 2–3 hours. Plain ‘isobaric’ bupivacaine 0.5% 3–4 mL is also commonly used but is less reliable above T10.
| Operation site | Block level | Drug volume (hyperbaric bupivacaine 0.5%) |
|---|---|---|
| Perianal | L 4/5 | 2.5 mL |
| Urogenital | T 10 | 2.75–3.0 mL |
| Lower abdominal | T 6/7 | 3.0–3.25 mL |
Complications
Some complications (hypotension, urinary retention, bradycardia) are actually physiological consequences of central neural blockade and should not represent a clinical problem if correctly managed. If management is inappropriate, secondary effects such as nausea and vomiting, faintness or vasovagal loss of consciousness may follow. Total spinal blockade requires urgent supportive management, which may include leg elevation, ventilatory support including intubation, IV fluids and vasopressors. The Third National Audit Project, Major Complications of Central Neuraxial Block in the United Kingdom (NAP3) examined the incidence of complications. The main findings are outlined in Figure 7.15.
| The NAP3 report (published in 2009) covered injuries reported in 700,000 CNB cases 46% spinals, 41% epidurals 45% obstetric, 44% perioperative |
| Results 84 ‘major’ incidents out of 700,000 cases reported 67% resolved completely Injuries were judged either ‘optimistically’ or ‘pessimistically’ according to the census reports submitted |
| Permanent injuries Between 14 (optimistic) and 30 (pessimistic) permanent injuries 2.0–4.2 per 100,000 cases (between 1 in 54,000 and 1 in 24,000) 60% after epidurals, 23% after spinals, 13% after CSE |
| Deaths or paraplegias Between 5 (optimistic) and 13 (pessimistic) 0.7–1.8 per 100,000 cases (between 1 in 140,000 and 1 in 50,000) |
Headache
Loss of CSF through the dural puncture site will produce a low-pressure headache due to traction on the cranial meninges. The main characteristics of a spinal headache are that it is minimal when lying flat, is severe when sitting up or standing, occurs in the occipital and bifrontal distribution, and may be worsened by coughing or straining. In severe cases the traction may produce cranial nerve symptoms with alterations in vision and hearing. Onset is usually within 24 hours of the injection, and the majority of PDPH diminishes rapidly with rest, oral analgesia and adequate hydration and should resolve within 7 days. Occasionally more invasive treatment is required in high-risk groups such as pregnant women and after puncture with large-bore needles. An epidural blood patch, in which up to 20 mL of the patient’s blood is withdrawn from a vein under the strictest sterile precautions and injected through an epidural needle placed as close to the level of the dural puncture as possible, is very effective at relieving a PDPH, with > 90% success with the first injection. Other causes of headache should be considered before ascribing the cause to the spinal and a careful history of events should be elicited, as headaches are a very frequent complaint after surgery or labour.
Neurological sequelae
Temporary symptoms of paraesthesia, hypoaesthesia and motor weakness may follow spinal anaesthesia but are not necessarily the result of trauma to a spinal nerve root. These symptoms occur from pressure, surgical trauma or stretching of the root or peripheral nerve, and the great majority resolve spontaneously within a few weeks. Serious, permanent neurological damage is extremely rare, but in view of the serious consequences of such an event, any neurological sequelae should be formally examined by a neurologist with experience of this type of damage as soon as the problem arises. Other rare causes of neurological damage include brain damage and anterior spinal artery syndrome due to excessive and prolonged hypotension, infection (meningitis and epidural abscess), arachnoiditis and cauda equina syndrome (both associated with the injection of incorrect solutions), and are usually the result of a failure of technique.
Epidural anaesthesia
Indications
Surgery can be undertaken within the abdomen and the lower limbs using an epidural as the sole anaesthetic technique, but it is more usual to combine epidural anaesthesia and a general anaesthetic. Epidural infusions are extensively used for postoperative analgesia following thoracic and major abdominal surgery, as well as in the management of some acute and chronic pain conditions (Figure 7.16).
| Surgery |
|
| Acute pain relief |
|
| Chronic pain states |
|
The salient significant differences between spinal and epidural approaches are summarised in Figure 7.17. These differences apply to single-shot, local anaesthetic blocks; the addition of adjuvant drugs (such as opioids or α2-agonists) can alter the characteristics of each technique. For epidural administration it is customary to insert a catheter to allow top-up doses or prolonged infusions, whereas spinal catheters are not commonplace. Combined spinal and epidural (CSE) anaesthesia is used, especially for obstetric surgery, to utilise the benefits of both techniques. Surgical block can be rapidly established with a small dose of spinal bupivacaine (2–2.5 mL hyperbaric solution) followed by the slower onset of a low-dose epidural, which can be used to extend operating time and postoperative analgesia. However, the NAP3 study demonstrated an increased relative risk with this combined technique, compared to when spinal and epidural techniques are used alone, and a careful evaluation of individual risk should be discussed with the patient.
| Spinal | Epidural | |
|---|---|---|
| Onset | 2–5 minutes | 20–30 minutes |
| Duration | 2–3 hours (single shot) | 3–5 hours |
| Drug volume | 2.5–4 mL | 20–30 mL |
| Quality of block | Rapid surgical anaesthesia | May be inadequate in some dermatomes |
In summary, spinals provide rapid-onset, short-duration surgical anaesthesia below the umbilicus with small doses of drug. Epidurals have a slower onset time, require large doses of drug and produce less dense surgical anaesthesia but can be used more flexibly in the lumbar and thoracic regions, and their duration may be extended to days or weeks for analgesia by the insertion of a catheter.
Physiology
The effects of epidural anaesthesia on the major organ systems are similar to those of spinal anaesthesia, with the height of the block being the major determinant. In a patient with compromised cardiovascular or respiratory reserve, the slower onset of epidural blockade gives more time to manage the onset of hypotension and other side effects, although against this advantage must be weighed the risks of the need for a much larger dose of local anaesthetic drug. The spread of local anaesthetic solution within the epidural space and thus the ultimate height of block is determined by a number of factors (Figure 7.18).
| Factors | Comment |
|---|---|
| Drug mass | Drug mass is critical, and more important than either volume or concentration |
| Drug volume | For a given drug mass, larger volume gives more spread than a small volume |
| Site of injection | The epidural space increases in volume in a caudal direction. Thus a given volume will spread further in the cervical > thoracic > lumbar > sacral Onset is fastest and the block most intense in the dermatomes nearest the site of injection |
| Age | A given volume spreads further with increasing age over 40 years |
| Raised abdominal pressure | Smaller volumes may be needed in pregnancy and morbid obesity |
| Patient position | Prolonged sitting position may reduce upward spread. Earlier onset of block in dependent side |
| Injection technique | Slow ‘unfractionated’ injection of dose through needle gives fewer incomplete blocks than ‘fractionated’ or incremental doses |
Equipment
In addition to the equipment necessary for spinal anaesthesia (see above) a suitable epidural pack will be required. There are several commercial packs readily available, and these will contain a loss-of-resistance syringe, Tuohy needle, catheter and bacterial filter as a basic set.
Technique
The practical technique of lumbar midline approach to the epidural space is described in Figure 7.19.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







