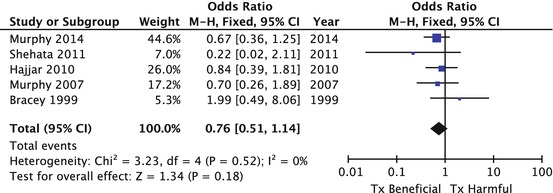
Fig. 5.1
Forest plot of the odds of mortality for transfusion versus no transfusion from observational studies. Individual references are available on request
5.3 Randomised Controlled Trials on Red Blood Cell Transfusion in Non-Cardiac Surgery Patients
A recent Cochrane review summarised the results of published RCTs that have attempted to determine safe levels of anaemia or appropriate transfusion threshold across a range of clinical settings [25]. These RCTs, commonly referred to as ‘trigger trials’, determine whether patient allocation to a more liberal transfusion threshold, based usually on a higher blood haematocrit or haemoglobin concentration, results in a different clinical outcome to a more restrictive or lower transfusion threshold. Thus, both groups are exposed to transfusion albeit at different frequencies and also to different levels of anaemia. In this respect, they differ from observational studies in that they do not attempt to define the risks of transfusion or anaemia in isolation and reflect the absolute interdependence of these two factors. This is pragmatic, there is no ethical basis upon which transfusion could be completely withheld from one group of patients, and they reflect the almost universal use of haemoglobin/haematocrit measurements to guide red blood cell transfusion decisions. These trials are limited in that they assume a universal anaemia threshold that is applicable to all patients and cannot inform individual treatment decisions, although this is commonplace in clinical practice and a criticism of all RCTs. Many of these trials also have design limitations that significantly increase the risk of bias. Firstly, most are underpowered to detect differences in important clinical endpoints such as death. Secondly, randomised trials commonly recruit selected groups of relatively low-risk patients who have low frequencies of the adverse outcomes the intervention is intended to influence. Thirdly, by randomising all consented patients, many of whom never develop severe anaemia, they result in large proportions of patients in either group who never require transfusion. Finally, few of these studies report compliance to allocated transfusion thresholds, a potential source of procedural bias. These sources of bias tend to move the effect estimate of the intervention towards the null. Quantitative meta-analyses of the outcomes from these trials do not overcome all of these limitations. They are also limited in that they assume that the patient groups will be homogeneous, with a similar balance of risks and benefits over a wide range of restrictive and liberal transfusion thresholds in different clinical settings. Perhaps unsurprisingly, these meta-analyses show no apparent difference between restrictive and liberal transfusion strategies (Fig. 5.2). That is not to say that these findings must be discounted. They are supported by the findings of a recent large high-quality RCT in high-risk patients. The Functional Outcomes in Cardiovascular Patients Undergoing Surgical Hip Fracture Repair (FOCUS) trial compared liberal and restrictive transfusion thresholds in 2016 hip fracture patients, of whom 63 % had a history of cardiovascular disease. This trial only randomised patients with haemoglobin levels <10 g/dL and carefully documented non-adherence to the study protocol (8 %). The FOCUS trial reported no difference in a range of clinical outcomes, including death or major morbidity. Thus, best evidence suggests that restrictive transfusion is not harmful in non-cardiac surgery patients. Moreover, in the absence of harm, restrictive practice should be adopted; there is no clinical indication to provide a therapy that has no benefit but a considerable cost, as concluded by the Cochrane review [22, 25]. Importantly however, the patients in the FOCUS and other trials did not have symptomatic cardiac disease and did not undergo surgery with cardiopulmonary bypass. Transfusion decisions in cardiac surgery are best informed by trials conducted in cardiac surgery patients.
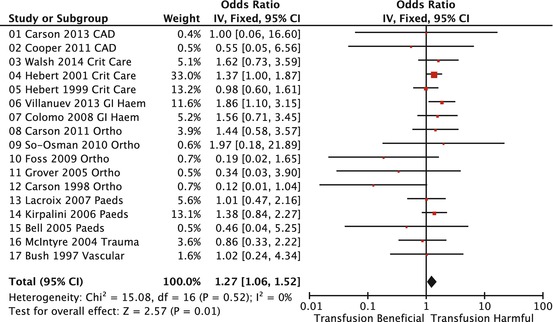
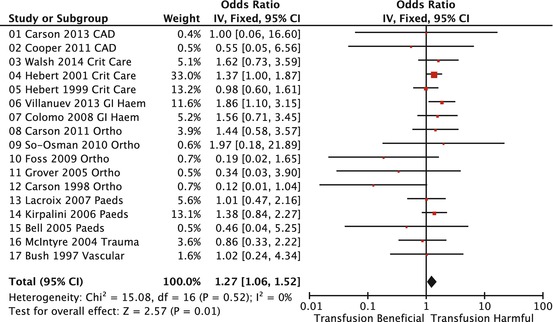
Fig. 5.2
Forest plot of the odds of mortality for restrictive transfusion versus liberal transfusion from non-cardiac surgery RCTs. Individual studies are as labelled in reference [25]
5.4 Randomised Trials on Red Blood Cell Transfusion in Cardiac Surgery Patients
Six RCTs [26–31] have thus far compared liberal with restrictive transfusion practices in patients undergoing cardiac surgery in a total of 3,356 patients (Fig. 5.3). These trials demonstrate many of the limitations observed in non-cardiac surgery RCTs. In particular, all but 1 of these trials, the Transfusion Indication Threshold Reduction (TITRe 2) trial, did not select only those who required transfusion, i.e. those that developed predefined level of anaemia prior to randomisation. TITRe 2 was also the only trial adequately powered to demonstrate differences in important clinical outcomes. Meta-analysis of these trials is dominated by this and another trial, the single-centre Transfusion Requirements After Cardiac Surgery (TRACS) trial [20]. The TRACS trial randomised 502 patients to restrictive and liberal transfusion thresholds. However, all consented patients were randomised in this study, reducing the ability of the trial to detect a treatment effect; 22 % in the liberal group did not receive any transfusion despite a liberal trigger which was higher than in most other trials (haematocrit 30 %). In the TRACS trial, there was no difference between the groups with respect to death or major morbidity. The TITRe 2 trial was a multicentre trial in 16 UK cardiac centres that recruited 3,565 patients of whom 2007 breached the threshold of 9 g/dL and were randomised to either a restrictive threshold of 7.5 g/dL or a liberal threshold of 9 g/dL. Fifty-three percent of patients were transfused in the restrictive group, and 92 % were transfused in the liberal group. Non-adherence was closely monitored and was similar to that observed in the FOCUS trial (8 %). There was no difference between the two groups in terms of the primary outcome, a composite of any infectious or ischaemic complication. However, sensitivity analyses that included acute kidney injury as objectively determined by serial creatinine measurements in the primary outcome did demonstrate increased risk of harm in the restrictive group (odds ratio for infectious or ischaemic morbidity = 1.20, 95 % confidence intervals (CI) 1.00–1.44, p = 0.045). This finding was supported by an analysis of secondary outcomes including death, which was increased in the restrictive group (4.2 % versus 2.6 %; hazard ratio = 1.64, 95 % CI 1.00–2.67, p = 0.045). Quantitative meta-analysis of all the trials that have compared liberal with restrictive transfusions in cardiac surgery also indicates a benefit from more liberal transfusion thresholds (Fig. 5.3), with, importantly, a reduced risk of death from liberal transfusion (OR = 0.76, 95 % CI 0.51–1.14). The cardiac surgery trials used different thresholds, and there is insufficient evidence from these trials to recommend a specific anaemia threshold. The TITRe 2 trial suggested that a threshold of 9 g/dL may be appropriate. Interestingly, subgroup analysis did not detect any interaction between the effect estimate and a range of risk factors including poor left ventricular function, diabetes, and age greater than 75 years, factors commonly used to influence transfusion decisions.
5.5 Summary and Conclusions
Contemporary blood management guidelines, and increasingly health policy, advocate restrictive transfusion practice, with the caveat that thresholds should be increased in high-risk patients. The use of restrictive thresholds is supported by the findings of observational studies and RCTs in non-cardiac surgery patients. These studies are not adequate to inform transfusion decisions in cardiac surgery however. Existing observational studies in cardiac surgery patients lack the methodological rigour to determine safe levels of anaemia, and the findings of RCTs in non-cardiac surgery patients fail to address the specific nature of the patients presenting for cardiac surgery, principally the existence of symptomatic disease, and the altered oxygen utilisation characteristic of CPB. RCTs in cardiac surgery have until recently suffered from significant limitations making interpretation difficult. However, the recent TITRe 2 trial, which has randomised significantly more patients than all the previous cardiac surgery RCTs combined, indicates that restrictive transfusion practice may not be safe in this highly specific clinical setting, and this is supported by quantitative meta-analysis of this and other cardiac surgery ‘trigger’ trials. Moreover, other risk factors that are often considered to influence transfusion requirements such as age and co-morbidity did not influence this result, further supporting a hypothesis that these patients exist at the limits of the oxygen supply/utilisation balance. Here we suggest that cardiac surgery therefore represents a specific high-risk group where restrictive practice is not safe. This hypothesis will be tested by the Transfusion Requirements in Cardiac Surgery III (TRACS III) trial (NCT02042898). TRACS III is an international multicentre RCT comparing liberal with restrictive thresholds that started recruiting in January 2014. This trial will enrol 3,592 patients, more than all previous trials combined that is powered to detect differences in death and major morbidity. However, until the results of this trial are presented, expected in 2018, the available evidence suggests that more liberal transfusion thresholds of a haemoglobin of 9 g/dL be adopted in cardiac surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree