Chapter 11 Radiation Safety and Complications of Fluoroscopy, Ultrasonography, and Computed Tomography
 Patient doses can be minimized by limiting the time of fluoroscopy; proper positioning of the C-arm; use of collimation; and if necessary, shielding the patient.
Patient doses can be minimized by limiting the time of fluoroscopy; proper positioning of the C-arm; use of collimation; and if necessary, shielding the patient. Scattered radiation exposure, the major radiation risk to procedure room staff, can be reduced by use of personal protective equipment such as lead aprons, lead shielding, and maximizing the distance from the x-ray source.
Scattered radiation exposure, the major radiation risk to procedure room staff, can be reduced by use of personal protective equipment such as lead aprons, lead shielding, and maximizing the distance from the x-ray source. Consideration should be given to the use of protective glasses and gloves that are specially designed to reduce x-ray exposure.
Consideration should be given to the use of protective glasses and gloves that are specially designed to reduce x-ray exposure.Terminology
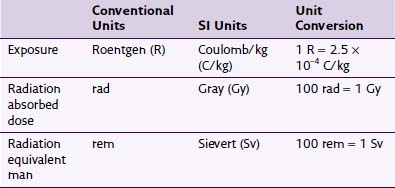
Any discussion of radiation safety requires a basic understanding of the nomenclature specific to this field. The literature is inconsistent in its use of units, with no standardization on using conventional or SI units. Fortunately, for the purposes of the clinician using fluoroscopy, many of these units can often be considered equivalent. Exposure is a quantity of radiation intensity. It is expressed in the conventional units of Roentgen (R) and the SI units of Coulomb/kg (C/kg). The energy absorbed from the exposure is described in conventional units as radiation absorbed dose (rad) and in SI units as Gray (Gy). Different types of radiation cause different biologic effects despite having similar absorbed doses. To predict the biologic effect from different types of radiation, rad is converted to radiation equivalent man (rem) or Sievert (Sv) in SI units. This conversion is accomplished by multiplying either rad or Gy by a quality factor unique to the type of radiation. As an example, whereas the quality factor for x-ray radiation is 1, it is 20 for α particle or fast neutron radiation.1 This quality factor of 1 allows exposure, dose, and dose equivalent to be considered equal for practical purposes despite their different meanings and uses, so 1 R ≈ 1 rad ≈ 1 rem. Conversions between units are summarized in Table 11-1.
Radiation Physics
The image produced by the X-radiation can be altered by either modulating the current or voltage of the x-ray tube. A higher tube current (mA) will cause an increase in the number of electrons striking the anode and thus increase the number of x-rays produced. By increasing the voltage (kVp), the released electrons will have higher energy, and thus the X-radiation will have higher energy and penetrance. The amount of radiation reaching the image intensifier over a period of time is called the radiographic density; the higher the amount of radiation, the brighter the image appears on the fluoroscope monitor. In general, a 15% increase in kVp will have the same effect on radiographic density as doubling the mA.2 Modern C-arms incorporate automatic brightness control (ABC) to optimize the brightness and contrast of the image. This is accomplished by automatic adjustment of mA and kVp.1
Background radiation is unavoidable radiation from both natural sources as well as medical procedures. The average individual receives approximately 3.6 mSv/yr with 15% of this coming from medically necessary radiation when averaged across the population.2 The amount of background radiation from natural sources varies according to region.3
Basics of C-Arm Design
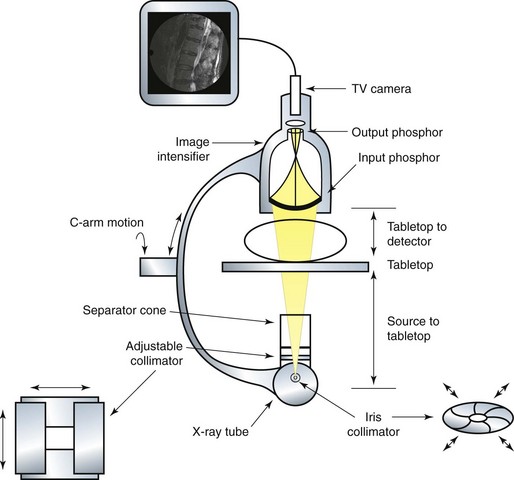
X-radiation is produced in the x-ray tube and directed toward the image intensifier. The image intensifier is composed of two phosphor screens. The input phosphor is spherical, and in combination with the output phosphor, the x-ray image is amplified and converted to visible light, allowing a TV camera to then transmit the image to a screen distant from the image intensifier. Collimation is the process of restricting the x-ray beam to only the clinically important anatomic area. The two types of collimators are iris and adjustable. An adjustable collimator is composed of lead shutters that can be closed to create a rectangular field. An iris variable aperture collimator creates a smaller circular field of radiation. Both collimators reduce the radiation field that reaches the image intensifier and the overall dose to the patient. A basic anatomy of a typical C-arm can be seen in Fig. 11-1.
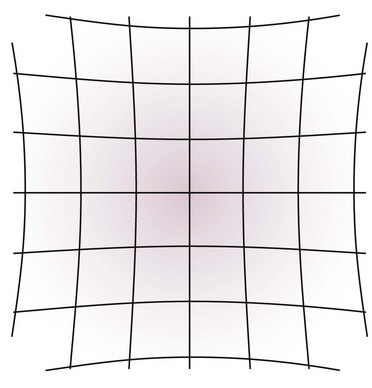
Two types of distortion can occur because of the construction of the image intensifier. Vignetting is the decreased spatial resolution and brightness at the periphery of the fluoroscopic image. The second is pincushion distortion, which is caused by the spherical construction of the input phosphor.2 This creates a fisheye effect as signal from the spherical input phosphor is transmitted to the flat output phosphor. A visual description of this effect can be seen in Fig. 11-2. Both of these distortions can be avoided by placing the anatomic structure of interest in the center of the fluoroscopic image.
Radiation Biology
Damage to the body from radiation occurs from direct cellular damage and indirect damage from creation of reactive oxygen species. Direct cellular damage is most likely to occur in cells that are in the G1 or M phases of the cell cycle. In the G1 stage, proteins are synthesized that prepare the cell for replication. During the M stage, DNA is packaged tightly into chromosomes, and there is an increased risk of a lethal double-strand DNA break.4 Not all radiation damage is lethal to the cell because complex mechanisms repair both single- and double-strand DNA breaks.5 The repair process is usually completed in 1 to 2 hours, so an increase in time between radiation doses causes an increase in cell survival.4
Indirect cellular damage is the result of hydrolysis of water, resulting in production of reactive oxidative species. Two-thirds of radiation-induced DNA damage is attributable to hydroxyl radicals.4 For example, a reactive oxygen species may combine with protein, resulting in the loss of important enzymatic activity in the cell.6 Antioxidants that can scavenge free radicals are therefore important in minimizing this type of damage. Molecules that have sulfhydryl groups and amine groups can scavenge these destructive entities.4
Damage Caused by Radiation
The effects of radiation on the body are divided into deterministic (nonstochastic) and probabilistic (stochastic). Deterministic effects are directly related to the dose received and exhibit a threshold below which the effect does not normally occur and above which the effect is dose dependent. Typically, these effects are related to cell death. An example is found in skin injury from exposure to radiation. An acute dose of 2 Gy causes early transient erythema, which occurs several hours after the dose and resolves within days.7 At an acute dose of 7 Gy, permanent epilation (loss of hair) occurs in about 3 weeks. Table 11-2 gives a more complete enumeration of deterministic effects.8 As described later in this chapter, many of the deterministic effects are not seen because of relatively low doses of radiation administered in the typical interventional pain fluoroscopy suite.
Table 11-2 Skin Entrance Dose Thresholds for Radiation-Induced Skin Injury
| Effect | Dose (Gy) | Onset |
|---|---|---|
| Early transient erythema | 2 | Hours |
| Main erythema | 6 | 10 days |
| Permanent epilation | 7 | 3 weeks |
| Dry desquamation | 14 | 4 weeks |
| Moist desquamation | 18 | 4 weeks |
| Secondary ulceration | 24 | 6 weeks |
| Late erythema | 15 | 8–10 weeks |
| Ischemic dermal necrosis | 18 | >10 weeks |
| Dermal atrophy | 10 | 12 weeks–1 year |
| Induration (invasive fibrosis) | 10 | >1 year |
| Telangiectasia | 10 | >1 year |
| Late dermal necrosis | >12 | >1 year |
From Brown KR, Rzucidlo ER: Acute and chronic radiation injury, J Vasc Surg 53(suppl):15S-21S, 2011.
As the probabilistic risks of radiation exposure have no threshold value, the guiding concept in radiation safety has been to keep doses “as low as reasonably achievable.” This is known as the ALARA concept and is accepted by all regulatory agencies.1 The maximum permissible dose (MPD) is the upper limit of rem one could receive without substantial risk of a clinically significant reaction. Table 11-3 lists the annual MPDs for different anatomic structures. A dose of 25 rem can lead to measurable hematologic depression, and a whole-body total radiation dose of 100 rem can lead to radiation sickness, nausea, fatigue, hemapoietic disturbances, alopecia, and radiation dermatitis.9 It is thought that x-rays may account for 1% of all cancers in the United States.10
Table 11-3 Annual Maximum Permissible Dose Per Target Organ or Area
| Organ or Area | Annual Maximum Permissible Dose (rem) |
|---|---|
| Thyroid | 50 |
| Extremities | 50 |
| Lens of the eye | 15 |
| Gonads | 50 |
| Whole body | 5 |
| Pregnant women | 0.5 |
From National Council on Radiation Protection and Measurements (NCRP): Report No. 116. Limitation of exposure to ionizing radiation, Bethesda, MD, 1993, NCRP Publications.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree