CHAPTER 129
Radial Neuropathy
(Saturday Night Palsy)
Presentation
The patient has injured his upper arm, usually by sleeping with his arm over the back of a chair. He now presents holding the affected hand and wrist with his good hand and reports decreased or absent sensation on the radial and dorsal side of his hand and wrist and inability to extend his wrist (wrist drop), thumb, and finger joints. With the hand supinated (palm up) and the extensors aided by gravity, hand function may appear normal, but when the hand is pronated (palm down), the wrist and hand will drop (Figure 129-1).
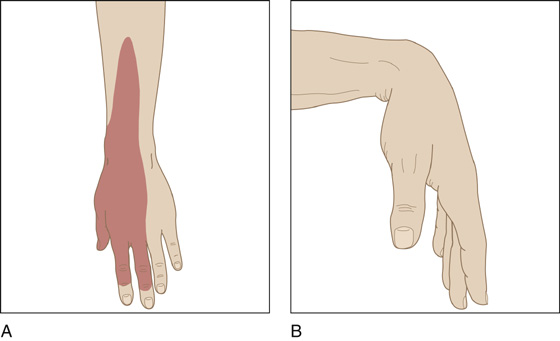
Figure 129-1 A, Decreased or absent sensation on the radial and dorsal sides of the hand and wrist. B, Hand will drop when positioned palm down.
What To Do:
 When there is a history of significant trauma, look for associated injuries. This sort of nerve injury may be associated with cervical spine fracture, injury to the brachial plexus in the axilla, or fracture of the humerus.
When there is a history of significant trauma, look for associated injuries. This sort of nerve injury may be associated with cervical spine fracture, injury to the brachial plexus in the axilla, or fracture of the humerus.
 Document all motor and sensory impairment. When practical, draw a diagram of the area of decreased sensation, and grade muscle strength of various groups (flexors, extensors, etc.) on a scale of 1 to 5. The triceps reflex should be preserved, but the brachioradialis reflex will be decreased or absent.
Document all motor and sensory impairment. When practical, draw a diagram of the area of decreased sensation, and grade muscle strength of various groups (flexors, extensors, etc.) on a scale of 1 to 5. The triceps reflex should be preserved, but the brachioradialis reflex will be decreased or absent.
 Patients with radial palsy often appear to have weakness in addition to radial-innervated muscles. A study of volunteers found decreased strength of handgrip, key pinch, and thumb palmar adduction after radial nerve block. Patients have difficulty spreading the fingers, suggesting weakness of finger abduction, but this is correctable by supporting the fingers or extending the hand when the examiner holds the wrist level with the forearm.
Patients with radial palsy often appear to have weakness in addition to radial-innervated muscles. A study of volunteers found decreased strength of handgrip, key pinch, and thumb palmar adduction after radial nerve block. Patients have difficulty spreading the fingers, suggesting weakness of finger abduction, but this is correctable by supporting the fingers or extending the hand when the examiner holds the wrist level with the forearm.
 If there is complete paralysis or complete anesthesia, arrange for early neurologic consultation and treatment. Incomplete lesions may be satisfactorily referred for delayed follow-up evaluation and physical therapy.
If there is complete paralysis or complete anesthesia, arrange for early neurologic consultation and treatment. Incomplete lesions may be satisfactorily referred for delayed follow-up evaluation and physical therapy.
 Construct a splint, extending from proximal forearm to just beyond the metacarpophalangeal joint (leaving the thumb free), which holds the wrist in 90-degree extension (Figure 129-2). This and a sling will help protect the hand, also preventing edema and distortion of tendons, ligaments, and joint capsules, which can result in loss of hand function after strength returns.
Construct a splint, extending from proximal forearm to just beyond the metacarpophalangeal joint (leaving the thumb free), which holds the wrist in 90-degree extension (Figure 129-2). This and a sling will help protect the hand, also preventing edema and distortion of tendons, ligaments, and joint capsules, which can result in loss of hand function after strength returns.
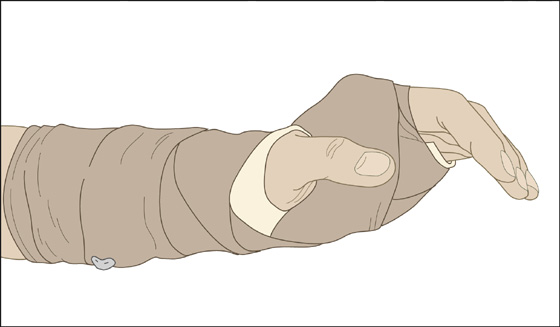
Figure 129-2 Construct a splint that holds the wrist in 90-degree extension.
 Explain to the patient the nature of his peripheral nerve injury; if minor, recovery may take place over a few hours; if more significant, there may be a slow rate of regeneration (about 1 mm per day or approximately 1 inch per month). Stress the importance of splinting and physical therapy for preservation of the eventual return of function. Arrange for follow-up.
Explain to the patient the nature of his peripheral nerve injury; if minor, recovery may take place over a few hours; if more significant, there may be a slow rate of regeneration (about 1 mm per day or approximately 1 inch per month). Stress the importance of splinting and physical therapy for preservation of the eventual return of function. Arrange for follow-up.
What Not To Do:
 Do not be misled by the patient’s ability to extend the interphalangeal joints of the fingers, which may be accomplished by the ulnar-innervated interosseous muscles.
Do not be misled by the patient’s ability to extend the interphalangeal joints of the fingers, which may be accomplished by the ulnar-innervated interosseous muscles.
Discussion
Usually, there is no difficulty in establishing the diagnosis of radial palsy. This neuropathy is produced by compression of the radial nerve as it wraps around the humerus at the spiral groove, where its proximity to the bone makes it susceptible to injury. Most commonly, it occurs when a person falls into a deep sleep, either drug-induced or a result of intoxication, and is held up by his arm thrown over the back of a chair or compressed in some other similar fashion. Because depressant drugs and alcohol predispose a person to prolonged sleep in one position (without the movement typical of normal sleep), the weight of the body may exert pressure on the arm for enough time (usually a period of several hours) to produce wallerian degeneration of nerve fibers. Less severe forms may befall the swain who keeps his arm on his date’s chair back for an entire double feature, ignoring the growing pain and paresis.
If the injury to the radial nerve is in the forearm, sensation typically is spared, despite the wrist drop. The deficient groups will be the wrist ulnar extensors as well as the metacarpophalangeal extensors. A high radial palsy in the axilla (e.g., from leaning on crutches) will involve all of the radial nerve innervations, including the triceps.
In many circumstances, this condition gives rise to a temporary neuropathy or plexopathy, which generally resolves within hours or days. In most cases, the moderate to severe Saturday night palsy resolves spontaneously and completely over the course of a few months. Pain control, a wrist splint, and passive range-of-motion exercises are usually sufficient treatment.
It should be kept in mind though, that if the compression is severe and prolonged, a more grave form of this condition known as “crush syndrome” may occur. Skeletal muscle injury, brought about by protracted immobilization, leads to muscle decay, causing rhabdomyolysis, which may in turn precipitate acute renal failure. This condition is potentially fatal and has an extremely high morbidity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


