Pulmonary Artery Catheters
Khaldoun Faris
I. GENERAL PRINCIPLES
A. Objectives.
1. Assess left ventricular (LV) or right ventricular (RV) function.
2. Monitor hemodynamic status.
3. Guide treatment with pharmacologic and nonpharmacologic agents.
4. Provide prognostic information.
B. Types.
1. Standard pulmonary artery catheter (PAC).
2. Pacing PAC.
3. Continuous cardiac output PAC.
4. Continuous mixed venous O2 PAC.
5. RV ejection fraction PAC.
II. INDICATIONS
A. Cardiovascular disease.
1. Myocardial infarction, associated with cardiogenic shock, mechanical complications, or right heart failure.
2. Severe or progressive congestive heart failure.
3. Primary pulmonary hypertension for diagnosis and to guide vasodilator therapy.
4. Severe valvular heart disease.
5. Shock states.
6. Cardiac tamponade.
B. Perioperative period.
1. Cardiac surgery.
2. Aortic surgery.
3. Liver transplant.
4. Major abdominal and thoracic surgery in the setting of severe or unstable cardiac status.
C. Critical illness.
1. Major trauma and burns.
2. Severe sepsis and septic shock.
3. Acute renal failure.
4. Decompensated cirrhosis.
5. Acute respiratory distress syndrome (ARDS) with multiple organ dysfunction.
6. Severe head injury with refractory intracranial hypertension.
7. Cerebral vasospasm.
8. Severe preeclampsia/eclampsia.
III. PROCEDURE
A. Equipment.
1. The standard catheter length is 110 cm, and the most commonly used external diameters are 5 or 7 Fr.
2. A balloon is present 1 to 2 mm from the tip; when it is inflated with air, it guides the catheter from the greater intrathoracic veins through the right heart chambers into the pulmonary artery (PA).
3. The standard PAC used in the intensive care unit (ICU) is a quadruple-lumen catheter that has a lumen containing electrical leads for a thermistor positioned at the catheter surface, 4 cm proximal to its tip. The thermistor measures PA blood temperature and allows thermodilution cardiac output measurements.
4. A five-lumen catheter allows passage of a specially designed 2.4-Fr bipolar pacing electrode probe through the additional lumen for intracardiac pacing.
5. Continuous mixed venous oxygen saturation measurement is clinically available using a fiberoptic five-lumen PAC.
6. Continuous cardiac output can be measured by catheters equipped with a filament located in the RV portion of the catheter and a rapid response thermistor at the distal end. Pulse-heating currents are applied to the filament randomly, and temperature changes are detected by the thermistor.
7. Catheters equipped with fast-response (95 ms) thermistors allow determination of right ventricle ejection fraction (RVEF) and RV systolic time intervals.
B. Technique.
1. The insertion procedure of the standard PAC is discussed here. The insertion of the other types of PACs is beyond the scope of this chapter.
2. A time-out is performed to ensure “correct patient and side,” and informed consent has been obtained if appropriate.
3. Central venous access using the appropriate size introducer sheath must first be obtained using sterile technique including maximum barrier precautions (see Chapter 2).
4. Continuous monitoring of the electrocardiogram (ECG) and pressure waveforms of the catheter is required, as well as equipment and supplies for cardiopulmonary resuscitation.
5. Flush all lumens of the catheter with normal saline.
6. Insert the catheter in the sterile sleeve adapter and pull the adapter proximally.
7. Pass the catheter through the introducer sheath into the vein and advance it, using the marks on the catheter shaft indicating 10-cm distances from the tip, until the tip is in the right atrium.
8. This maneuver requires advancement of approximately 35 to 40 cm from the left antecubital fossa, 10 to 15 cm from the internal jugular vein, 10 cm from the subclavian vein, and 35 to 40 cm from the femoral vein.
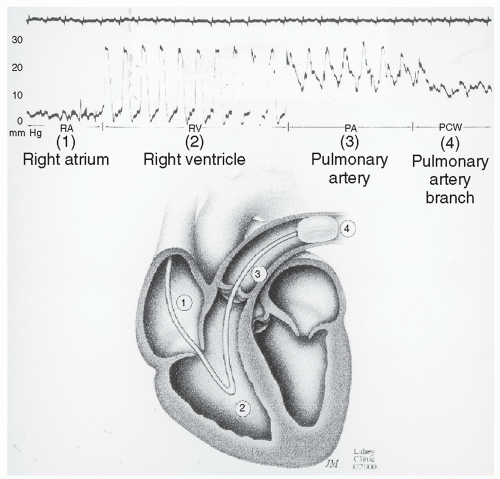
9. A right atrial waveform on the monitor with appropriate fluctuations accompanying respiratory changes or cough confirms proper intrathoracic location (Fig. 4-1).
10. With the catheter tip in the right atrium, inflate the balloon with the recommended amount of air.
a. Inflation of the balloon should be associated with a slight feeling of resistance—if it is not, suspect balloon rupture and do not attempt further inflation or advancement of the catheter until balloon integrity has been properly reevaluated.
b. If significant resistance to balloon inflation is encountered, suspect malposition of the catheter in a small vessel; withdraw the catheter and readvance it to a new position.
c. Do not use liquids to inflate the balloon because they may be irretrievable and could prevent balloon deflation.
11. With the balloon inflated, advance the catheter until an RV pressure tracing is seen. Continue advancing the catheter until the diastolic pressure tracing rises above that observed in the RV (diastolic step-up), thereby indicating PA placement. Raising the head of the bed and tilting
the patient to the right will facilitate passage of the catheter through the RV and reduce the risk of arrhythmias.
the patient to the right will facilitate passage of the catheter through the RV and reduce the risk of arrhythmias.
12. Advancement beyond the PA position results in a fall on the pressure tracing from the levels of systolic pressure noted in the RV and PA. When this is noted, record the pulmonary artery occlusion pressure (PAOP) and deflate the balloon.
13. Phasic PA pressure should reappear on the pressure tracing when the balloon is deflated. If it does not, pull back the catheter with the deflated balloon until the PA tracing appears.
a. Carefully record the balloon inflation volume needed to change the PA pressure tracing to the PAOP tracing.
b. If the inflation volume is significantly lower than the manufacturer’s recommended volume or if subsequent PAOP determinations require decreasing balloon inflation volumes as compared with an initial appropriate volume, the catheter tip has migrated too far peripherally and should be pulled back immediately.
14. Most introducers have a valve that can be tightened to secure the catheter in the correct PA position. To avoid catheter kinkage, the valve should not be tightened too much.
15. Order a chest radiograph to confirm the catheter’s position; the catheter tip should appear no more than 3 to 5 cm from the midline.
16. Fluoroscopic guidance by an experienced operator may be required to insert the PAC in certain disease states such as severe tricuspid regurgitation.
IV. POSTPROCEDURE CONSIDERATIONS
A. Pressure and waveform interpretation.
1. Normal resting right atrial pressure is 0 to 6 mm Hg.
2. The normal resting RV pressure is 17 to 30/0 to 6 mm Hg.