Introduction
Psychiatric emergencies are acute changes in behavior that negatively impact a patient’s ability to function in his or her environment. Often such patients are in a state of crisis in which their baseline coping mechanisms have been overwhelmed by real or perceived circumstances. In dealing with such emergencies, the emergency physician faces many challenges and must prioritize his or her clinical efforts toward four main concerns.
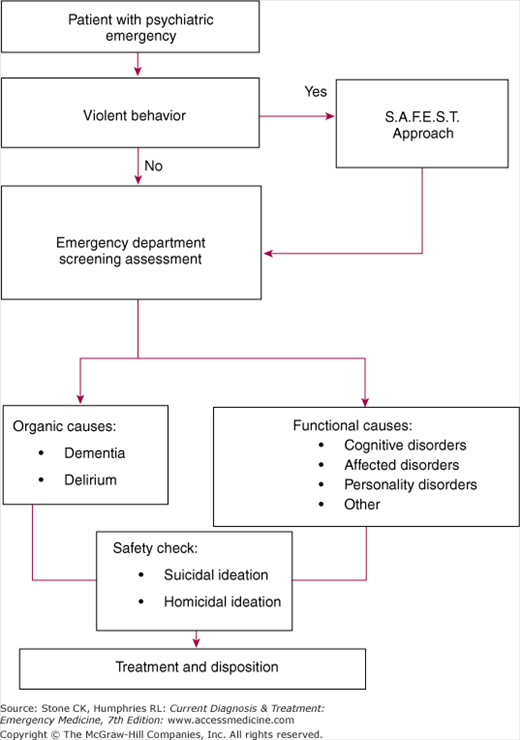
First, the physician must ensure his or her own safety and the patient’s well-being if violence or agitated behavior is present. Second, the physician must perform an effective screening assessment, probing for organic causes and completing a psychiatric safety check. The screening assessment ensures that there is no underlying medical cause for the patient’s condition, either initially inducing the aberrant behavior or evolving as a consequence of that behavior (eg, malnutrition or dehydration). The screening assessment also involves a psychiatric safety check to explore for suicidal ideation, homicidal ideation, or patients’ inability to care for themselves. Third, the physician must ensure that the patient receives appropriate psychological support and medical treatment, even if the treatment needs to be provided without the patient’s consent. Lastly, the physician must determine the appropriate disposition for the patient.
The algorithm in Figure 49–1 provides a decision-making guide to the management of psychiatric emergencies. This algorithm reflects the four main priorities in patient care and provides a framework for this chapter.
The S.A.F.E.S.T. Approach to Violent or Agitated Patients
The emergency physician may encounter patient who threatens or exhibits violent behavior toward staff. In these cases, it is important to recognize the early warning signs of impending violence and adopt an approach to management that reduces the likelihood of injury to staff and patient. Early warning signs of impending violence include threatening statements, clenched fists, loud vocalizations, shifting body positions toward a fighting posture, agitated movements, and striking inanimate objects. If such behavior is detected, adopt the S.A.F.E.S.T. approach:
- Spacing—Maintain distance from the patient. Allow both the patient and you to have equal access to the door. Do not touch a violent person.
- Appearance—Maintain empathetic professional detachment. Use one primary contact person to build rapport. Have security staff available as a show of strength.
- Focus—Watch the patient’s hands. Watch for potential weapons. Watch for escalating agitation.
- Exchange—Delay by calm, continuous talking is crucial to permit de-escalation of the situation. Avoid punitive or judgmental statements. Use good listening skills. Target the current problem or situation in order to find face-saving alternatives for resolution and to elicit the patient’s cooperation with treatment.
- Stabilization—If necessary, use three stabilization techniques to get control of the situation: physical restraint, sedation, and chemical restraint.
Physical restraint—Once the situation permits, it is advisable to restrain any violent or agitated person to ensure safety. This activity is best done by trained security personnel who should also search the patient for weapons. Implement documentation that indicates the need for restraints and provides a record of safety checks on the restrained patient.
Sedation—If agitation persists, sedation is best achieved by administering lorazepam, 1–2 mg intramuscularly or intravenously. Dosing may be repeated to achieve effect while monitoring for side effects including respiratory depression.
Chemical restraint—Chemical restraint is best achieved with neuroleptics. For patients not responding to sedation, haloperidol 5 mg may be administered intramuscularly. In elderly patients, it is best to start with lower dosing and increase by 1–2-mg increments. Dosing may be repeated every 30 minutes until the patient is in more control. Be alert for the emergence of extrapyramidal symptoms, seizure activity, or neuroleptic malignant syndrome.
- Treatment—Once the patient is more manageable, initiate treatment based on the patient’s symptoms. The patient may refuse treatment and may need to receive treatment involuntarily in order to ensure his or her safety.
Emergency Department Screening Assessment
Focus on precipitating causes and circumstances that brought the patient to the emergency department. It may be necessary to elicit information from multiple sources such as family, friends, or ambulance personnel. Other key topics include previous psychiatric treatment, seizure disorders, polysubstance abuse, and any recent suicidal attempts including possible ingestions.
Perform a thorough physical examination, including neurologic assessment. Complete vital signs are essential. Look for physical clues to the source of an altered mental status, such as evidence of head injury, drug use, or toxidromes. Assess the patient for adverse consequences of his or her behavior such as malnutrition or dehydration.
It is important to document the mental status examination in patients presenting with psychiatric emergencies. The mental status assessment should probe for global functioning, thought disorders, mood disorders, and personality disorders.
Assess the patient for general orientation (person, place, time, reason for visit), memory (short and long term), judgment, and concentration.
Assess the patient for abnormal thought content such as hearing voices, experiencing command hallucinations, or having paranoid thoughts.
Assess the patient for evidence of depression or mania. Compare the appropriateness of the patient’s stated mood with his or her overt affect. Look for clues such as emotional lability or unbalanced emotional extremes.
Try to assess whether the patient’s current behavior is an acute psychiatric event that represents a decompensation in his or her normal functioning or a representative sample of a maladaptive pattern of behavior derived from an underlying socially inappropriate personality matrix.
The utility of screening tests remains a controversial topic. Recent American College of Emergency Physician (ACEP) guidelines recommend directing laboratory evaluations based on history and physical findings. Routine testing of all patients is very low yield and is not necessary for Emergency Department assessment. Given these recommendations, the following studies may be helpful in the evaluation of patients presenting with psych emergencies if the history and physical suggests an organic cause:
- Electrolyte panel with glucose
- Pulse oximetry
- Toxicology screen (blood and urine)
- Blood ethanol level
- Liver function tests
- Computed tomography (CT) scan of the head
- Electrocardiogram (ECG)
- Thyroid function tests
The etiology of psychiatric emergencies involves the classic triad of brain, mind, and behavior. Often a patient presents with an alteration in his or her behavior manifested as change in mental state, level of functioning, mood, or personality. The emergency physician must distinguish between those patients needing medical treatment for an organic problem affecting the brain (eg, delirium or dementia) and those individuals who would benefit from psychiatric treatment for a functional problem of the mind (eg, thought disorder, mood disorder, or personality disorder).
Traditional psychiatry involves the diagnosis and treatment of functional entities. The psychiatric emergency, however, is an acute, undifferentiated presentation of altered behavior that may result from either functional or organic conditions. In fact, sometimes both types of problems coexist in the same patient. The emergency physician must consider all these possibilities, first ruling out organic conditions before diagnosing functional entities that may require psychiatric care. This is often referred to as “medical clearance”.
Many patients present to psychiatric facilities with acute altered behavior. Emergency physicians often provide the first and possibly only medical evaluation the acute psychiatric patient is likely to receive. In addition, psychiatric facilities may not be equipped with either appropriate staff or equipment to provide comprehensive medical evaluation and/or treatment. Emergency department personnel are tasked with excluding a medical etiology for the patient’s symptoms. Unfortunately, the term “medical clearance” can imply different things to psychiatric staff and emergency staff. Emergency staff must determine the appropriate evaluation based on a focused history and physical. No agreed upon standard exists and therefore emergency physicians must use patient presentation to determine the appropriate evaluation.
Organic disorders may be very difficult to differentiate from behavioral changes caused by a functional condition. However, some factors may point to an organic cause of the behavioral change. Organic causes often are acute in onset, whereas functional disorders develop over time. Visual hallucinations are much more common with organic syndromes or medical illness than are auditory hallucinations. Age of onset may also be a clue. Patients presenting with functional etiologies are usually younger, typically 12–40 years of age. Exceptions are always possible, but older patients need special consideration when disease is being attributed to functional origin, especially when no history of previous psychiatric disorder is present. Patients with organic disorders generally present with emotional lability, whereas patients with a flat affect usually have functional disease. Finally, any abnormality in vital signs or features of a toxidrome should immediately point to an organic cause.
The emergency physician must directly assess for the presence of suicidal or homicidal ideation in all patients presenting with a psychiatric emergency. In general, the patients’ ability to care for themselves is a cardinal component of the initial assessment.
The management of suicidal ideation involves recognition of the problem, an assessment of risk, and development of a treatment plan.
Patients with suicidal ideation may present with an obvious attempt to cause self-harm. However, suicidal patients may present to the emergency department more indirectly, with suicidal ideation as the underlying cause behind other presentations, such as through an automobile accident. The best screening approach involves general questions about the patient’s emotional state. Inappropriate, irrational, or dysphoric answers should prompt further investigation, culminating in direct questions about suicidal intent.
Several factors increase the risk of suicide. Patients with prior suicide attempts are at increased risk. Patients who employ violent means are more serious about their intent. Existence of a detailed plan reflects significant commitment to following through with the suicide attempt, particularly when coupled with a depressed emotional state or altered mental status. Poor social support or inadequate coping mechanisms also put patients at increased risk.
Admit patients who have clear suicidal ideation, unless immediate psychiatric evaluation is an option. The admission may be directly to the psychiatry service or to the medical service with a psychiatry consult. It may be necessary to sign involuntary admission holds on patients who resist efforts to ensure their safety. Patients with suicidal ideation should be monitored closely at all times, ideally with a one-to-one sitter. They should be given emotional support throughout their stay and their environment should be screened for any potential means of suicide.
Patients expressing homicidal intent require special measures to ensure staff safety and the safety of the third party threatened by the patient. The patient’s threats should be believed, particularly if he or she has a specific plan. The third party, if specifically named, should be contacted through appropriate authorities to ensure his or her safety. The patient should be closely monitored by security personnel, with restraints, as indicated, in a setting devoid of potential weapons. Acute psychiatric consultation is mandatory.
Organic Causes for Psychiatric Emergencies
Patients with acute behavior, mood, or thought disturbances must be medically evaluated for the presence of dementia or delirium. Dementia is a chronic, progressive alteration in memory associated with cognitive decline, agnosia (inability to recognize familiar objects), apraxia (inability to perform tasks), and aphasia (defective language function). Alzheimer’s disease is the classic type of dementia. However, infections, such as HIV, and other neurologic conditions, such as stroke, can also cause dementia.
Delirium, by contrast, is an acute disturbance in consciousness. It may also involve cognitive decline, but the patient’s level of consciousness is decreased, unlike in dementia. Delirium has a short onset and usually a fluctuating course.
Alzheimer’s disease is the most common type of dementia. It starts with memory loss affecting recent memory. Long-term memory is usually preserved. As the disease progresses, more cognitive deficits become apparent until the patient is no longer able to function. History and physical examination are the most important contributors to the diagnosis. Magnetic resonance imaging (MRI) is an important adjunct.
Acetylcholinesterase inhibitors (eg, tacrine, donepezil) are used to increase central nervous system (CNS) levels of acetylcholine. This treatment helps to delay the progression of disease in some patients. However, no agent is currently available that can prevent the ultimate progression of Alzheimer’s disease.
Multiple medical problems can cause a delirious state, which may be confused with psychosis. Drug intoxication or withdrawal; infection; and endocrine, metabolic, neurologic, and cardiopulmonary disturbances are most often implicated.
See Chapter 47.
The stimulant drugs such as cocaine and amphetamines, including MDMA (Ectasy), can cause symptoms of behavioral and personality disturbance. These drugs can also induce someone with a compensated psychiatric illness such as schizophrenia to decompensate. Therefore, when evaluating a patient with mental status changes and bizarre behavior, the physician should determine whether stimulant drugs are present. The diagnosis is based on history of substance abuse, characteristic signs, and a positive drug screen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree