KEY POINTS
The initial sign that a malignant hyperthermia crisis is developing is a rise in end-tidal CO2 levels. The treatment of choice is dantrolene.
Twitch monitors should be utilized to ensure that neuromuscular blockade has been adequately reversed as physical examination is not generally adequate. Residual neuromuscular blockade is an important cause of postoperative respiratory failure.
Unfractionated heparin for DVT prophylaxis offers no benefit for trauma patients. Low-molecular-weight heparin should be used unless contraindicated.
Patients with systolic anterior motion (SAM) of the mitral valve or significant ventricular hypertrophy should undergo fluid resuscitation as the mainstay of post-cardiac surgery management as inotropes may cause severe obstructive cardiogenic shock.
Cardiac tamponade, massive hemothorax, and right heart failure are significant causes of morbidity and mortality in cardiac surgery. Their presentations can be similar and distinguishing between the different causes is imperative to ensure that proper medical and/or surgical treatment is performed.
Inhaled pulmonary vasodilators are important adjuncts in the treatment of acute right heart failure in the postoperative period as they do not have the systemic effects of hypotension and hypoxemia seen with intravenous agents.
β-Blockers and amiodarone are the main agents used for perioperative prevention of atrial fibrillation in cardiac surgery patients.
Augmentation of mean arterial pressure, maintenance of cardiac output, and monitoring and drainage of cerebrospinal fluid with a lumbar drain are important adjunctive therapies to reduce rates of paralysis following aortic surgery.
Cardiac herniation following pneumonectomy and pericardial patch breakdown is characterized by acute obstructive shock, jugular venous distention, and discoloration of the upper torso. The mortality rate is 50%; therefore, immediate recognition and surgical treatment are imperative.
Bilateral recurrent laryngeal nerve injury leads to acute, emergent respiratory failure requiring intubation, followed by tracheostomy.
OVERVIEW OF POSTOPERATIVE CRITICAL CARE
The principles of postoperative management for general care and postoperative emergencies are often discussed only in depth in large surgical texts or specialized surgical service texts. Any critical care provider who cares for general surgical, cardiothoracic, neurosurgical, and trauma patients should have a basic understanding of routine postoperative care, including understanding of surgical drains, chest tubes, and wound care. As with all aspects of patient care, communication with nursing, ancillary personnel, and other health care providers is essential to appropriate recognition and care for the emergencies. Communication with the anesthesia and surgical teams bringing the patient to the ICU should occur to ensure that the critical care provider understands what surgical procedure occurred, what events are expected, and what potential complications to watch for. The critical care unit should furthermore have appropriate equipment to assist in recognition and, when appropriate, treatment of these emergencies. Much of the critical care management of postoperative and trauma patients is similar to nonsurgical critically ill patients. This chapter is designed to assist in specific postoperative and trauma situations not covered elsewhere in this textbook.
IMMEDIATE POSTANESTHESIA CARE
When a patient presents to the ICU following surgery, they are unresponsive because of a variety of medications, including volatile anesthetics, benzodiazepines, narcotics, and neuromuscular blockers. Volatile anesthetics tend to dissipate quickly but can maintain their effects for 20 to 60 minutes postoperatively. The speed of emergence is directly proportional to alveolar ventilation, but inversely proportionate to solubility of the agent within the blood. The longer the anesthesia time, the more total tissue uptake occurs, which can affect the duration of time it takes to emerge from the anesthesia. Recovery is generally fastest with desflurane and nitrous oxide and slowest with isoflurane. If the patient has been hypoventilated during and after the surgery, this may also lead to delayed emergence from anesthesia. Narcotics and benzodiazepines have variable duration of action depending on the amount administered during surgery. Recovery from intravenous anesthetics is mainly dependent on redistribution rather than the elimination half-life of the drug. As the total dose administered during an anesthetic application increases, cumulative effects become apparent and lead to prolonged emergence; the half-life will become more involved in the duration of emergence. Propofol and remifentanil lead to the shortest emergence time. Advanced age, renal impairment, and/or hepatic disease can all affect duration of action of IV anesthetics. An adequate amount of time should be given for these to wear off before becoming unduly concerned about mental status. The anesthetic record is an excellent source, as well as the verbal report from the anesthesia team, which is imperative to obtain on patient arrival to the ICU.
Neuromuscular blockade can have prolonged duration of action in some cases and should be considered when a patient is unable to move adequately or cannot hold up the head for 10 seconds. In some instances, a false sense that the blockade has worn off can be seen and, following extubation, the patient has difficulty maintaining ventilation without assistance. A train-of-four twitch monitor should be used in determining whether paralysis has been completely reversed. If paralysis is persistent, neostigmine (0.5-2 mg) and glycopyrrolate can be used to reverse the action of the neuromuscular blockers. The diaphragm has been shown to be the most resistant skeletal muscle with regard to effects from neuromuscular blockade. It also tends to be the first to recover. Patients who were able to hold either their head or leg up for 5 seconds in a study by Pavlon were able to perform all airway-protection tests necessary for postoperative extubation.
Delayed emergence can occur because of several reasons, the most common being residual anesthetic, sedative, and analgesic drug effects. Emergence can also be delayed by electrolyte abnormalities such as hyperglycemia and hyponatremia. Use of other sedating or interacting agents such as alcohol or recreational drugs prior to anesthesia may also contribute. If the length of emergence becomes prolonged, then naloxone in 0.04 mg increments and/or flumazenil in 0.2 mg increments can be given to rule out opioid or benzodiazepine effects, respectively.1
Patients may become restless before they are fully responsive or they may experience disorientation, anxiety, and pain. Generally, this is self-limited; however, hypoxemia, acidosis, hypotension, bladder distention, or other complications should be considered and evaluated. Despite this restlessness, it is usually possible to have patients follow commands and participate in working toward extubation. Small doses of narcotics and/or benzodiazepines may be necessary to help relax the patient enough to avoid self-harm, self-extubation, or other complications. This usually can be accomplished without causing further sedation.2 Generally, the use of low-dose fentanyl or morphine for pain and/or 0.5 to 1 mg of midazolam intermittently can control agitation. In most cases, agitation or somnolence should improve within 30 to 60 minutes with appropriate management and monitoring. If not, then conditions such as sepsis, shock, and encephalopathy should be considered. In these patients, decisions regarding extubation can be difficult.
Patients returning from the operating room frequently have moderate to severe hypothermia. The causes are multifactorial and include IV fluids and blood products that are not warmed prior to infusion, cool air temperature for operating personnel comfort, vasodilation from the use of volatile anesthetics, large open wounds and raw surfaces, and evaporation. Although there may be times when hypothermia is useful, for example, post-cardiac arrest or anoxic brain injury, the majority of postoperative patients should be returned to normothermia.3 Postoperative hypothermia has been shown to worsen coagulopathy, increase transfusion requirements, increase susceptibility to infection, increase risk of cardiac ischemia, and increase shivering and overall discomfort.4 The goal should be rewarming during emergence and on presentation to the ICU. Forced-air rewarming devices should be used to normalize temperature (36°C) and reduce shivering, in order to reduce the risk of further complications.5
In the immediate postoperative period, many patients can be extubated quickly following surgery.6,7 However, several factors in addition to anesthetic reversal need to be considered prior to extubation including plans to return to the operating room in the near future, ongoing bleeding, inadequate resuscitation, or severe metabolic acidosis. The overall ease of intubation and any complications during the initial intubation should also be considered. Patients with neurological damage who are unable to follow commands and/or have an absent gag and cough reflex suffer increased rates of reintubation and increased risks of morbidity. If patients are unable to be extubated within the immediate postoperative period, daily reassessment should be performed. Assessments of physiologic reserve are paramount to ensure successful extubation. Patients should breathe without mechanical assistance to allow assessment of respiratory rate, vital signs stability, end-tidal carbon dioxide levels, and comfort. If trauma is involved, especially in the case of chest wall damage, assessment of coordination of the chest wall with the respiratory pattern is important, as is ability to control pain.
Malignant hyperthermia (MH) was first reported in 1962 after Denborough described a series of anesthetic deaths within a particular family. MH is a hypermetabolic crisis that is induced by certain anesthetic agents, including succinylcholine, sevoflurane, isoflurane, desflurane, and halothane. A familial relationship does seem to exist but is not a reliable indicator. The overall incidence is rare—approximately 1 in 15,000 patients.1 Approximately 50% of those who experience an MH crisis have had a previous anesthetic agent without complication. The frequency is reduced in women and patients older than 50. Pediatric patients and those with musculoskeletal disorders including myotonia, osteogenesis imperfecta, King-Denborough syndrome, and Duchenne muscular dystrophy have the highest prevalence. In addition, certain surgical procedures have also associated with an increased risk including repair of cleft palate, tonsillectomy and adenoidectomy, repair of ptosis, strabismus correction, and orthopedic procedures.1 Unrecognized MH carries an approximately 80% mortality, while treated aggressively, the mortality rate is only 10%.
The earliest indication that an MH crisis is developing is an increase in end-tidal carbon dioxide levels. Fever, tachycardia, tachypnea, and rigidity of the masseter muscle (trismus) will generally develop in patients. Patients will then quickly become unstable if not aggressively treated; further symptoms and findings will include hypotension, cyanosis, cardiac arrhythmias, and severe hyperpyrexia. As the crisis develops, temperature may raise as much as 1°C to 2°C every 5 minutes.8
The hallmark treatment of MH is dantrolene, which was specifically developed to treat the condition. Dantrolene is a skeletal muscle relaxant that must be administered intravenously. It comes in powder form and must be reconstituted at bedside. In an average 70-kg patient, thirty-six 20-mg vials will be needed for stabilization. After the patient is stabilized, dantrolene is administered at 1 mg/kg every 6 to 8 hours for 1 to 3 days to prevent recurrence during which time patients should remain in the ICU for monitoring. Comprehensive treatment guidelines for MH according to the Association of Surgical Technologists are included in Table 112-1.1,9
Association of Surgical Technologists Malignant Hyperthermia Treatment Guidelines9
|
GENERAL POSTOPERATIVE AND TRAUMA CARE AND SURGICAL EMERGENCIES
A complete overview of nutrition in the critically ill patient is discussed elsewhere. Postoperative patients have increased nutritional needs because of wound healing, changes in bowel motility, swallowing, and support of surgical anastomoses. In most postoperative patients who are relatively well nourished, enteral or parenteral support may not be needed unless it is anticipated that oral nutrition cannot be started within 7 days after surgery. In critically ill patients whose metabolic demands are increased, nutritional support may be needed earlier.10 Patients in whom the duration of illness is expected to be 7 or more days should be considered for early nutritional support. Examples of patients include those with severe intra-abdominal sepsis, pancreatitis, major trauma, or burns.
In general, enteral access is the preferred route of administration. It has been associated with reduced gut mucosal atrophy,11 bacterial translocation, decreased length of stay, and decreased rates of infection when compared to delayed initiation of feedings.12,13 In addition, patients who cannot assume normal nutritional requirements by oral feeding alone may need additional enteral nutritional support. Trauma patients with blunt or penetrating abdominal injuries show reduced infection rates when fed enterally, and in burn patients, studies demonstrate that nutrition should be started immediately. Even delaying 18 hours results in a higher rate of parenteral nutrition requirement.14
Even when critically ill, most postoperative patients who have undergone a laparotomy have return of bowel function in the first few days. Gastroparesis can occur and will delay gastric emptying. Clinical signs of gastroparesis include abdominal distention, 500 mL/day of nasogastric tube output, or residual volumes greater than 300 mL in the stomach after feedings. Theoretically, one method to combat this would be to initiate postpyloric feeding,15 but postpyloric feeding has not been shown to decrease ICU length of stay, mortality rate, or pneumonia rate when compared with gastric feeding. Prokinetic agents, such as metoclopramide and erythromycin, can be used with some positive results.16
While most critically ill patients tolerate gastric feedings well, the Eastern Association for the Surgery of Trauma (EAST) outlines which trauma patients warrant postpyloric feedings including patients with severe traumatic brain injury who did not tolerate gastric feedings in the first 48 hours of trauma and patients with abdominal trauma who have undergone laparotomy.17 It is critical that trauma patients are adequately resuscitated or else they may develop intestinal necrosis in the face of direct small bowel feeding.
In cases of acute pancreatitis, the degree of inflammation plays a role in route of nutrition. In mild pancreatitis, enteral nutrition (feeding via a tube into the stomach or small intestine) will not be needed unless oral (taking food by mouth) feeding cannot be tolerated after 5 to 7 days. In patients with severe acute pancreatitis, early enteral feeding should be used. This route has been shown to have reduced infection, need for surgery, and length of stay compared with parenteral nutrition.18 Gastric feedings can be used in most patients with acute pancreatitis.19
Parenteral nutrition has not been shown to reduce morbidity or mortality and it is associated with increased risk of catheter- and noncatheter-related infections.20,21 A recent study by Casaer and colleagues found that those patients where parenteral nutrition was initiated at day 8 or after had a faster overall recovery time and fewer overall complications.22 If bowel function or injury will not allow enteral nutrition or if enteral nutrition is not expected within 7 days, then parental nutrition should be given. It is generally recommended that if patients fail to reach at least 50% of their goal enteral rate by day 7, parenteral nutrition should be started, but the combination of parenteral and enteral nutrition has only demonstrated benefit in malnourished patients.23 Parental nutrition is frequently used in patients with an enterocutaneous fistula where enteral nutrition can worsen fistula healing by increased output. In general, these patients should have complete bowel rest and parenteral nutrition with 1.5 to 2 times the normal nonprotein calorie complement.24
The monitoring and management of drains in the postoperative patient is an important task that is frequently overlooked or not given the attention that it deserves. The surgical team should be queried during the handoff communication with the critical care team regarding the location, type, and purpose of each drain that is in place. Many abdominal surgeries can involve numerous drains in various locations. Sometimes a pictorial representation on the patient chart can help simplify the task of monitoring drain output. Increased or decreased drain output or change in the fluid of the drain can represent significant clinical findings and an understanding of the types and locations of the drains is essential to diagnosing these. For instance, a change in drain content to presence of bile, debris, or stool suggests a leak or anastomotic breakdown.25 A list of commonly used drains, their compositions, mechanisms, and indications for usage is included in Table 112-2.
Surgical Drains and Wound Management Systems
| Drain | Composition and Drainage Method | Collecting System | Typical Uses | Photographic Representation |
|---|---|---|---|---|
| Abramson117/sump drain | Passive; triple-lumen sump drain; allows an air vent, suction lumen, and irrigation/medication lumen | Gravity collection bag | Peritoneal cavity removal of large volumes of thick exudates |
®2014 C.R. Bard, Inc., Used with permission. |
| ABThera118 and V.A.C. 119 Systems | Active; continuous negative pressure | 300- 1000 mL graduated container | Negative pressure wound healing and temporary abdominal closure system |
Used with permission. Courtesy of KCI. |
| Blake120 | Active; radiopaque silicone four-channeled drain with channels along the sides with a solid core center | Bulb grenade | Abdominal, neck, breast/soft tissue, or chest exudates | |
| Davol117 | Active; radiopaque, perforated, silicone and PVC drain; variable types: channeled, round, or flat types | 400 mL three-spring evacuator suction | Neurosurgery, head and neck, breast, abdominal, or orthopedic exudates |
®2014 C.R. Bard, Inc., Used with permission. |
| Duet® External Drainage & Monitoring System121 | Passive; translucent or fabricated of radiopaque (barium impregnated) silicone tubing | CSF drainage collecting system with rotating pressure scale | Ventricular and lumbar drain monitoring (both in mm Hg or cm H2O) |
Used with permission of Medtronic, Minneapolis, MN. |
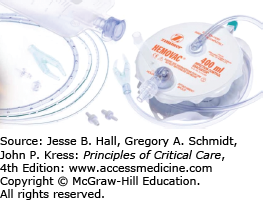
| Hemovac122 | Active; radiopaque, perforated, silicone round drain | 400 mL evacuator and a disposable exudate bag | Neurosurgery, head and neck, breast, abdominal, or orthopedic exudates |
Used with permission of Zimmer, Warsaw, IN. |
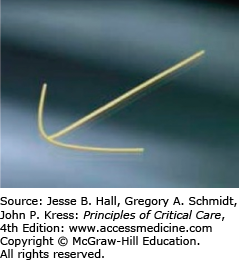
| Jackson-Pratt123 | Active; radiopaque, perforated, silicone and PVC drain; variable types; four-channeled, round, or flat types | Bulb grenade | Abdominal, neck, breast/soft tissue, or chest exudates |
Used with permission of Cardinal Health, Dublin, OH. |
| Malecot117 | Passive; latex drain with four wings | Gravity collection bag | Percutaneous nephrostomy tubes or enteral diversion or access (for bowel perforation drainage or feeding tube) |
®2014 C.R. Bard, Inc., Used with permission. |
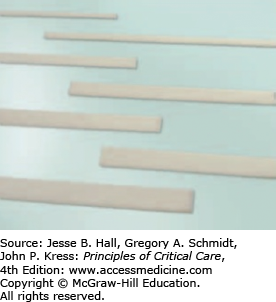
| Penrose117/gravity drain | Passive; flat latex drain | None | Promotes drainage in an open surgical wound; typically perirectally or head and neck |
®2014 C.R. Bard, Inc., Used with permission. |
| PleurX124 | Active; tunneled fenestrated silicone catheter | 500 or 1000 mL vacuum container | Recurrent pleural effusions or malignant ascites | |
| T-tube117 and cholecystostomy tubes | Passive or active | Bile collection bag or bulb grenade | T-tube: placed within the hepatobiliary ducts during open gallbladder procedure to drain bile; cholecystostomy tube: placed within the gallbladder to drain bile |
®2014 C.R. Bard, Inc., Used with permission. |
In general there are passive and active drains. Passive drains provide a route of low resistance for the movement of material out of the body. They work via capillary action and pressure gradients. Examples of passive drains include Penrose, Malecot, and red Robinson drains. Active drains use some sort of external suction device to create negative pressure gradient. Examples of active drain systems include Hemovac, Jackson-Pratt, and Blake drains. They can have their own mechanical drainage system as in the Hemovac drain or be attached to grenade bulb or wall suction.
The drainage of the GI tract is often accomplished through sump drains. These drains draw air into one lumen and then remove fluid through another. The air “sump” system avoids drawing mesentery and bowel into the drainage system. Drains are generally soft and flexible and are made of either a silicon material or polyvinyl chloride (PVC). Drains can be either prophylactic or therapeutic in their purpose. If the drain is placed for therapeutic reasons, it is to remove pus, debris, and fistula drainage, or to prevent premature closure of a wound. If the drain is placed for prophylactic reasons, it is designed to prevent the accumulation of bile, pus, intestinal fluid, or blood or to monitor for complications of a difficult operation with high risk of anastomotic breakdown.26 The use of drains has decreased over time as there are now multiple randomized controlled trials demonstrating that routine use of drains in many intra-abdominal (including appendectomy, colorectal, and hepatic) surgeries, as well as thyroid and parathyroid surgeries, does not prevent anastomotic leaks or other complications.27 There exists some evidence that drains prevent seroma formation and can also aid in diagnosing anastomotic and biliary leaks following surgery.28 In addition to locations of drains, critical care physicians need to determine from the surgical team whether specific drains should be used for gravity or suction, and what are the expected fluid contents and output.
Specific drains that require special attention and potentially management by the critical care team include intraventricular drains, lumbar drains, and chest (thoracostomy) tubes. Intraventricular catheters (ventriculostomies, external ventricular drain, EVD) are used both to drain cerebrospinal fluid and monitor intracranial pressure. The drainage of cerebrospinal fluid can also be used to decrease intracranial pressure. Although this catheter is effective and necessary, several complications can occur. The risk of hemorrhage is 1% to 6%. It can either be immediate or delayed and can occur at several anatomic locations.29,30 Infection can also occur in any of the spaces where the catheter passes, including skin, osteomyelitis of the calvarium, subdural empyema, meningitis, parenchymal abscess, and/or ventriculitis.31 Infection rates have been reported from 2% to 22%. The literature does not directly support the use of prophylactic antibiotics in patients with these catheters, but clinical practice generally employs their use. The best care for these catheters is to maintain sterile technique, remove them as soon as feasible, and avoid flushing the catheter as this increases risk of infection.29 Care of lumbar drains is similar. Typically these are used post-descending thoracic aortic surgery for improved spinal perfusion and are covered more in depth later in this chapter in the section “Paralysis/Paresis After Thoracic Aortic Surgery.”
Chest (thoracostomy) tubes are ubiquitous to critical care settings. All critical care physicians should have a basic understanding of their management. Chest tubes are placed into the pleural cavity for reasons of draining air or fluid. As a result, they are directed into the pleural cavity based on their intent with tubes placed for effusions placed inferiorly and posteriorly and tubes placed for air placed anteriorly and apically. Sizes vary widely from small pigtail catheters, which can be as small as 3 French to large thoracostomy tubes typically used for large volume hemothoraces posttrauma or post-cardiac surgery (28 French or larger). They can be placed directly into the hemithorax or mediastinum or can be tunneled for long-term drainage, as with the Pleurx catheter. Tubes should be checked for the functionality each day. Tubes placed within the pleural cavity should have condensation in the tubing and should tidal with breathing. “Tidaling” is noting the fluid within the tubing or within the collection chamber to be rising and falling with breathing in accordance with the thoracic pressure variation.
Most chest tube collection systems function on a three-bottle system. This may be confusing as all of three of these chambers are contained within one system, for example, Pleura-Evac. The first chamber is a collection chamber. Pleural collection systems have graduated cylinders to monitor the amount of drainage. In patients who are being examined after trauma or cardiothoracic surgery, volumes >100 mL/h should be discussed with the treating surgeon. The second chamber is passage across a one-way valve through a water-seal chamber. If an air leak is present, then bubbles will be seen in the water chamber. The extent of the leak can be continuous, meaning present at all times or just present with cough or deep exhalation. Finally the third bottle is a suction control chamber. Suction can be applied from −10 to −40 cm of H2O. When no external suction is applied, the system is said to be on “water seal.” Typically chest tubes placed for acute hemothorax or pleural effusion are set to drain at −20 cm of H2O suction, but settings for suction are variable based on the intent of the thoracostomy tube. In general, chest tubes placed after noncardiac thoracic surgery or for pneumothorax should be placed to water seal as soon as possible. Numerous studies have found that placing chest tubes on water seal after a brief period of suction for reexpansion shortens the time to resolution of the air leak.32,33 Air leaks that are greater than four of seven chambers will likely not be able to tolerate a water seal setting and generally must be placed on suction.34 It should be mentioned that a chest tube in a pneumonectomy space should be to a balanced-drainage system or to water-seal. A pneumonectomy chest tube should not be placed to suction because of the risk of acute mediastinal shift.35
The topic of wound care is broad and far-reaching. This discussion will concentrate on initial postoperative dressings and their care, as well as use of vacuum-assisted closure devices. Initial management of wounds involves the placement of a sterile dressing that covers the operative incision. It is recommended to keep this dressing dry and in place for the first 48 hours following surgery. During this initial 48 hours, an epithelial barrier develops over the wound when it has been closed by primary intention. After this initial period, the skin can be cleansed with water, and no further dressing is necessary. Surgical wounds that are left open to heal by secondary intention or that have necrotic tissue, wound exudates, or inflammatory cells do not form this epithelial barrier. Larger, open wounds require a moist, occlusive dressing with frequent removal of exudates and necrotic tissue to allow for appropriate epithelialization. The wet-to-dry dressing provides a moist environment, traps the wound exudates, has bacteriostatic properties, and does not adhere to the wounds. Dressing changes will occur at least twice daily for clean wounds, but more frequently for wounds with a greater amount of exudative and inflammatory material.36 Normal saline solution is used to soak the dressing prior to application. Meshed gauze should be used to provide a mechanical debridement action with dressing changes. Table 112-3 lists commonly used topical agents and negative wound pressure devices along with their mechanisms of action and typical usages.
Topical Wound Management Choices
| Generic Namea | Brand Namesa | Mechanism | Uses |
|---|---|---|---|
| Collagenase | Santyl |
|
|
| Dimethicone | Proshield |
|
|
| Double (polymyxin B/bacitracin) and triple (bacitracin, neomycin, and polymyxin B) antibiotic ointment | Bacitracin, Neosporin |
|
|
| Hydrocolloid | Askina Hydro, Biofilm, Brulstop, DermaFlex, DuoDERM, Hycolloid |
|
|
| Hydrogel | Aquaheal, Carrysyn, DermaGel, Dermagran, Flexigel, Skintegrity |
|
|
| Mafenide acetate | Sulfamylon |
|
|
| Papain/urea | Accuzyme, AllenZyme, Ethezyme, Gladase, Kovia, Pap-Urea |
|
|
| Papain/urea/chlorophyllin copper | Allanfil, Panafil, Papfyll, Ziox |
|
|
| Silver impregnated dressing | Acticoat, Actisorb, Arglaes, Interdry AG, SilverCEL |
|
|
| Silver sulfadiazine | Silvadene |
|
|
Vacuum-assisted wound-closure devices are employed in more and more postoperative patients every day. These devices place the wound under subatmospheric pressures that increase blood flow to the affected area, reduce edema and excess fluid, and increase wound contraction to allow for enhancement of wound granulation. It is important to ensure that wounds are not highly contaminated or do not have significant amounts of necrotic tissue before the use of these devices. Many of these devices use a sponge that is placed over the wound and then covered by an occlusive dressing.37 Reported advantages of this type of therapy include reduced frequency of dressing changes, improved patient comfort, improved efficiency of wound closure, and improved removal of edema fluid. There is some evidence that this negative- pressure therapy may hasten time to grafting or secondary closure, and may help improve wound contraction over abdominal wounds. The use of these devices in complicated abdominal injuries, evisceration, and abdominal compartment syndrome has increased and studies generally show benefit; however, there is also evidence that the devices may increase rates of new enterocutaneous fistula formation.38
The overall supportive care of the patient is also important when attempting to enhance wound care. Both hyperglycemia and hypoglycemia should be avoided. Routine perioperative antibiotic usage should be limited to 24 hours and optimization of nutrition should be employed to further enhance wound healing. Wounds should be evaluated at least daily to monitor for progression of healing and for signs of infection. Most normal surgical wounds will have a small, dry scab and a small border of reactive erythema that will resolve over about a week. Wounds that develop progressive erythema and induration may indicate the presence of underlying cellulitis/wound infection. These should be treated with opening of the incision rather than administration of antibiotics. In most instances, systemic antibiotics are not necessary once the wound has been open and adequately drained, but it is important to ensure that the infection has not spread to the fascia and soft tissues, indicating necrotizing fasciitis.39
All postsurgical patients requiring the ICU should have consideration given for chemical anticoagulation in addition to mechanical mechanisms for deep vein thrombosis (DVT) because they are inherently at risk for the development of this complication.40 Numerous guidelines exist for assistance in determining which anticoagulation is best for certain patient populations; however, in general, prevention should include anticoagulation in any general surgery patient who is considered to be at moderate-to-high risk for DVT. Major risk factors include presence of an operation, physical immobility, age, malignancy, obesity, and smoking history.41
Low-dose unfractionated heparin or low-molecular-weight heparin should be used. Low-molecular-weight heparin can be administered in most cases, unless obesity is a factor. Low-dose unfractionated heparin should be administered three times daily rather than twice daily as previously recommended. In high-risk patients, mechanical devices should be used in addition to anticoagulation. If the risk for postoperative bleeding is considered too high to administer chemical prophylaxis, mechanical prophylaxis should be used until chemical agents can be started. In addition chemical prophylaxis should not be given in the 12 hours proceeding placement or removal of an epidural catheter. Unfractionated heparin administered subcutaneously can be administered while an epidural catheter is in place, but close monitoring for signs of complications should be performed.42
DVT prophylaxis in the neurosurgical patient is imperative but routinely is not started within an appropriate time frame. This is generally because of the hesitation of the neurosurgeons, rather than the intensivists. Because of the increased risk in this patient population, mechanical prophylaxis should be used routinely and initiated immediately. Heparin administered at just 5000 units subcutaneously every 12 hours has been shown to significantly reduce the risk of DVT in neurosurgical patients without increasing the risk of bleeding, as long as there is no active hemorrhage at the time it is initiated.43 In general, chemical prophylaxis should be added within 24 hours of surgery. In many cases, this will have to be worked out on a case-by-case basis with the neurosurgeons.
Trauma patients carry a significant risk for the development of DVT and its complications. It is also one of the most difficult groups for which to provide adequate prophylaxis to prevent DVT from occurring. Risk factors for DVT are numerous and controversial; they include spinal fractures, traumatic brain injury, spinal cord injuries, prolonged mechanical ventilation, multiple operative procedures, and pelvic fractures. Although there are few studies validating specific anticoagulation practices in patients with these factors, there is ample evidence that low-dose unfractionated heparin offers no benefit at all in trauma patients.44 Alternatively, twice daily low-molecular-weight heparin has been shown to reduce the incidence of DVT in trauma patients, but patients should be monitored closely for bleeding complications during its use.45 Patients with active bleeding or at high risk for bleeding complications should receive mechanical prophylaxis; however, there are no data that prove efficacy in this population.46 Sequential compression devices are often contraindicated or difficult to place with extremity fractures, fasciotomies, and external fixators. Trauma patients who are at high risk for venous thromboembolism who cannot receive anticoagulation should be considered for temporary inferior vena cava filter placement.47
As any general surgery resident will tell you, postoperative hypotension is bleeding until proven otherwise. Patients in hemorrhagic shock demonstrate clinical signs of tachycardia, diminished peripheral pulses, coolness of the extremities, anxiety/agitation, and hypotension. Generally, 25% to 30% of blood volume loss occurs before signs of shock are evident, but younger patients or elderly patients receiving certain cardiovascular medications may lose a greater percentage of blood volume prior to demonstrating signs. Most adult patients can lose up to 15% of their blood volume without showing any overt symptoms. Loss of 40% of circulating blood volume is life threatening and generally requires operative (or interventional) control of hemorrhage. The absolute hemoglobin/hematocrit values are not a reliable indicator of hemorrhage as they may be affected by acute whole blood volume loss and/or hemodilution from fluid resuscitation. Trending values are often more helpful in this situation. Hypothermia, acidosis, and coagulopathy, the so-called triad of death, should be corrected unless there is an obvious source of bleeding prior to returning to the operating room as venous hemostasis can often be achieved by simply controlling these factors. Patients should be actively warmed with an external warming device (eg, Bair Hugger) and warmed fresh-frozen plasma, platelets, and cryoglobulin should be administered as appropriate to correct the coagulopathy.
Critical care providers should be aware of potential “sentinel bleeds,” small volume bleeds classically from a sternal wound or peritoneal drains that may represent an ensuing large volume blood loss. Such sentinel bleeds can represent vasospasm of a surgical bed artery, duodenal ulceration into the gastroduodenal artery, or small right ventricular runt that is a risk for rapidly tearing with coughing episode. Responding to these small bleeding episodes can be lifesaving. Again it is imperative that critical care practitioners recognize hypotension in postoperative and trauma patients likely represents hemorrhagic shock. Assessment of the surgical wound or any drains for signs of bleeding should be performed. In the trauma patient, a FAST (focused assessment of sonography for trauma) examination can be performed at the bedside to look for intra-abdominal fluid. A CT scan can be considered, but this takes time and use of contrast dye to assess for extravasation in a patient already at high risk for acute kidney injury. Immediate involvement with the surgical or trauma team is mandatory for operative or interventional decision making.
PRINCIPLES OF OPEN HEART SURGERY AND CARDIAC SURGERY EMERGENCIES
There are entire textbooks dedicated to postoperative management of open-heart surgery. This section will only deal with the most superficial of these and subsequent sections will address specific emergencies that must be recognized by the critical care team managing. A general understanding of cardiac anatomy, cardiopulmonary physiology, and basic operative techniques is a must in order to be able to communicate with the surgical and anesthetic teams that bring the patient to the ICU. Understanding coronary anatomy, divisions of the mediastinal and pleural cavities, and electrical anatomy of the heart are mandatory in order to be able to recognize when complications occur and how they may be a technical or functional complication of the surgery.
The coronary vessels are widely described as three main arteries, although there are only two ostia (origins) that come directly off the aorta. There are three sinuses of Valsalva that protrude just above the aortic valve to the level of the sinotubular junction (STJ). The left coronary sinus is located on the left of the aorta and gives off the left main (LM) artery. The right coronary sinus is located anteriorly and gives off the right coronary artery (RCA). This anatomic location is important to understanding why the right heart is at risk for air embolism as the right coronary artery is the first anterior branch off of the aorta. The noncoronary sinus has no vessels arising from it. The left main artery further divides into the left anterior descending (LAD) artery and the left circumflex artery (LCx). Occasionally, a third vessel comes directly off the left main called the ramus intermedius (RI). The LAD branches into septal perforators that feed the septum and the diagonal vessels that along with the LAD and RI, if present, feed the anterior heart. The terminal LAD feeds the apex of the left ventricle. The LCx is so named since it encircles the heart in a posterior fashion. It gives off obtuse marginal branches that are important to the blood supply of the lateral heart and occasionally the posterior descending artery (PDA) that supplies the mitral valve. The primary branches of the RCA that are bypassed include the posterolateral (RPL) branch feeding the inferior heart and the PDA that supplies the posterior heart and septum. In the majority of the population, the PDA arises from the right coronary artery. The origin of the PDA leads to a description of a heart being right, left, or codominant. A diagram of the main arteries that are bypassed is included in Figure 112-1. Understanding which vessels have been bypassed allows the clinician to interpret findings of postoperative ischemia on ECG as native or graft related, which is important to treatment considerations as will be discussed later.