Key Clinical Questions
Introduction
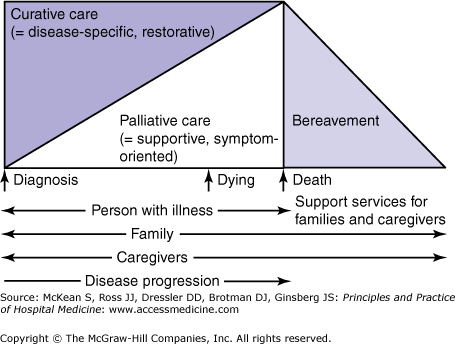
Hospitalized patients with advanced illness have a high burden of symptoms including pain, nausea, and dyspnea. These symptoms can arise from the disease itself as well as from the therapies used to treat it. They can arise at any point in the course of illness and can significantly diminish quality of life. Palliative care is the field of medicine focused on symptom management and improving quality of life for patients living with a life-threatening illness (Morrison & Meier, 2004), whether the goals for care include cure, life prolongation, or living with a chronic illness. Palliative care expertise includes the assessment and treatment of pain and other symptoms, and the relief of suffering caused by thye physical, psychosocial, and spiritual aspects of disease. Unlike hospice, which requires that a physician endorse a six-month prognosis in order for a patient to qualify for service, palliative care, sometimes also referred to as supportive care, is provided in conjunction with curative treatment at any point in the disease trajectory from the time of diagnosis (Figure 215-1). As a patient becomes sicker, palliative care may become a greater focus either because the burden of curative treatments outweighs the benefits or they are no longer effective or because the patient no longer desires them. Palliative care is provided by an interdisciplinary team including physicians, nurses, social workers, pharmacists, psychologists, and chaplains (Morrison & Meier, 2004). Palliative care teams treat not only the patient, but also attend to the needs of the family, understanding that family can include any person the patient identifies as part of his or her support network. Palliative care is provided early in the course of illness and across multiple care settings; therefore, communication among the varied settings and continuity of care is essential to achieving quality care for patients (Table 215-1).
|
While palliative care refers to an approach to care focused on symptom management and improving quality of life, palliative medicine refers to the medical specialty focused on providing palliative care. Despite the emergence of palliative medicine as a formally recognized medical specialty in 2007, all physicians who care for patients with serious and advanced illnesses need to be able to provide appropriate pain and symptom management and identify and treat other sources of suffering in their patients. In order to achieve this goal, all physicians need training in palliative care (Block et al, 2007). Even with such training, physicians will identify some patients who have needs so complex that referral to a specialized palliative medicine team will be appropriate.
Palliative care can be provided in any setting, including hospitals, clinics, nursing homes, emergency facilities, prisons, and home (Table 215-2). Hospice is a common way for people in the United States to receive palliative care at home when they reach the last few months of life. To qualify for hospice benefits, a patient must have a two-physician certified life expectancy of six months or less, and the patient must agree to give up insurance coverage for medical care focused on cure or life prolongation. Hospice is covered by Medicare as well as most health insurance providers. In the United States, the vast majority (> 90%) of patients receive hospice services at home, although the number of patients receiving hospice in nursing homes is growing (Teno et al, 2004). Patients enrolled in home hospice generally have a primary caregiver who is guided by a hospice nurse who visits on an as-needed basis, typically ranging from one to three times per week depending on the patient’s status. Nursing aides provide personal and custodial care typically for about four hours per day. The hospice agency can help the family arrange for other (private pay) custodial care as needed by the patient. Durable medical equipment (hospital bed, wheelchair, commode, etc) and medications related to symptom management are provided at no charge to the patient under the hospice benefit. While hospice providers can manage most symptoms at home, if a crisis occurs, the patient can be admitted to an acute care facility until symptoms are under control.
| Model | Care Setting |
|---|---|
| Consultation service team | Usually in a hospital or nursing home; often includes social work evaluations |
| Combined hospice program and palliative care program | Hospital, nursing home, freestanding hospice inpatient facilities |
| Dedicated inpatient unit | Acute hospitals, nursing homes |
| Hospice-based palliative care in the home | Home |
| Outpatient palliative care practice or clinic | Hospital or private practice |
Pathophysiology
In patients with advanced illness, death is more often the result of sequential systemic changes rather than failure of a single organ. Despite differing courses of diverse illnesses, the dying process is remarkably similar across disease states. Altered carbohydrate, fat, and protein metabolism leads to a catabolic state, and homoeostasis is lost in association with increasing cytokine concentrations. Loss of both adipose tissue and muscle may be severe. Cytokines, including tumor necrosis factor, interleukins 1 and 6, and interferon γ, contribute directly to the weight loss, anorexia, and fatigue that characterize end-stage disease.
Diagnosis and Treatment
The key aspects of palliative care can be divided into eight domains including (1) structure and processes of care; (2) physical aspects of care; (3) psychological and psychiatric aspects of care; (4) social and practical aspects of care; (5) spiritual, religious, and existential aspects of care; (6) cultural aspects of care; (7) care of the imminently dying patient; and (8) ethical and legal considerations. Specific components of these domains are outlined in Table 215-3.
| Area | Examples |
|---|---|
| Physical | Pain, shortness of breath, nausea, fatigue, weakness, anorexia, insomnia, confusion, constipation, treatment side effects, functional capacities, treatment efficacy and alternatives (and patient and family preferences) |
| Psychological/psychiatric | Anxiety, depression, care-giving needs or capacity of family; stress; grief and bereavement risks for the patient and family (ie, depression and comorbid complications); coping strategies |
| Social | Family structure and geographic location; cultural concerns and needs; finances; sexuality; living arrangements; caregiver availability; access to transportation; access to prescription and over-the-counter medicines |
| Spiritual/religious/existential | Spiritual background, beliefs, and practices of the patient and family; hopes and fears; life completion tasks; wishes regarding care setting for death |