KEY POINTS
Development of data integration platforms, Clinical Decision Support Systems (CDSS), telemedicine, and mobile computing applications are rapidly changing the acute hospital environment.
The widespread adoption of health information technology (HIT) is being actively promoted as a tool to facilitate quality and safety of health care.
High cost, indiscriminate data presentation, information overload, and a lack of human factor consideration present significant barriers to wider HIT adoption.
Although HIT adoption improved some elements of quality and safety, there is currently little evidence to prove that HIT adoption is associated with improved patient-centered outcomes.
To get the most from the digitalization of the ICU environment, an integrated and multidisciplinary approach is required. Medical informatics and human factor engineering provide a core methodology and tools for meaningful use of HIT to optimize quality and safety of critical care delivery
INTRODUCTION
It has been estimated that ICU patients are exposed to an average of 178 processes of care every 24 hours.1 Each process is an opportunity for the system of health care delivery to fail. The same study estimated that the rate of failure, in the form of errors, which caused or had the potential to cause harm, was about 1%, or just fewer than 2 per patient per day. This may seem a small number of failures but when one considers severity of illness of ICU patients, it is not surprising that they are particularly vulnerable to those errors. With the declaration of Vienna, the elimination of error in the ICU has been determined to be the single most important priority of the critical care societies of all major developed and developing nations including the Society of Critical Care Medicine in the USA and European Society of Intensive Care Medicine. The combination of health information technology, medical informatics, and an invested team of frontline providers has the potential to play an important role in the redesign of ICU systems of health care delivery. In this chapter, we outline the application of medical informatics in the acute care setting. With examples, we illustrate some of the challenges and opportunities that exist for acute care settings equipped with a comprehensive electronic health record.
HEALTH INFORMATION TECHNOLOGY AND ELECTRONIC HEALTH RECORD
Health care providers and policy makers already support the use of health information technology (HIT) as a tool for providing efficient, high-quality patient care. HIT has been defined as “the application of information processing involving both computer hardware and software that deals with the storage, retrieval, sharing, and use of health care information, data, and knowledge for communication and decision making.” Electronic health record (EHR) is one application of HIT and is perhaps the one most familiar to bedside providers.
Widespread adoption of interoperable HIT has become a top priority for health care systems in both developed and developing nations. In the USA, implementation of HIT is supported by the HITECH provisions of the American Recovery and Re-investment act of 2009.2 Central to the release of funding, the concept of “meaningful use” has been adopted as a mechanism to ensure government funding is directed toward technology that enhances the quality of care delivered to patients. The definition of meaningful use of EHR has only recently been agreed upon by the Center for Medicare and Medicaid Services and is expected to shape the core functionality of HIT in the USA for the foreseeable future.
The adoption of HIT has been advocated on the basis that an overall increase in the quality of care delivery will follow. The major areas of positive impact are reported to include increased adherence to protocol-based care,3 reduction in medication errors, and lower cost.4,5
Despite the potential benefits, the complexity of the effect that widespread adoption of EHR will have on processes of care is largely unknown. Significant knowledge gaps currently exist and are underlined by a number of studies that report a negative impact of HIT on patient-centered care. These negative effects include disruptions to established workflow, increased time spent in documentation and away from patient care, and information overload. The care of patients in the ICU generates vast quantities of data. A significant advantage of a HIT-enabled ICU is that these data are available in a digital form. Digital signatures of patient characteristics, disease state, physician and nursing actions, as well as operational data such as time stamps or entity location offer an unprecedented opportunity to capture data, which facilitates system understanding as well as the development of applications which nudge it toward an optimized state.
ICU patients, however, by virtue of their severity of illness and the large number of processes of care, team members, and technology, may be particularly vulnerable to the potentially disruptive effects of HIT adoption. For example, the implementation of a commercially available computerized physician order entry (CPOE) system in a pediatric ICU was associated with a doubling of adjusted mortality.6 In many cases, technology buries useful information in noise. The hopelessly inadequate performance of bedside alarms manifest as unnecessary interruptions to workflow, frequent manual override without action, and provider fatigue.
In order to realize the “meaningful use” of EHR, it is essential that hospital managers, clinicians, systems engineers, cognitive scientists, and information technology and informatics experts work together to understand how health care providers can best be enabled to provide safe care and improve patient-centered outcomes. In other industries, this multidisciplinary approach has been adopted very successfully and has led to increased reliability, system optimization, and innovation. In a similar manner to a state-of-the art navigational aid, future HIT applications should guide the ICU patient safely from one health state to the next.
BIG PICTURE: WHAT IS MEDICAL INFORMATICS?
Informatics and computers in medicine mean different things to different people depending on their roles and responsibilities. For policy makers, they may facilitate access to benchmark public health data. For hospital administrators, they may provide resource utilization oversight and reportable indicators of quality. For the hospital or community practitioner, they may be used for documentation, patient scheduling, prescribing, and billing. For the patient, they may offer access and the ability to share their own medical data. For researchers, they may provide access to raw data and the tools to analyze it.
Medical informatics is defined by American Medical Informatics Association as, the application of “the principles of computer and information science to the advancement of life sciences research, health professions education, public health, and patient care” and is described as a “multidisciplinary and integrative field focused on health information and communication technologies, and involves computer, cognitive, and social sciences.” The growing importance of this field of practice is such that there are ongoing efforts to establish clinical informatics as a formally recognized medical subspecialty.7
In general, medical informatics has two overall goals8:
Provide solutions for problems related to data, information, and knowledge processing in medicine and health care.
Study the general principles of processing data, information, and knowledge in medicine and health care.
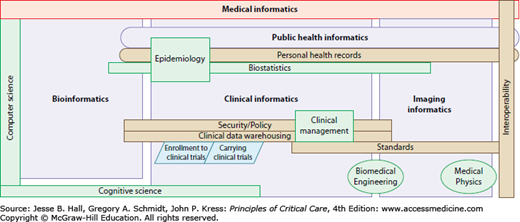
Medical informatics coordinates the activity of many different disciplines and areas of expertise (Fig. 8-1).
FIGURE 8-1.
Schematic relationship between clinical informatics and other disciplines. Medical informatics encompassed many different areas of research and application. Currently four major areas of activity have been identified: public health, bioinformatics, clinical informatics, and imaging informatics.
Top-level medical informatics domains include
Public health informatics: Use informatics on the population level (eg, disease surveillance systems)
Bioinformatics: Processing of molecular and cellular data, such as gene sequences
Clinical informatics: Practice of informatics as it relates to patients and clinicians, including nursing and dentistry
Imaging informatics: Computer applications and information technology in the medical imaging field
BRIEF HISTORY AND CURRENT STATE OF COMPUTER USE IN THE ICU
Using technologies in critical care is not a new concept. A recent review article covers the history of technology implementations in ICU.9 Computer use in the ICU was first reported in 1964 when physicians and engineers began to adapt heart-lung bypass monitors for ECG and blood pressure recording.10 At the same time, the care of critically ill patients was becoming more complex and the development of intensive care as a medical subspecialty began. Even in the early stages of critical care development it was recognized that a large quantity of information was being recorded and processed by bedside practitioners. Studies done during this period demonstrated that nurses spent up to 40% of their time on communication and clerical tasks. Continued medical progress through the intervening decades has led to an exponential growth in available information and expected standards of documentation of processes of care.
With the introduction of microprocessors and personal computers at the end of 1970s health care organizations started using computer applications for administrative and financial tasks.
The first commercial clinical information systems (CIS) in the ICU were developed by monitors’ manufactures to extend functionality, but later the EHR itself became the most important part of CIS. CIS was introduced into ICU practice in the hope that it would increase the accuracy and availability of patient data, reduce the time clinicians spend on documentation while increasing the time available for direct patient care, and facilitate the development of displays, which presented a clearer clinical picture than that represented by the raw data. The success of CIS in these areas is variable. A systematic review (12 articles) of critical care CIS showed that 25% of the studies found an increase, 33% reported a decrease and 42% found no difference in the time providers spent charting.11 Some of the most commonly cited concerns voiced by providers when asked about barriers to CIS implementation include disruption of established workflow, increased complexity, and reduced patient contact.12,13
The early innovators in the clinical informatics field worked in academic settings. Nowadays due to the high cost and complexity of systems development, this activity has shifted to commercial companies. Unfortunately, this trend can lead to a disconnect between the developer and the end user with the promotion and implementation of applications which fail to meet clinician’s needs.
The objectives of ICU information management today are
Automatic capture of information from monitors and devices and transfer for display and storage within CIS. Bedside monitors were the first devices connected to ICU EHR. Later other devices such as ventilators and infusion pumps become connected as well. The automatic data collection reduces data error compared to manual charting
Communication with other hospital systems with links to radiology and laboratory systems
Automatic calculation of raw data into meaningful information
While EHR has the potential to advance the quality of care in the ICU, studies have shown mixed results. Table 8-1 summarizes some of the studies of EHR impact on ICU quality of care.
Studies of EHR Impact on ICU Quality of Care and Their Findings
| Study | Finding |
|---|---|
| A 4-year cross-sectional study of 18 quality measures. | No association between the duration of EMR use and performance with respect to quality of care.33 |
| Study of 3364 hospitals comparing quality of care measures for hospitals with or without fully implemented CPOE systems. | Significant positive association in 5 of 11 quality measures related to ordering medications and in 1 of 9 nonmedication-related quality measures.34 |
| Automated data capture from ICU devices. | Reduces nursing workload.35 |
| Shown to increase time spent in direct patient care.36 | |
| Better automation and usability ICU. | Increased use of HIT was associated with fewer catheter-related infections.37 |
| To assess the effect of CIS on quality of nutritional support in the ICU. | The use of postpyloric feeding tubes and energy (food) delivery increased with CIS, resulting in significantly less patient weight loss.38 |
| To study the impact of the use of a reporting tool derived from an ICU-computerized flow sheet on compliance with JCAHO core measures performance. | Improvements in DVT prophylaxis, GI bleeding prophylaxis, and glucose control in the ICU.39 |
| To compare the impact on patient care of general CPOE system versus a modified system designed specifically for ICU use. | The number of orders written per patient for vasoactive drips, sedative infusions, and ventilation management decreased significantly with the modified CPOE system, however, no impact on ICU length of stay.40 |
| Effect of CPOE on prevention of serious medication errors. | The rate of serious medication errors decreased by 55% after CPOE implementation.14 |
| Impact individual electronic medical record surveillance on the risk of ventilator-induced lung injury. | The exposure to potentially injurious ventilation decreased after the system implementation.21 |
| Prospective trial compared a paper-based ICU versus a computerized. | The ICU computerization resulted in a significant decrease in the occurrence and severity of medication errors in the ICU.41 |
| Study of the impact of implementation of commercially available CPOE on standardized mortality in a pediatric ICU. | CPOE introduction was associated with a doubling of mortality.6 |
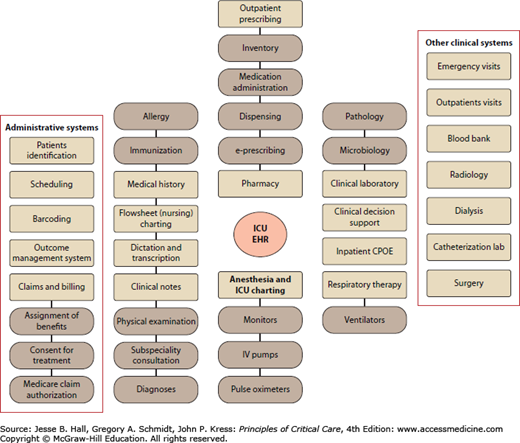
An ICU EMR (terminology is interchangeable with EHR—see glossary) has additional components compared to outpatient and inpatient EHRs. The most notable difference is that the charting module captures high-resolution data from medical devices. ICU charting modules are a vital component of the modern ICU EMR (Fig. 8-2).
Computerized physician order entry (CPOE) can be used to order medications, laboratory tests, radiologic investigations, and consultation services. In many instances, CPOE has been demonstrated to decrease the time taken to complete an order, decrease associated complications (handwriting identification and medication errors), and improve billing management. One of the major reported effects of CPOE is a 55% decrease in serious medication errors.14 In the ICU, the rate of preventable medication errors is almost twice that found in other hospital settings.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree