FIG. 29.1 Head tilt. Patient’s head is tilted backward and neck is hyperextended. This maneuver is contraindicated in presence of possible cervical injury. (Courtesy of Department of Nurse Anesthesia, Virginia Commonwealth University, Richmond, VA.)
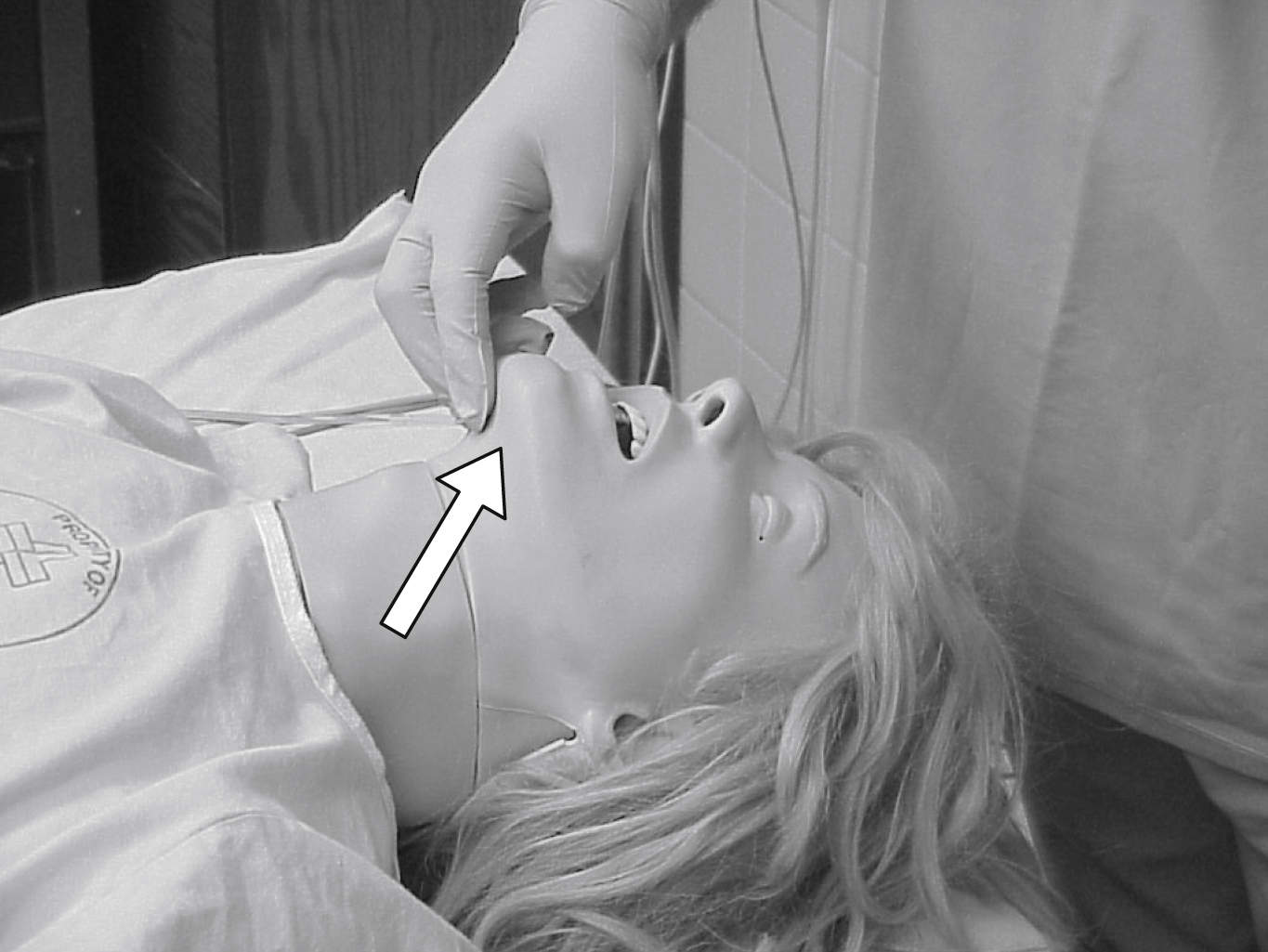
FIG. 29.2 Chin lift. Rescuer places two fingers under bony portion of lower jaw, near chin, and pushes patient’s chin upward with moderate pressure. (Courtesy of Department of Nurse Anesthesia, Virginia Commonwealth University, Richmond, VA.)
Laryngospasm
Laryngospasm is an involuntary partial or complete closure of the vocal cords caused by secretions, stimulation, or irritation of the laryngeal reflexes during emergence. Wheezing, reduced compliance, stridor (partial), paradoxical chest or abdominal movements, and absence of ventilation (complete) are signs and symptoms of laryngospasm. Ventilation is decreased or absent, and oxygenation of the patient is difficult as carbon dioxide builds (PaCO2 increases). Treatment may include airway maneuvers (chin lift/jaw thrust), elevation of the head of bed to maximize respiratory excursion, and application of a bag-valve-mask for continuous positive pressure with oxygen. Secretions need to be carefully removed with suction. The patient may need reintubation to secure the airway if mask ventilation is difficult. Medications may include succinylcholine and can include other neuromuscular blocking agents and lidocaine. When the patient has received a neuromuscular blocking agent, the patient may need sedation to reduce anxiety related to apnea, muscle relaxation, and awareness.

FIG. 29.3 Head tilt and chin lift maneuvers are often done collectively. (Courtesy of Department of Nurse Anesthesia, Virginia Commonwealth University, Richmond, VA.)
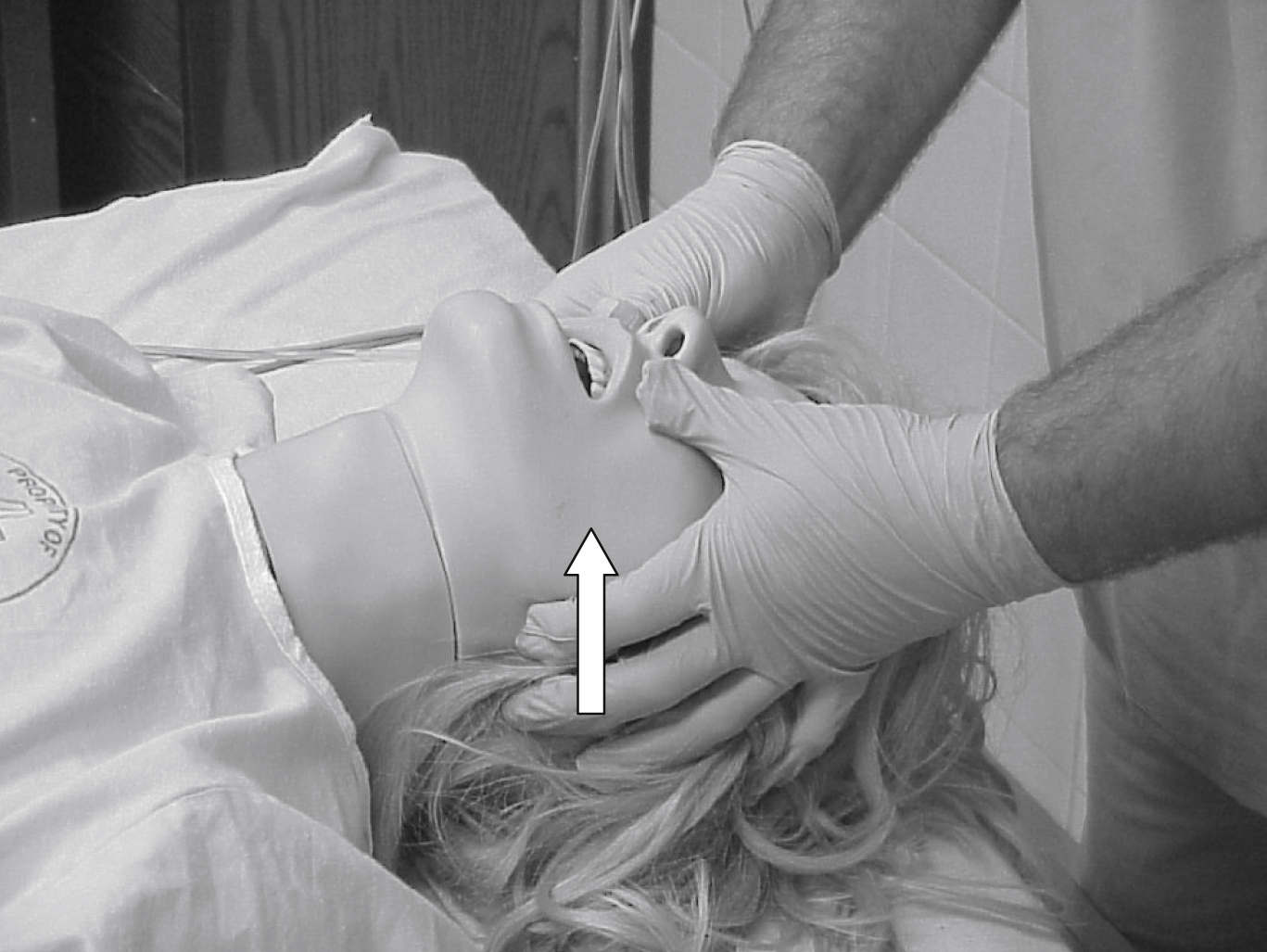
FIG. 29.4 Jaw thrust. Rescuer grasps angles of patient’s lower jaw and lifts with both hands. Jaw thrust can be done with head tilt (as pictured) or alone without head tilt. Jaw thrust without head tilt is technique of choice for patient with suspected neck injury because it causes least movement of cervical spine. (Courtesy of Department of Nurse Anesthesia, Virginia Commonwealth University, Richmond, VA.)
Subglottic Edema
The primary complication of postextubation laryngeal edema is subglottic edema. For the pediatric patient, this obstruction is typically observed in children 1 to 4 years of age. Traumatic intubation, tight fit of the endotracheal tube, coughing with the tube in place, position change with the tube inserted, surgery of the head or neck, and procedures that last more than 1 hour can result in subglottic edema. Crowing respirations, stridor, and rocking chest wall respiratory attempts may signal subglottic edema. Postoperative supplemental humidified oxygen can diminish airway swelling. Initial treatment includes humidified oxygen and nebulized mist treatment with racemic epinephrine. Further treatment may include inhalation of a helium–oxygen mixture, administration of dexamethasone, and calming with analgesics and parental or caregiver presence. Ambulatory surgery patients with subglottic edema treated with racemic epinephrine may be considered for overnight admission because of the risk of rebound edema. Extended observation for up to 8 hours may be sufficient if the parents are comfortable and emergency resources are readily available.
Bronchospasm
Sudden constriction of the smooth muscles in the walls of the bronchioles results in bronchospasm. Bronchospasm may be the result of preexisting asthma, allergy or anaphylaxis, chronic diseases of the lung (chronic bronchitis, emphysema), histamine release, mucous plugging, aspiration, pulmonary edema, wheezing with acute heart failure but without any other acute pulmonary pathology (cardiogenic asthma), or foreign body aspiration. Signs and symptoms include cough, expiratory wheezing, dyspnea, use of accessory muscles, and tachypnea. Treatment of the patient includes removal of the identified cause, oxygen administration, inhaled bronchodilators, and epinephrine. Depending on cause, an antihistamine or dexamethasone may be appropriate. Secretions should be suctioned. If the condition results from foreign body aspiration, such as a tooth, emergent bronchoscopy is needed. Ventilatory support may be necessary, and the patient may need reintubation for maintenance of oxygenation and ventilation.
Aspiration
Identified as a high-risk low-frequency occurrence, aspiration may be observed in the postanesthesia setting. The patient with a nasal or oropharyngeal airway in place and returning gag reflexes may become nauseated and vomit. In a nonresponsive state and supine position, the patient is at greater risk for aspiration. Types of aspirates include large particle, clear acidic or nonacidic fluid, foodstuff or small particle, and contaminated material. In addition, foreign bodies such as teeth or blood may be aspirated. Symptoms include unexplained tachypnea and tachycardia, cough, bronchospasm, hypoxemia, atelectasis, interstitial edema, hemorrhage, and acute respiratory distress syndrome. The aspiration can trigger laryngospasm, infection, and pulmonary edema.
Prevention of aspiration is preferred. Patients at risk should be identified before surgery and premedicated. Patients at risk are patients with emergent procedures, known full stomachs, or history of gastroesophageal reflux disease; those older than age 65 years; patients who are obese; and women in labor. Premedications include histamine blockers, nonparticulate antacids, and anticholinergic agents. During surgery, rapid sequence induction and nasogastric tube placement may help to minimize aspiration in the highest risk patients. However, preemptive use of a nasogastric tube may contribute to increased vomiting and subsequent aspiration; use should be limited to patients with known or suspected obstruction or ileus.3 After surgery, maintenance of the endotracheal tube until airway reflexes have returned and positioning of the patient with the head to the side or in a left lateral decubitus position can aid in decreasing the risk of aspiration. If aspiration occurs, hypoxemia should be corrected and hemodynamic stability maintained. The patient may need reintubation, suctioning, and mechanical ventilation. Arterial blood gases assist in planning respiratory management of the patient. A chest radiograph can be obtained, but findings may be inconclusive initially; radiographic findings may lag behind clinical signs by 24 hours after the suspected aspiration event. Prophylactic antibiotics or steroids are not recommended. Tracheal secretions should be cultured; if results are positive, antibiotics can be prescribed.
Hypoventilation
Hypoventilation may be the result of residual anesthetic agents; opioids; neuromuscular blocking agents; inadequate reversal of opioids, sedatives, or neuromuscular blocking agents; thoracic or abdominal incisions and procedures and subsequent splinting of incisions; or neuromuscular diseases.
Signs and symptoms include decreased respiratory rate, shallow respirations, increased end-tidal carbon dioxide (ETCO2), and increased PaCO2 (>45 mm Hg [hypercarbia]). Treatment includes identification and management of the cause of the hypoventilation, supplemental oxygen administration, verbal and tactile stimulation, deep breathing exercises, repositioning, and cautious use of opioid analgesics or sedatives. Oxygen saturation monitoring is necessary, and capnographic monitoring may be appropriate for patients at risk.
Hypoxemia
Unidentified hypoxemia in the postanesthesia patient is not as common since the advent of noninvasive oxygen saturation monitoring with pulse oximetry. Hypoxemia may be the result of a low inspired concentration of oxygen, hypoventilation, ventilation–perfusion inequality, increased intrapulmonary right to left shunt, or pneumothorax. It can also be caused by diffuse airway collapse, pulmonary edema, and pulmonary embolism. Treatment includes identification and correction of the cause, stimulation of the patient, supplemental oxygen administration, and continuous positive airway pressure (CPAP), which can be used in the spontaneously breathing patient. Patients who cannot maintain oxygen levels may need tracheal intubation and mechanical ventilation and positive end-expiratory pressure (PEEP) support.
Pneumothorax
Pneumothorax, an accumulation of air or gas in the pleural space, can occur during the perianesthesia period. It may be the result of percutaneous internal jugular and subclavian vein cannulation, hemodynamic monitoring line placement, certain upper extremity blocks (supraclavicular and infraclavicular approaches to the brachial plexus), or operative procedures of the chest. The patient may have sharp ipsilateral chest pain and dyspnea. Assessment findings include decreased breath sounds and hyperresonance on the affected side of the chest. Treatment includes supplemental oxygen administration and ordering of a chest radiograph. If a less than 20% pneumothorax is diagnosed based on the chest radiograph, the treating physician may opt to observe the patient for a period of time until the pneumothorax either resolves or increases. If the pneumothorax is greater than 20% or the patient has cardiovascular compromise, a chest tube may be needed.
Pulmonary Edema
Fluid overload, congestive heart failure, or acute pulmonary injury can result in pulmonary edema. Signs and symptoms include hypoxemia, crackles (rales), and decreased pulmonary compliance. Pulmonary infiltrates are seen on chest radiograph results.
Identification and treatment of the cause of the pulmonary edema is the first step in treatment. In addition, diuretics and fluid restriction to decrease afterload and supplemental oxygen administration may be ordered. Patients with an inability to maintain oxygenation or adequate ventilation may undergo intubation and mechanical ventilation and PEEP.
Noncardiogenic Pulmonary Edema
Noncardiogenic pulmonary edema, also known as negative pressure pulmonary edema, may be the result of upper airway obstruction, laryngospasm, bolus dosing with naloxone, incomplete reversal of neuromuscular blockade, or a significant period of hypoxia. When the cause is obstructive in origin, two types of postobstructive pulmonary edema (POPE) have been identified: type I and type II.4 Both present with acute respiratory distress. Type I usually occurs within 60 minutes of a precipitating event, but onset can be delayed up to 6 hours. Type I POPE may follow postextubation laryngospasm, epiglottitis, croup, choking or foreign body, strangulation, hanging, endotracheal tube obstruction, laryngeal tumor, goiter, mononucleosis, postoperative vocal cord paralysis, migration of the urinary catheter balloon used for tamponade epistaxis, near drowning, and intraoperative direct suctioning of an endotracheal tube adapter.3 Type II POPE develops soon after relief of chronic upper airway obstruction such as after tonsillectomy or adenoidectomy, removal of upper airway tumor, choanal stenosis, and hypertrophic redundant uvula.5
Signs and symptoms include hypoxemia, cough, failure to maintain oxygen saturation levels, tachypnea, and frothy sputum. Treatment includes supplemental oxygen administration and maintenance of a patent upper airway. CPAP may be used. Patients with an inability to maintain a patent airway may need intubation and mechanical ventilation with PEEP. For patients with significant compromise, hemodynamic support and continued observation in an intensive care unit may be needed. Patients with noncardiogenic pulmonary edema typically recover rapidly after the intense initial phase and leave the critical care unit within approximately 24 to 36 hours and without permanent sequelae from the event.
Pulmonary Embolism
Patients predisposed to development of pulmonary emboli include patients who are obese or immobile, are undergoing pelvic or long bone procedures, or have a history of congestive heart failure or malignant disease.6 Signs and symptoms can include tachypnea, pleuritic chest pain, hemoptysis, breathlessness, and a sense of impending doom. Treatment is supportive for correction of hypoxemia and hemodynamic instability. Intravenous heparin and morphine sulfate may be given to help stabilize the pulmonary capillary membrane. Prevention of venous thromboembolism and subsequent pulmonary emboli development includes pharmacologic prophylaxis (e.g., subcutaneous unfractionated heparin, low–molecular-weight heparins) or intermittent or sequential pneumatic compression devices.
Cardiovascular Complications
Cardiovascular complications that occur in the PACU range from relatively benign ectopic beats to hemodynamic collapse from an acute myocardial infarction. The perianesthesia nurse monitors the patient continuously in phase I, observing rate, rhythm, and blood pressure, and noting any signs or symptoms of hemodynamic compromise. The following section briefly discusses the more common cardiovascular complications seen in the perianesthesia setting.
Surgical and patient characteristics predict risk for a major adverse cardiac event (MACE) including death or myocardial infarction.7 Examples of low-risk procedures (risk of MACE <1%) include noncardiac procedures without significant fluid shifts and stress such as cataract extraction or simpler plastic surgery procedures. Typically, patients at low risk of perioperative MACE do not require further testing before procedures. Noncardiac procedures for which elevated risk for MACE is ≥1% include operations for peripheral vascular disease to emergent procedures and others where stress and fluid shifts may be significant. Patient risk factors are associated with coronary artery disease, recent myocardial infarction <60 days, cerebrovascular disease, heart failure, cardiomyopathies, valvular heart disease, arrhythmias and conduction disorders including patients with cardiovascular implantable electronic devices (CIEDs), pulmonary hypertension, and adult congenital heart disease. Additionally, the risk of cardiovascular complications is increased in patients with reduced functional status (i.e., limited exercise capacity or ability to perform activities of daily living and age ≥55 years).
Dysrhythmias
Dysrhythmias can occur as the result of hypoxia, hypercarbia, electrolyte abnormalities, acid-base alterations, myocardial ischemia, medication effects, pain, hypovolemia, bladder distention, and hypothermia. Occasional ectopic beats may be seen in healthy patients. Significant dysrhythmias necessitate immediate identification and treatment; these include premature ventricular contractions (more than five per minute, coupled [more than two together], or multifocal), ventricular tachycardia, ventricular fibrillation, asystole, heart block, pulseless electric activity, and new-onset atrial fibrillation. Treatment includes identification and treatment of the cause, supplemental oxygen administration, ventilatory and hemodynamic support, and pharmacologic therapy. Advanced cardiac life support (ACLS) or pediatric advanced life support (PALS) protocols are initiated when appropriate.
Bradycardia
Sinus bradycardia can occur as the result of vagal responses, hypoxia, medication effects, increased intracranial pressure (ICP), or distended bladder. Treatment is dependent on the cause and can include anticholinergic agents (e.g., atropine), supplemental oxygen administration, and stimulation. If the condition is the result of elevated ICP, hyperventilation and pharmacologic therapy may be indicated.
Tachycardia
Sinus tachycardia occurs commonly in the postanesthesia setting. Causes include hypoxia, hypercarbia, hypovolemia, sepsis, hyperthermia, heart failure, pain, medications, and psychological stress. Treatment includes administration of supplemental oxygen, ventilation support, and evaluation of fluid and cardiac status. If the condition results from pain, medication with analgesics is the treatment. Sedatives may be needed if the condition is from anxiety or stress. If the patient is hyperthermic, the patient’s core temperature is lowered with recommended cooling devices. Tachycardia in patients with coronary artery disease can increase the risk of myocardial ischemia.
Hypotension
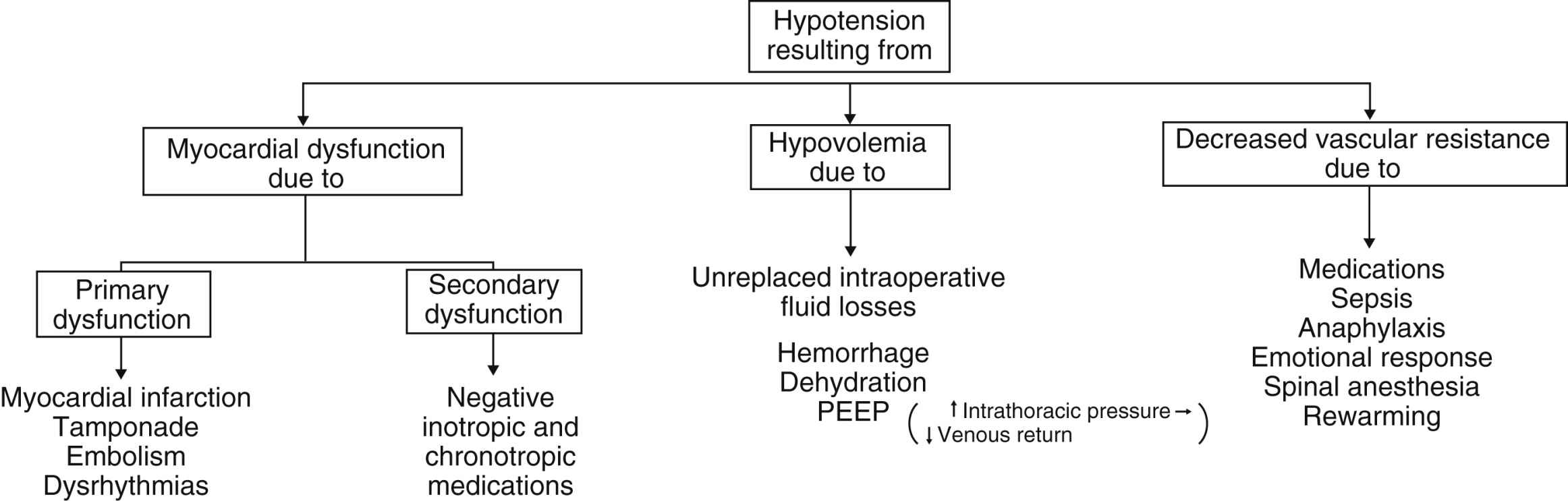
Hypotension is defined as blood pressure less than 20% to 30% of the baseline blood pressure.8 Causes range from use of an inappropriately sized cuff, to hypovolemia, myocardial dysfunction, and a decrease in systemic vascular resistance (Fig. 29.5). Management and treatment of hypotension in the PACU include use of a cuff of the appropriate size, administration of supplemental oxygen, initiation of fluid resuscitation, stoppage of medication infusions if causative, and passive leg raising for an evaluation of fluid responsiveness.9 Inotropic agents or vasopressor or vasoconstrictive agents may be ordered.
Hypertension
Hypertension is defined as “persistent elevation of systolic blood pressure greater than 140 mm Hg, a diastolic blood pressure greater than 90 mm Hg, or requiring an antihypertensive treatment.”10 Too small or narrow of a cuff can result in abnormally elevated blood pressures. Pain, stress, hypoventilation, hypoxemia, hypercarbia, fluid overload, delirium, medications, bladder, bowel or stomach distention, or hypothermia can cause hypertension. Many of the patients in PACU in whom hypertension develops have preexisting hypertension. The elevation in blood pressure is usually benign and short lived; however, the hypertension can precipitate myocardial ischemia in the patient with coronary artery disease as a result of stimulation of the sympathetic nervous system. Treatment for hypertension includes use of an appropriately sized cuff and identification and management of the underlying cause first. This condition may necessitate ventilatory support and oxygen administration, analgesics or sedatives, bladder decompression, and antihypertensive medications.
Patients who have had a cervical or thoracic spinal cord injury (above T6) are at risk for developing autonomic dysreflexia, which is a massive uninhibited sympathetic cardiovascular response to noxious stimuli (e.g., bowel or bladder overdistention) characterized by paroxysmal hypertension, severe headache, flushing above the level of injury, diaphoresis, temporal or neck vessel engorgement, nasal congestion, blurred vision, piloerection, bradycardia, cardiac arrhythmias, and atrial fibrillation.11 Treatment includes elimination of the precipitating stimuli if known and elevation of the head of the bed. Pharmacologic treatment may be needed to reduce the blood pressure if the blood pressure remains elevated after these measures. Medications for the treatment of hypertension include nifedipine and captopril.
Acute Myocardial Infarction
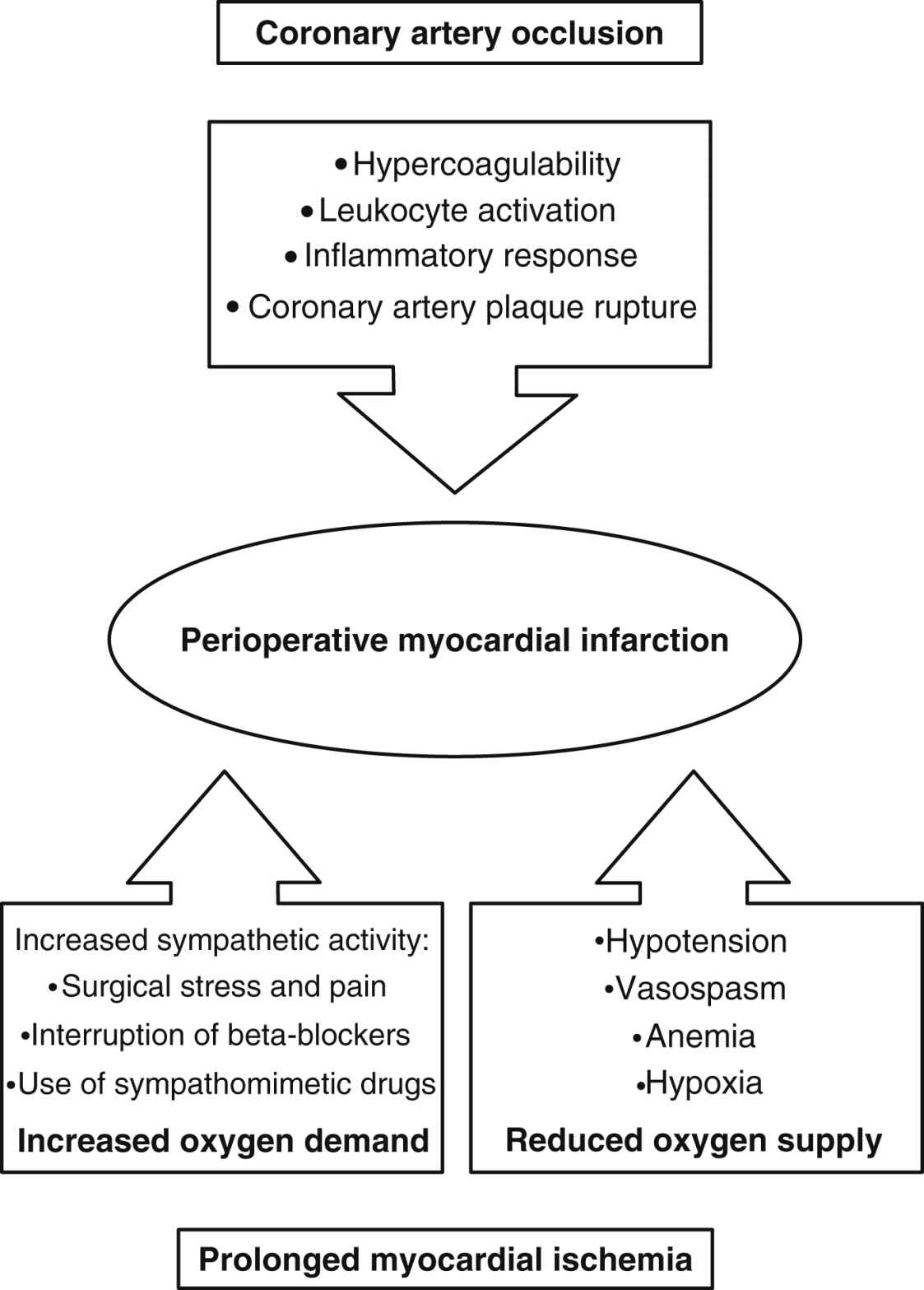
The patient with a history of preexisting coronary artery disease, diabetes, and significant dysrhythmias is at risk for perioperative cardiac events.7 The pathology of perioperative myocardial infarction is shown in Fig. 29.6.12
When a patient has chest pain in the PACU, the cause needs to be evaluated with the first consideration for the source as cardiac in origin (Box 29.2).13 The signs and symptoms of myocardial infarction include chest pain, tachypnea, tachycardia or other dysrhythmias, hypotension or hypertension, pallor, diaphoresis, cool extremities, nausea, vomiting, and generalized weakness. New Q waves or increasing prominence of existing ones, ST-segment elevations, and T-wave inversions may be seen on electrocardiogram (ECG) results. Initial treatment is aimed at relieving chest pain, reducing cardiac workload, stabilizing cardiac rhythm, limiting infarct size, preventing further damage, and detecting and treating complications. The first response is to order a 12-lead ECG; initiate supplemental oxygen to maintain arterial oxygen saturation (SaO2) above 90%13; administer morphine, nitrates, and antiplatelet/anticoagulant agents; and continuously monitor the ECG. Laboratory blood studies are obtained, including cardiac troponin-I or T levels, and, for additional prognostic information, B-type natriuretic peptide or N-terminal pro-B-type natriuretic peptide levels. The patient is evaluated and transferred to a critical care unit as indicated by diagnosis for continued monitoring and possible interventional procedures and management.
Thermoregulation
For a detailed discussion of thermoregulation including malignant hyperthermia (MH), see Chapter 53.
Hypothermia
Hypothermia is defined as a core temperature of less than 36° C.11,14 Signs and symptoms of hypothermia include shivering, restlessness, discomfort, and cold pale cyanotic extremities and distal appendages from peripheral vasoconstriction. This state can lead to delayed medication clearance, myocardial ischemia, unexplained hypertension, and residual paralysis from neuromuscular blocking agents. The American Society of PeriAnesthesia Nurses Evidence-Based Clinical Practice Guideline for the Promotion of Perioperative Normothermia offers the perianesthesia nurse guidance for assessment and management of the patient who is hypothermic during the perianesthesia period.14 Recommendations for treatment of the patient include active rewarming, supplemental oxygen administration, and ventilatory support if necessary.
Hyperthermia
Hyperthermia is defined as a core temperature of more than 38° C.11,14 Temperature elevations may be the result of blood transfusion reactions, warm environment, medication-induced fever, use of anticholinergic medications, overcorrected hypothermia, endocrine disorder, hypothalamic injury, or MH. Signs and symptoms include fever, tachycardia, and warm flushed skin and other signs and symptoms depending on the cause of the hyperthermia (shaking, chills or rigors, agitation). The cause should be identified and corrected when possible. Cooling blankets or pads may be used, and an antipyretic agent may be given.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree