Positive End-Expiratory and Continuous Positive Airway Pressure
KEY POINTS
1 Adding positive end-expiratory pressure (PEEP) can help maintain patency of collapsed lung units or further distend those that are already patent. The former action usually is beneficial, whereas the latter may cause alveolar overdistention. Both effects may occur simultaneously in different lung regions at the same level of PEEP.
2 Positive end-expiratory alveolar pressure or total PEEP is the sum of the PEEP applied intentionally at the airway opening (PEEP or “extrinsic” PEEP) and auto-PEEP (“intrinsic” or “inadvertent” PEEP) that results from dynamic hyperinflation. Expiratory muscle activity may raise the measured value for total PEEP.
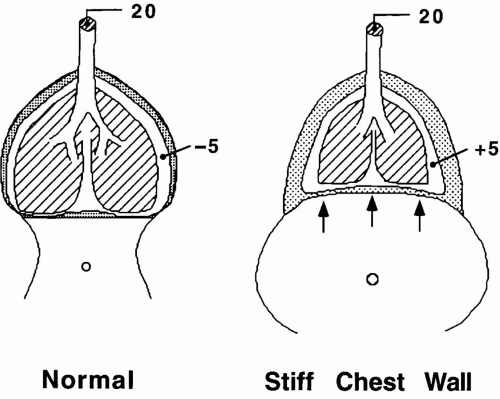
3 Transalveolar pressure is the key variable that determines PEEP’s effect on lung volume. A patient with a poorly compliant chest wall will require a higher PEEP to achieve adequate lung expansion.
4 Use of PEEP in improving arterial oxygenation, in minimizing ventilator induced lung injury, and perhaps in preventing pneumonia stems primarily from its ability to impede the recollapse of edematous or compressed alveoli recruited by higher pressures experienced during the tidal inspiratory phase or by a sigh or recruitment maneuver. PEEP also improves the distribution of alveolar liquid, translocating edema fluid from the alveolus to the interstitium. When PEEP reduces cardiac output, it also tends to reduce shunt fraction.
5 The volume recruiting effect of PEEP is influenced by the chest wall compliance, the tidal volume, and the activity of the respiratory muscles. Any benefit from PEEP on oxygen exchange may be offset by expiratory muscle activity and restored by muscle relaxation.
6 A shift to the prone position exerts a selective PEEP-like action in the dorsal regions of the lung and commonly improves oxygenation of patients with lung edema. Proning also has the potential to initiate transfer of secretions, inflammatory edema, and other biofluids to the central airway and to the previously unaffected lung sectors.
7 PEEP tends to decrease both preload and afterload to the left ventricle. Impaired venous return may lower the cardiac output in a passive patient who does not have intact vascular reflexes or adequate circulating blood volume. Conversely, reduced left ventricular afterload resulting from PEEP may benefit the patient in acute congestive heart failure. The hemodynamic effects of auto-PEEP are similar to those of external PEEP.
8 Increased peak and mean alveolar pressures that result from excessive PEEP may produce or extend barotrauma, reduce oxygen delivery, and increase ventilatory dead space. PEEP may either increase or decrease the work of breathing.
9 Good candidates for PEEP have clinically significant hypoxemia that is refractory to inspired oxygen, diffuse acute pulmonary disease, a poorly compliant respiratory system, a tendency for atelectasis, acute cardiogenic edema with increased left ventricular afterload, audible dependent rales during tidal breathing, or severe airflow obstruction with tidal flow limitation. Virtually all intubated patients are candidates for PEEP of 3 to 5 cm H2O to help offset the lung compressing effects of recumbency.
10 Choosing the optimum level of PEEP is an empirical process determined by the response of multiple gas exchange, mechanics, and hemodynamic variables to a well-monitored PEEP trial. Recruitment maneuvers are integral to the selection process.
11 Auto-PEEP can dramatically increase the work of breathing and provoke patientventilator dyssynchrony. In many patients with flow limitation during tidal breathing, these problems can be addressed by adding an appropriate level of PEEP that minimizes end-expiratory airflow without raising the peak alveolar pressure significantly.
Hypoxemia resulting from alveolar collapse or edema often responds to alveolar recruitment and maintenance of lung unit patency with positive end-expiratory airway pressure (PEEP). Adding PEEP helps keep lung units patent but may further distend those that are already open. When PEEP maintains recruited lung volume, it not only improves arterial oxygenation but also may reduce the elastic work of expanding the lung or improve the distribution of ventilation. Conversely, PEEP added to an already “open” lung without compensatory recruitment tends to create dead space and possibly worsen the oxygen exchange. Maintaining end-expiratory lung volume helps prevent ventilatorinduced lung injury (VILI) during the initial stages of the acute respiratory distress syndrome (ARDS), reduces alveolar edema, and seems useful in avoiding complications after thoracic and upper abdominal surgery.
This chapter focuses primarily on the use of PEEP in hypoxemic respiratory failure; this objective is quite distinct from that of adding PEEP to reduce the work of breathing and improve breath triggering (without increasing the lung volume) during flow-limiting airflow obstruction. The latter important topic is addressed elsewhere (see Chapter 25).
DEFINITIONS
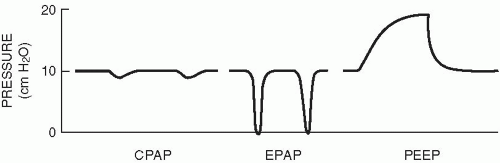
Positive end-expiratory alveolar pressure, or “total PEEP” (PEEPT), is the sum of PEEP applied intentionally at the airway opening (PEEP or “extrinsic” PEEP) and auto (“occult,” “inadvertent,” or “intrinsic”) PEEP (PEEPi). The expressions “assisted ventilation with PEEP” and “continuous positive pressure breathing” are synonymous, referring to mechanically delivered tidal breaths with positive pressure maintained at end-expiration (Fig. 9-1). By convention, when airway pressure is positive at the end of expiration during time limited mechanical ventilation, the acronym is “PEEP.” During spontaneous breathing cycles, it is called “continuous positive airway pressure,” or “CPAP.” In practice, CPAP has come to imply that the patient provides some or all of ventilating power while PEEP suggests that the ventilator is carrying most or all of the breathing workload. The terms are often interchanged, however, as they will be in this chapter—the key principles underlying PEEP and CPAP are identical. When two levels of PEEP are alternated, with spontaneous breaths occurring during each phase, the mode is termed “biphasic positive airway pressure” or “BIPAP.” (In this context, the term BIPAP must not be confused with “bi-level,” commercially known as BiPAP, which has been applied to a combination of pressure support and CPAP intended for noninvasive ventilation applied via face mask [see Chapter 7].) If the lower level of BIPAP is maintained only transiently (e.g., the span of a single exhalation), the mode is referred to as “airway pressure release.” Several of these PEEP variants are discussed elsewhere in this volume (see Chapters 7 and 10). The discussion here will focus on single levels of end-expiratory alveolar pressure.
PATHOPHYSIOLOGY
Actions of PEEP in Acute Hypoxemic Respiratory Failure
The normal lung requires no PEEP to maintain full recruitment—periodic sighs are sufficient to prevent or reverse the widespread alveolar collapse. When the chest cavity is reduced in size (e.g., after abdominal surgery), the lung is edematous or infiltrated (e.g., pulmonary edema), the alveoli are inherently unstable (surfactant depletion ARDS), and small airways are predisposed to closure during the tidal cycle, particularly in gravitationally dependent regions. Collapsed units open over a spectrum of airway pressures, determined largely by the local pressures that surround them. Even in ARDS, most collapsed units recruit at pressures lower than 25 cm H2O. Once opened, a lower airspace pressure (PEEP or CPAP) must be sustained to prevent their reclosure. The utility of PEEP in improving arterial oxygenation, in minimizing VILI, and perhaps in preventing pneumonia stems primarily from its ability to impede the recollapse of edematous or compressed alveoli recruited by higher pressures (Table 9-1).
PEEP applied to lung units that are already open increases alveolar dimensions, resting lung volume, and pleural pressure. Distention tends to redirect the blood flow, increase the vena caval resistance to venous return, and create ventilatory dead space, as well as to redistribute alveolar liquid to the interstitial space and favor edema clearance. In a heterogeneous lung with a wide range of unstable alveoli, alveolar opening may occur in different regions throughout inspiration, particularly when PEEP is low and tidal volume (VT) is high. When PEEP is added to an unchanging tidal volume, collapsed lung units are opened by the relatively high alveolar pressures (amplified by interdependence) that occur at the end of the inspiratory cycle; PEEP prevents their reclosure during expiration. Oxygenation may benefit by at least two other mechanisms. When PEEP reduces cardiac output, blood flow through shunt regions may also decline, reducing venous admixture. Perhaps more importantly, PEEP improves the distribution of alveolar liquid and translocates fluid from alveolar to interstitial spaces, lowering the diffusion distance for oxygen exchange. In the presence of alveolar edema, PEEP may prevent airway flooding by expanding the alveolar reservoir and encouraging fluid migration into the interstitial space. By inhibiting distribution of proteinaceous and mediator-laden biofluids via the airway network, both actions may play an important role in the prevention of injury propagation, as described in Chapter 8. (Conversely, abrupt removal of PEEP may precipitate translocation of alveolar liquid into the airways, impeding airflow and occasionally generating froth.) Most available data indicate that PEEP redistributes but does not decrease the total lung water; in some instances, lung weight may actually increase because of distention of the interstitial space and raised pulmonary venous and lymphatic pressures.
TABLE 9-1 BENEFITS AND PROBLEMS OF POSITIVE END-EXPIRATORY AIRWAY PRESSURE | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
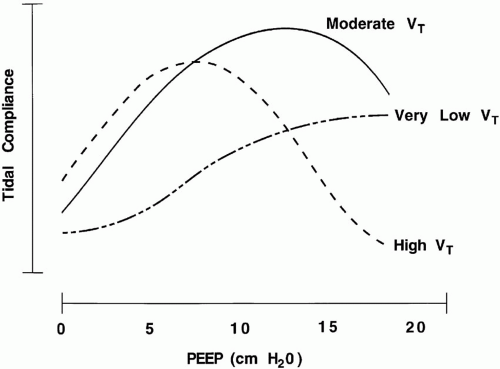
Interaction of PEEP and Tidal Volume
Recruitment of lung volume is a joint function of PEEP and the opening pressures generated in response to tidal volume. Airways open at higher volumes and trans-structural pressures than those at which they close (see “Recruiting Maneuvers”). Therefore, to achieve the same effect on oxygenation and compliance, higher values of PEEP may be needed when tidal volumes are smaller (Fig. 9-2) (see Chapter 25). Moreover, even if calculated tidal (chord) compliance values are identical, failure to maintain sufficient PEEP may result in tidal opening and closure of dependent lung units, a process that may produce high shearing stresses believed to damage the delicate lung tissues. Some experimental evidence suggests that the variation in tidal volume normally observed during health (biologically variable ventilation) serves an important recruiting function. The same minute ventilation achieved after lung injury with monotonous tidal volumes is associated with less-effective
oxygenation than the identical ventilation accomplished with varying tidal volumes. Any benefit is believed to be due (at least in part) to the avalanches of recruitment that occur when the higher inspiratory pressures are transiently applied.
oxygenation than the identical ventilation accomplished with varying tidal volumes. Any benefit is believed to be due (at least in part) to the avalanches of recruitment that occur when the higher inspiratory pressures are transiently applied.
Importance of Chest Wall Compliance
Volume changes resulting from PEEP are shared equally by the lungs and chest wall. Assuming that exhalation occurs passively, the volume recruited by PEEP (ΔV) depends on the compliance of the entire respiratory system, which itself is a function of both lung (CL) and chest wall (CW) compliances:
ΔV = PEEPT × CRS = PEEPT × [(CLCW)/(CL + CW)]
As discussed elsewhere (Chapter 5), the pressure distending the lung at end-expiration is (PEEPT – PPL), whereas the pressure that distends the passive chest wall is PPL alone. It follows that the volume-expanding and hemodynamic effects of PEEP will vary with the compliance of the chest wall (Fig. 9-3). A very obese patient or one with a recently operated abdomen or rib cage requires relatively more PEEP to keep the lung adequately recruited, and PPL tends to rise disproportionately with each PEEP increment. Local variations in the compliance of the chest wall help explain the heterogeneity of infiltration and lung expansion in the settings of pulmonary edema acute lung injury.
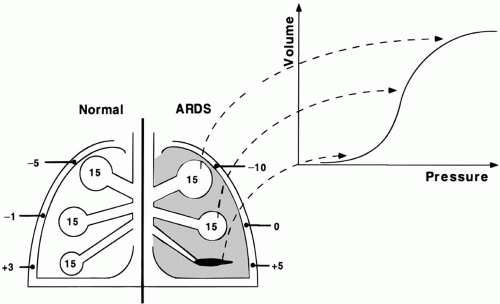
Regional Effects of PEEP
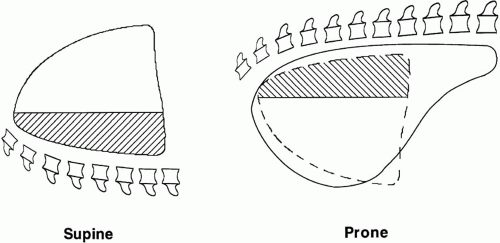
Pressure varies from site to site within the pleural space. In the supine position, a ventral-to-dorsal gravitational gradient causes the pleural pressure that surrounds dependent alveoli to be several centimeters H2O greater than that in nondependent regions, and this difference increases in the setting of acute lung injury. (This gravitational gradient of pleural pressure is less steep in the prone position.) Because alveolar distention is a function of transalveolar pressure (airspace minus surrounding pressure), regional alveolar dimensions and propensities to collapse differ, despite a common
airway pressure. As progressively higher pressures are applied, individual lung units pop open at some critical opening pressure but collapse abruptly as it is withdrawn. PEEP that is sufficient to hold alveoli in the uppermost regions patent throughout the tidal cycle may be insufficient to prevent the collapse of gravitationally dependent ones (Fig. 9-4). The consequences of this gradient of pleural and transalveolar pressures is likely to explain the marked dependency of computed tomographic (CT) densities evident during the initial stages of acute lung injury, as well as the lower “inflection zone” of improving compliance often observed on the inspiratory pressure-volume curve of the respiratory system early in the course of ARDS. PEEP tends to narrow the pleural pressure gradient if recruitment occurs or if alveoli in all regions are open. A PEEP value which recruits the most dependent alveoli may be needed to avoid their repeated opening and recollapse during each tidal cycle.
airway pressure. As progressively higher pressures are applied, individual lung units pop open at some critical opening pressure but collapse abruptly as it is withdrawn. PEEP that is sufficient to hold alveoli in the uppermost regions patent throughout the tidal cycle may be insufficient to prevent the collapse of gravitationally dependent ones (Fig. 9-4). The consequences of this gradient of pleural and transalveolar pressures is likely to explain the marked dependency of computed tomographic (CT) densities evident during the initial stages of acute lung injury, as well as the lower “inflection zone” of improving compliance often observed on the inspiratory pressure-volume curve of the respiratory system early in the course of ARDS. PEEP tends to narrow the pleural pressure gradient if recruitment occurs or if alveoli in all regions are open. A PEEP value which recruits the most dependent alveoli may be needed to avoid their repeated opening and recollapse during each tidal cycle.
Regional PEEP and the Prone Position
In experimental animals, the gradient of alveolar dimensions and pleural pressure is considerably greater in the supine position than in the prone position. Consequently, the prone position alters the distribution of lung volume corresponding to a
given airway pressure, with dorsal regions better expanded (Fig. 9-5). In effect, altering position exerts a differential PEEP-like effect in different lung regions. For the same PEEP, the distribution of tidal ventilation is more homogeneous, and ventilation -perfusion matching and arterial oxygenation tend to improve. Available data suggest that a similar phenomenon also occurs in humans. The effect of prone positioning on overall functional residual capacity (FRC) is debated and is likely to be influenced by any positional changes that occur in chest wall compliance because of the supporting surface. Although the distribution of volume is altered dramatically, FRC increases only modestly or remains unchanged by the turning process.
given airway pressure, with dorsal regions better expanded (Fig. 9-5). In effect, altering position exerts a differential PEEP-like effect in different lung regions. For the same PEEP, the distribution of tidal ventilation is more homogeneous, and ventilation -perfusion matching and arterial oxygenation tend to improve. Available data suggest that a similar phenomenon also occurs in humans. The effect of prone positioning on overall functional residual capacity (FRC) is debated and is likely to be influenced by any positional changes that occur in chest wall compliance because of the supporting surface. Although the distribution of volume is altered dramatically, FRC increases only modestly or remains unchanged by the turning process.
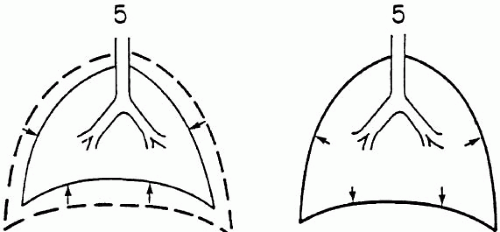
Active Expiration
If exhalation occurs passively (as it does during quiet, unstressed breathing), PEEP achieves its desired effect—increases in end-expiratory lung volume and in the number of open air channels. However, if the resulting lung expansion proves uncomfortable, spontaneously breathing patients may actively oppose PEEP in attempting to limit the volume increase. Active expiration to a volume lower than the equilibrium position that corresponds to the PEEP applied to the passive patient stores potential energy. In this way, PEEP or CPAP may provide a mechanism by which the dyspneic patient can use the expiratory muscles to share the workload otherwise borne entirely by inspiratory muscles. As the expiratory muscles relax, the outward recoil of the chest wall then provides an inspiratory boost (Fig. 9-6). The expiratory muscles are activated normally during vigorous exercise, hyperpnea, and impeded expiration. Opposition to PEEP occurring in a hypoxemic patient may attenuate volume recruitment, especially in the peridiaphragmatic zones. By silencing the expiratory muscles, sedation or paralysis restores the volume recruitment effect of PEEP and can markedly improve oxygenation. In addition, reduced oxygen consumption because of less respiratory effort and agitation undoubtedly contributes as the ventilator assumes the task of powering ventilation.
Time Course of PEEP Effect on Gas Exchange
Although lung recruitment is nearly completed within five to ten breaths, the time course is quite variable; several hours may be required to realize the full effect of a given PEEP increment. On the other hand, desaturation usually occurs quite abruptly upon PEEP withdrawal. Because PEEP’s primary benefit relates to the maintenance of lung volume and not to the positive pressure itself, the lung can be expanded by internally positive or externally negative pressure. Therefore, it should cause no concern for lost volume when a patient transiently pulls an inspiratory airway pressure lower than the set PEEP level. To generate a lower airway pressure, pleural pressure must have decreased at least as much as alveolar pressure, so that transpulmonary pressure and end-expiratory lung volume are preserved. (On the other hand, such a decline in pleural pressure may obligate significant ventilatory work.)
PEEP and Mean Airway Pressure
Mean alveolar pressure and its most easily measured analog, mean airway pressure, are discussed at length elsewhere in this text (see Chapters 5 and 24). It is worth noting here, however, that although mean alveolar pressure can be raised in a variety of ways, PEEP has the most predictable effect on oxygenation, combating end-expiratory lung unit collapse as it raises both mean airway and mean alveolar pressures by the amount of the PEEP applied. Just as PEEPT determines the end-expiratory alveolar dimension, in a passive patient, the mean airway pressure determines the average or mean alveolar volume. Most cardiovascular effects of PEEP are mediated by mean alveolar pressure via its effects on mean intrapleural and right atrial pressures. Apart from its effect on mean airway pressure, PEEPT maintains collapsible alveoli recruited throughout the tidal breath; therefore, it is instrumental in improving oxygen exchange and avoiding VILI. (In fact, it
has been argued that raising mean airway pressure while holding PEEPT constant may not help markedly to improve the arterial oxygen delivery.)
has been argued that raising mean airway pressure while holding PEEPT constant may not help markedly to improve the arterial oxygen delivery.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree