Chapter 28 Poisoning, overdosage, drugs and alcohol
POISONING AND OVERDOSAGE
Assessment
History
Investigations
Depending on the clinical setting other investigations would include:
Principles of management
Resuscitation, stabilisation and supportive care
All patients with an overdose should have intravenous access.
Decontamination
Gastrointestinal (GI) decontamination
The efficacy of activated charcoal is time-dependent and therefore should be considered mainly in those presenting within 1 hour when the poisoning is assessed to be high-risk. The main complication of charcoal is pulmonary aspiration, especially in the obtunded patient. Toxins not well adsorbed by charcoal are listed in Table 28.1. Activated charcoal is also available with a cathartic (e.g. sorbitol). There is little evidence to suggest that the addition of a cathartic is superior to using activated charcoal alone.
Table 28.1 Drugs not well adsorbed by activated charcoal
| Drug group | Examples |
|---|---|
| Alcohols | Ethanol, methanol, isopropyl glycol, ethylene glycol |
| Metals | Lithium, iron, mercury, potassium, lead, arsenic |
| Acids and alkalis | |
| Hydrocarbons | Turpentine, kerosene, eucalyptus oil, benzene |
Elimination
Multiple doses of charcoal may decrease drug absorption in some cases (Box 28.2). A suggested dosing regimen would be 25 g (adults) or 0.5 g/kg (children) every 2–4 hours. It is contraindicated if there is a bowel obstruction or decreased level of consciousness in a patient without a protected airway. Always check for the presence of bowel sounds before administering the next dose.
Box 28.2 Situations when multiple doses of charcoal may reduce drug absorption
Urinary alkalinisation may be used for increasing elimination of weak acids. This can be achieved by intravenous administration of sodium bicarbonate. Give a bolus of 1 mmol/kg IV followed by an infusion (100 mmol of sodium bicarbonate in 1000 mL 5% dextrose in 0.9% saline over 4 hours). Adjust the rate to a urinary pH > 7.5. Complications of bicarbonate therapy include fluid overload, alkalaemia, hypokalaemia and hypocalcaemia. Main indication is salicylate overdose.
Dialysis is the most commonly used form of extracorporeal elimination. It can enhance elimination of various toxins (Box 28.3). Indications for dialysis are listed in Box 28.4.
Specific therapies
Cardiovascular instability
Hyperthermia
TOXIDROMES AND SPECIFIC OVERDOSES
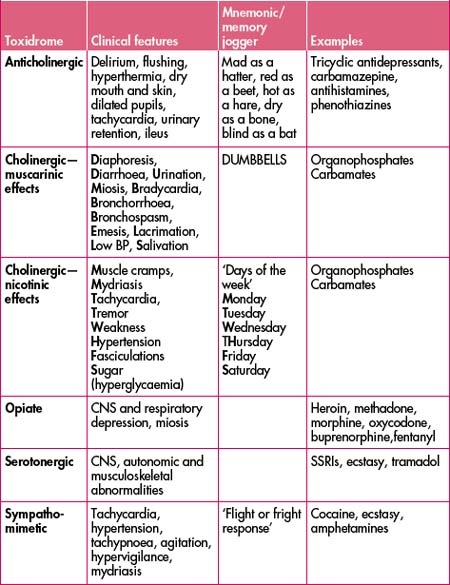
The clinical presentation of some poisonings may be predictable based on the pharmacology of the drug/substance involved. Some classic toxidromes with examples are listed in Table 28.2.
Opioids
This group of drugs includes those derived from opium as well as those that have opiate-like activity. Typical toxic effects are CNS and respiratory depression and miosis. Acute lung injury has been reported, typically occurring once ventilation has been restored following a period of respiratory depression. Other effects include mild hypotension (arteriolar and venous vasodilation). Treatment of opioid toxicity is supportive, especially of the airway and ventilation, and sometimes involves the use of naloxone, either as bolus dose(s) or infusion. Several drugs in this group have atypical toxic effects (Table 28.3).
| Opioid | Atypical toxic effects of clinical significance |
|---|---|
| Tramadol | Serotonergic syndrome, seizures |
| Dextropropoxyphene | Seizures, wide QRS arrhythmias, negative inotropic effects (Na channel blockade) |
| Methadone | Prolonged QT interval (possibly → torsades de pointes) |
| Pethidine | Seizures |
| Fentanyl | Muscle rigidity (rapid injection) |
Key points—opioids
Paracetamol
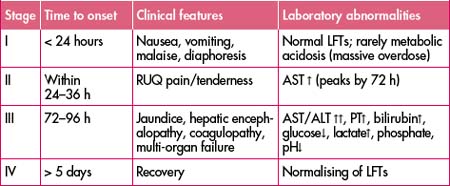
Paracetamol overdoses can be either single or staggered ingestions. There are four described stages of paracetamol poisoning (Table 28.4). Stage II marks the onset of liver injury. Renal failure is seen in 25–50% of those with hepatic dysfunction. Death is usually due to multi-organ failure, sepsis, haemorrhage, acute respiratory distress syndrome and/or cerebral oedema. Key blood tests are paracetamol level and transaminases—aspartate aminotransferase (AST) and alanine aminotransferase (ALT). Prothrombin time (PT) may also be indicated. Paracetamol levels are reported in various units (mg/L or μmol/L). When plotting the paracetamol level on the nomogram, always check the units are corresponding to the correct axis. Failure to do so may be life-threatening.
Paracetamol can be implicated in an accidental overdose. Remember to ask quantities of paracetamol ingested in the patient who has been self-medicating to achieve analgesia. Paracetamol is a common component of over-the-counter medications such as cold and flu preparations and migraine tablets. Serious hepatotoxicity is less common in children compared to adults. Charcoal can be given in those who present within 1 hour after potentially toxic ingestions.
Key points—paracetamol
Guidelines and treatment nomogram
General key points
Management of acute single ingestions
Presentation 8 hours after ingestion:
Management of staggered ingestions
Repeated supratherapeutic ingestion
Table 28.5 Repeated supratherapeutic doses that may be associated with hepatic injury
| Adults and children aged > 6 years | Children aged < 6 years |
|---|---|
| > 200 mg/kg or 10 g (whichever is less) over a single 24-hour period | ≥ 200 mg/kg over a single 24-hour period |
| 150 mg/kg or 6 g (whichever is less) per 24-hour period for the preceding 48 hours | ≥ 150 mg/kg per 24-hour period for the preceding 48 hours |
| > 100 mg/kg or 4 g/day (whichever is less) in patients with predisposing risk factors (e.g. chronic alcohol use, use of enzyme-inducing drugs, prolonged fasting, dehydration) | ≥ 100 mg/kg per 24-hour period for the preceding 72 hours |