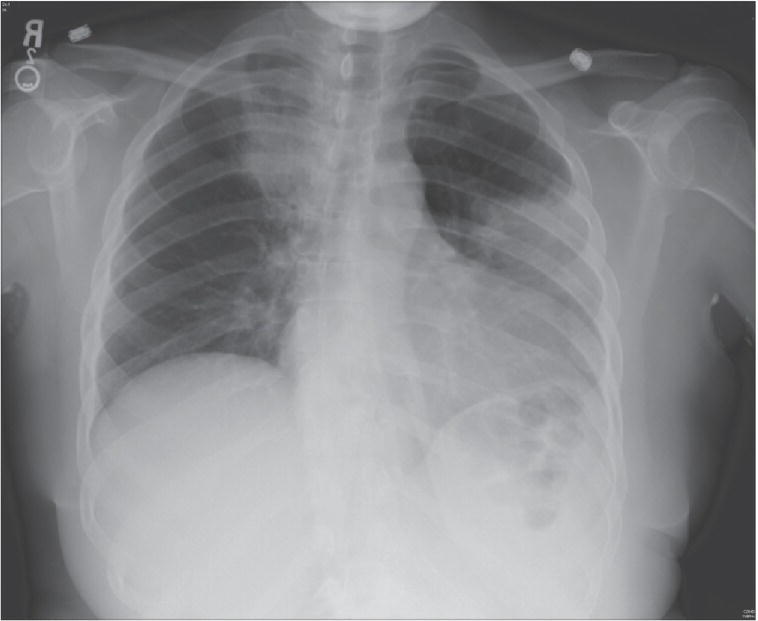
John Bedolla1 and Jesse M. Pines2,3 1 Department of Surgery and Perioperative Care, Dell Medical School, University of Texas, Austin, TX, USA 2 US Acute Care Solutions, Canton, OH, USA 3 Department of Emergency Medicine, Drexel University, Philadelphia, PA, USA Community‐acquired pneumonia (CAP) is an acute infection of the lung’s parenchyma accompanied by symptoms of acute illness (Figure 29.1). There are several challenges in the ED evaluation of patients with CAP. The chest radiograph has a false‐negative rate of 7–10%. Therefore, by itself, a negative chest X‐ray does not entirely rule out pneumonia. The history and physical exam, as well as serum testing, inform a structured and unstructured estimation of pretest probability for CAP. Illness severity in diagnosed CAP often guides decisions about admission, further diagnostic testing in the ED, and the choice of antibiotics. There are diagnostic scoring systems for estimating the pretest probability of CAP, and scoring systems for estimating the severity of illness, expressed as mortality.1,2 The prevalence of CAP in unselected patients presenting with cough and fever is 5–10%. Beginning with this prevalence, a pretest probability for CAP can be estimated using a structured or unstructured approach. An unstructured approach means the clinician simply adds of positives and negatives to arrive at a general sense or high or low probability of pneumonia. A more structured approach, as advocated by Diehr and Heckerling, involves using the 6–7 of the most salient clinical and laboratory elements to establish a more continuous range of pretest probabilities, ranging from less than 1% to greater than 50%. The pretest probability along with the chest radiograph interpretation and the negative predictive value (NPV) or positive predictive value to arrive at posttest probability for CAP. When considering CAP in the setting of a viral respiratory pandemic, it is essential to know that some viral disease, such as severe acute respiratory syndrome (SARS), middle east respiratory syndrome (MERS), coronavirus 2019 (COVID‐19), and Hantavirus, can present dense lobular findings typical of bacterial pneumonia, and multifocal infiltrates usually associated with pneumonia.3–5 Figure 29.1 Left lower lobe pneumonia. One of the most widely used severity scoring systems is the pneumonia severity index (PSI) which was developed by Fine et al.6 Table 29.1 details the elements of the PSI and its association with risk of death at 30 days. The PSI helps guide disposition by identifying patients who are at low risk for death and therefore candidates for outpatient management. The PSI score places patients with pneumonia into tiers I, II, III, IV, and V, with a mortality of 0.1%, 0.6%, 0.9%, 9.5%, and 26.7%, respectively. Tiers I, II, and III have mortality rates sufficiently low for these patients to be treated as outpatients. The PSI has a sensitivity of 99.7% for mortality, but a low specificity at 23%, for a NPV of 99.7 and a PPV of 6. The PSI weighs patient co‐morbidities and age more heavily than other scoring systems. The PSI is also relatively cumbersome and requires an arterial blood gas.7 Table 29.1 The pneumonia severity index Source: Data from [6]. Table 29.2 The CURB‐65 scoring system* * Each element, when positive, is assigned one point. The CURB‐65 was developed by the British Thoracic Society. The purpose of the CURB‐65 is to identify patients who are at high risk of mortality from pneumonia. The elements of the CURB‐65 are detailed in Table 29.2. In the CURB‐65, similar to the PSI, higher numbers of points correlated with higher 30‐day mortality rates. In an international derivation and validation study, the 30‐day mortality rates for the CURB‐65 were 0.7% for score 0, 3.2% for score 1, 3% for score 2, 17% for score 3, 41.5% for score 4, and 57% for score 5. The authors of the CURB‐65 criteria have suggested that patients who score 0 or 1 are at low risk for mortality and can be managed as outpatients, while those who have a score of 2 are at intermediate risk, and those with scores >2 have severe CAP and are at high risk and should be managed in an intensive care unit. CURB‐65 has a sensitivity of 96% for mortality and a specificity of 34%, for a NPV of 99.4% and a PPV of 7%. CURB‐65 has slightly lower sensitivity and specificity compared with PSI. On the other hand, it is relatively easier and more reliably performed, as it takes into account only 5 elements: mental status, blood urea nitrogen (BUN), respiratory rate, blood pressure, and age cut off of 65. It relatively underestimates the severity of asthma in young patients.8,9 Other scores that have been used to predict mortality are: CURB (CURB‐65 minus age), CRB (CURB minus BUN), a qSOFA Score (quick Sequential Organ Failure Assessment), SIRS (systemic inflammatory response syndrome), and early warning scores such as NEWS and SEWS. CURB and CRB have not been validated in large studies and appear to have lower sensitivity and specificity than both PSI and SIRS. qSOFA, SIRS, and the warning system score, are primarily sepsis screening tools, and have proven ineffective in predicting mortality in pneumonia, since sepsis is only one of several causes of death precipitated by pneumonia.10 Which elements of the history and physical examination findings are associated with a diagnosis of pneumonia? Metlay et al. addressed this question in a systematic review evaluating history and physical findings against the criterion standard of findings on chest radiography.11 They reported likelihood ratios based on history and physical examination findings where there were two or more studies; however, an important limitation of this approach is that chest radiography is neither 100% sensitive nor specific for the diagnosis of pneumonia. These likelihood ratios are listed in Table 29.3. The most known scores for estimating pretest probability of pneumonia are the Heckerling Score and the Diehr Score, listed in Tables 29.4 and 29.5. Table 29.3 Positive and negative likelihood ratios for history, examination, and laboratory findings in diagnosing pneumonia Source: Data from [2].
Chapter 29
Pneumonia
Background
Characteristic
Points assigned
Demographic factor
Men
Age (years)
Women
Age (years)–10
Nursing home resident
+10
Coexisting illnesses
Neoplastic disease
+30
Liver disease
+20
Congestive heart failure
+10
Cerebrovascular disease
+10
Renal disease
+10
Physical examination findings
Altered mental status
+20
Respiratory rate ≥ 30 breaths/min
+20
Systolic blood pressure <90 mm Hg
+20
Temperature <35 °C (95 °F) or 40 °C (104 °F)
+15
Pulse ≥ 125 beats/min
+10
Laboratory and radiographic findings (if performed)
Arterial blood pH < 7.35
+30
Blood urea nitrogen level ≥ 30 mg/dL
+20
Sodium level < 130 mmol/L
+20
Glucose level ≥ 250 mg/dL
+10
Hematocrit < 30%
+10
Partial pressure of arterial 02 < 60 mm Hg or 02 Sat <90%
+10
Pleural effusion
+10
Class
Points
Mortality
I
<51
0.1%
II
51–70
0.6%
III
71–90
0.9%
IV
91–130
9.5%
V
>130
26.7%
Confusion
Elevated blood urea nitrogen (BUN) (>7 mmol/L)
Respiratory rate (≥30/min)
Blood pressure (systolic <90 mmHg or diastolic ≤60 mmHg)
Age ≥65 years
Clinical question
Finding
Likelihood ratio positive (LR+)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access




