Pleural Disorders in the Intensive Care Unit
Alexander C. Chen
Disorders of the pleura are found often in the intensive care unit (ICU). In some instances, pleural processes may be the primary cause of patients’ critical illness; in most cases, pleural disorders are recognized as secondary processes related to patients’ underlying illness. This chapter reviews the pathophysiology of these disorders and provides guidelines for managing these conditions in the ICU.
PLEURAL EFFUSIONS
The pleural space is a potential space between the visceral pleura, which covers the outer surface of the lung, and the parietal pleura, which lines the inside of the chest wall. In this space, there is a small amount of fluid present that functions to mechanically couple the lung to the chest wall and lubricate the interface of the visceral and parietal pleura. Pleural fluid normally results from the filtration of blood through high-pressure systemic blood vessels, and is drained from the pleural space through lymphatic openings in the parietal pleura that drain into parietal lymphatic vessels. In different disease states, fluid may originate from the interstitial spaces of the lungs, the intrathoracic lymphatics, the intrathoracic blood vessels, or the peritoneal cavity.
A pleural effusion is defined as an abnormal collection of fluid in the pleural space. Effusions occur when the rate of fluid formation exceeds the rate of fluid absorption. The most common causes of pleural effusions are shown in Table 16.1. Pleural effusions are commonly classified as being either exudative or transudative. An exudative pleural effusion implies that there is a disease process that is affecting the pleura directly, causing the pleura and/or its vasculature to be damaged. A transudative pleural effusion results when the pleura itself is healthy and implies that a disease process is affecting hydrostatic and/or oncotic factors that either increase the formation of pleural fluid or decrease the absorption of pleural fluid. Deciding if the pleura is injured or intact helps in formulating a concise differential diagnosis for potential causes (Table 16.2).
There are certain nonspecific signs and symptoms that may indicate the presence of a pleural effusion, but these are often difficult to ascertain in the ICU. Chest pain, particularly when sharp and made worse with breathing, can result from inflamed pleura in the presence of an effusion. Dyspnea is also common as the effusion can affect the mechanics of the diaphragm, cause a restrictive ventilatory defect, and/or cause compressive atelectasis leading to hypoxemia. The history can also help to reveal the cause of the effusion. For example, a patient with a fever and cough productive of sputum might have pneumonia causing the effusion. On physical examination, signs
that an effusion is present include dullness to percussion over the effusion, loss of fremitus, decreased breath sounds, crackles/egophony immediately above the effusion, and asymmetric diaphragmatic excursion with inspiration.
that an effusion is present include dullness to percussion over the effusion, loss of fremitus, decreased breath sounds, crackles/egophony immediately above the effusion, and asymmetric diaphragmatic excursion with inspiration.
TABLE 16.1 Common Causes of Pleural Effusions | |||||||
|---|---|---|---|---|---|---|---|
|
The majority of ICU patients will have their pleural effusion detected first by chest x-ray. Although a posterior-anterior (PA) and lateral chest x-ray is the preferred image, ICU patients typically have portable x-rays. Blunting of the costophrenic angle and a meniscus sign are the most common findings when an effusion is present. On the lateral chest x-ray, as little as 175 mL of fluid can be detected, while on the PA film it takes approximately 500 mL of fluid. Portable films are less sensitive, and often do not show the meniscus sign. Signs on the portable chest x-ray include loss of the diaphragm silhouette and increased basilar opacity with gradation over the entire hemithorax (more opaque at the base than the apex). Once a pleural effusion is detected radiographically, a lateral decubitus chest x-ray (where the dependent side is the side of the effusion) can quantitate the volume of fluid present and determine if the effusion is free-flowing or loculated. If the fluid is free-flowing, fluid can be detected as a straight line between the chest wall and lower border of the lung. Measurement of the distance between the chest wall and the lower border of the lung can give an idea of how much fluid is present. It is generally accepted that if this distance is >1 cm, then the amount
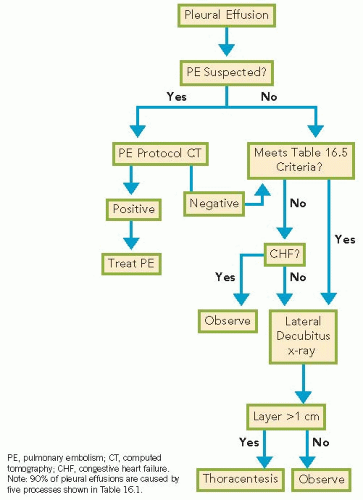
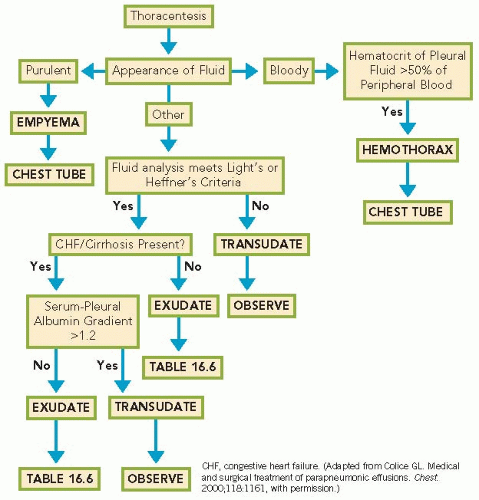
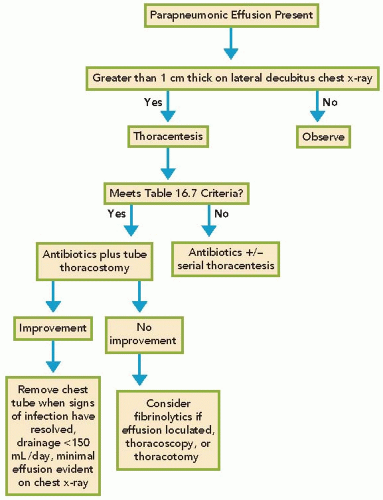
of fluid is significant. Diagnostic evaluation of the effusion from this point is discussed in Algorithms 16.1 and 16.2.
of fluid is significant. Diagnostic evaluation of the effusion from this point is discussed in Algorithms 16.1 and 16.2.
TABLE 16.2 Pathophysiological Causes of Pleural Effusions | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Other imaging modalities can also detect, quantify, and sometimes even characterize the pleural effusion. Chest computed tomography (CT) is a useful imaging tool in assessing pleural effusions and can help the clinician diagnose not only the presence of the effusion but also delineate possible causes. Different techniques yield different information, so it is important to select the appropriate technique:
Noncontrast CT scans can give a better idea of the amount of fluid within the pleural space, whether the fluid is loculated, and can detect abnormalities in the lungs that can be obscured by the effusion on standard chest x-ray.
Standard contrast CT scans also assess the pleural surface for abnormalities that might suggest empyema or pleural malignancy.
CT scans with contrast given by pulmonary embolism protocol can detect a pulmonary embolism as the cause of the effusion, but do not provide information about the pleural surface beyond that of a noncontrast CT.
CT scans cannot be done at bedside, a big disadvantage when dealing with a patient who is not stable enough to travel out of the ICU.
Ultrasound is beneficial for multiple reasons. It gives a real-time image that can be done at the bedside and used not only for diagnosis that an effusion is present but also guide diagnostic and therapeutic interventions (i.e., thoracentesis and tube thoracostomy). Ultrasound can detect whether the fluid is loculated or free-flowing, and can give clues as to whether the fluid is transudative, exudative, or even whether it is an empyema.
Once a pleural effusion is identified, it is important to attempt to diagnose the etiology of the effusion by obtaining a sample of the fluid for analysis. This is most often done by a thoracentesis. Thoracenteses can be safely performed as long as there is >1 cm of layered fluid on the lateral decubitus chest x-ray, even in patients receiving mechanical ventilation. One can remove a small amount of fluid for analysis or as much as 1,500 mL per drainage of fluid for both diagnostic and therapeutic goals (Algorithms 16.2, 16.3 through 16.4). The most common criteria used to separate exudates from transudates are Light’s criteria (Table 16.3). Heffner’s criteria (Table 16.4) can also differentiate exudate from transudate. Heffner’s criteria have a similar
sensitivity (98.4%), as Light’s criteria (97.9%) do not require simultaneous blood work to be drawn. Other specific tests (Tables 16.5 and 16.6) can help determine a specific diagnosis.
sensitivity (98.4%), as Light’s criteria (97.9%) do not require simultaneous blood work to be drawn. Other specific tests (Tables 16.5 and 16.6) can help determine a specific diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree