Key Clinical Questions
What are the valuable and helpful diagnostic testing modalities available in the evaluation of a pleural effusion?
How is empyema diagnosed and managed?
When does a malignant pleural effusion deserve serial drainage versus an indwelling drainage catheter versus pleurodesis?
What are the indications for chest tube placement (tube thoracostomy) in patients with a small pneumothorax?
When can a chest tube be removed, and how is that done?
Pleural Effusions
Pleural effusion complicates many different diseases making its precise incidence difficult to determine. The rate is estimated at 3.2 patients per 1000 population. The causes of effusions are varied (Table 243-1), with heart failure as the most common etiology. No data on hospital admission rate due to pleural effusions exists. Morbidity and mortality from pleural effusions correlates with the underlying etiology rather than the pleural effusion itself. Patients with pleural effusions secondary to malignancy or cirrhosis tend to have a poor prognosis while pleural effusions secondary to treatable or ameliorable conditions such as pulmonary emboli or surgery tend to have much better prognoses.
| System | Diagnosis |
|---|---|
| Cardiac |
|
| Pulmonary |
|
| Gastrointestinal | Cirrhosis or other causes of portal hypertension |
| Gynecologic | Ovarian hyperstimulation syndrome |
| Neoplastic |
|
| Rheumatologic/collagen vascular diseases |
|
| Renal |
|
| Occupational | Asbestosis |
| Trauma/iatrogenic injury |
|
| Idiopathic | Yellow nail syndrome |
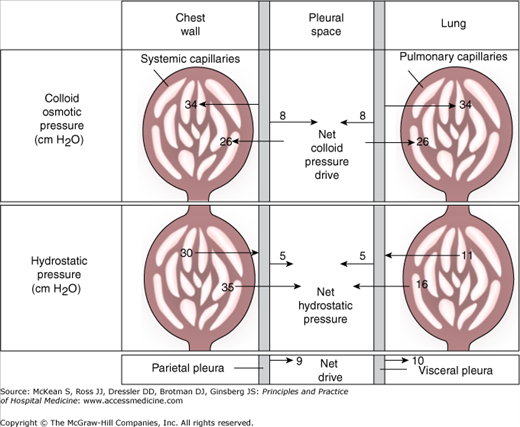
Normally, only a small 0.1 to 0.2 mL/kg or approximately 6 to 12 cc occupies the space between the visceral pleura lining the lung and the parietal pleura lining the chest wall and diaphragm. Fluid due to filtration from microvessels and stoma in the parietal pleura moves out of the pleural space by connecting to lymphatic channels. In the normal physiologic state the rate of pleural fluid turnover is 0.15 mL/hr, and in disease states this can be increased to approximately 30 ml/hr. A pleural effusion may collect in the pleural space due to increased production or decreased reabsorption of this fluid. Potential mechanisms of abnormal fluid accumulation include increased capillary permeability of the microvessels primarily in the parietal pleura, stoma obstruction, and decreased plasma oncotic pressures (Figure 243-1). In addition to serous fluid (hydrothorax), blood (hemothorax), lipid (chylothorax), and pus (empyema) may occupy the pleural space. Symptoms likely result from decreased chest wall compliance and stimulation of neurogenic receptors rather than direct compression of lung tissue.
Light’s Criteria classifies pleural effusions as either a transudate or an exudate (Table 243-2). Transudative pleural effusions indicate the presence of a systemic process, implicating organ systems other than the lungs. Volume overload medical conditions, including renal failure, heart failure, cirrhotic liver disease and hypoalbuminemia, cause transudates by overwhelming the capacity of the pulmonary lymphatics to absorb fluid. These types of effusions frequently occur bilaterally. In contrast, exudative pleural effusions indicate a local pleural process and necessitate a different diagnostic and therapeutic approach. These effusions form secondary to inflammation and obstruction of local lymphatic flow and most often occur unilaterally.
| Transudates | Exudates |
|---|---|
| Congestive heart failure | Pneumonia (parapneumonic effusion) |
| Cirrhosis with ascites | Cancer |
| Nephrotic syndrome | Pulmonary embolism |
| Peritoneal dialysis | Bacterial infection |
| Myxedema | Tuberculosis |
| Acute atelectasis | Connective tissue disease |
| Constrictive pericarditis | Viral infection |
| Superior vena cava obstruction | Fungal infection |
| Pulmonary embolism | Rickettsial infection |
| Urinothorax | Parasitic infection |
| Asbestos | |
| Meigs syndrome | |
| Pancreatic disease | |
| Uremia | |
| Chronic atelectasis | |
| Trapped lung | |
| Chylothorax | |
| Sarcoidosis | |
| Drug reaction | |
| Postmyocardial infarction syndrome (Dressler syndrome) |
Light’s criteria defining exudative effusions:
|
The usual symptoms of pleural effusion, dyspnea and chest pain, are nonspecific and many patients are asymptomatic. If incidentally noted on chest x-ray (CXR), the history should focus on symptoms and risk factors that may elucidate an underlying disease. Dyspnea usually only occurs in patients with very large effusions, but can occur with smaller effusions in patients with underlying lung disease and in approximately 50% of patients with malignant pleural effusions. The degree of breathlessness does not correlate with the size of the effusion. Chest pain caused by pleural inflammation is typically described as a stabbing or shooting pain. Deep inspiration and cough exacerbate the pain commonly at the site of the inflammation but may be referred anywhere in the thorax particularly the lower thorax and back. Placing pressure over the chest wall may provide partial relief.
Dullness to percussion, decreased tactile fremitus, egophany (e to a changes), and decreased breath sounds may suggest any process that leads to loss of air space, including an effusion greater than 300cc. Other physical exam findings will be related to the underlying disease process.
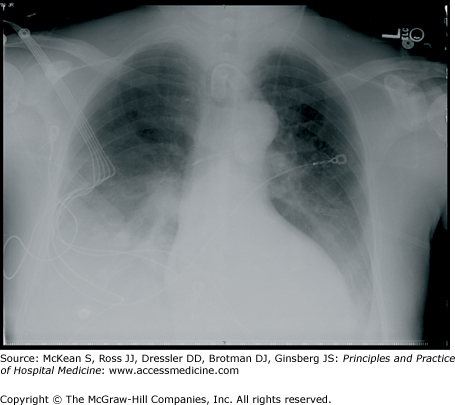
A simple upright anteroposterior (AP) or posteroanterior (PA) chest radiograph will detect fluid volumes of greater than 300 cc. If a pleural effusion is strongly suspected but not seen, a decubitus film (obtained with the patient lying with the affected side down) may detect as little as 50 cc of fluid and indicate whether the fluid is free flowing (Figure 243-2). A CXR will help delineate the effusion size and may provide clues to the cause. Bilateral effusions are more likely to be present in systemic diseases such as congestive heart failure or nephrotic syndrome. Unilateral massive pleural effusions which fill the hemithorax are more likely malignant. In addition to massive size, signs associated with malignancy include rib crowding, lobulated pleural thickening, elevation of the hemidiaphragm and mediastinal shift consistent with obstruction of a bronchus by an underlying carcinoma.
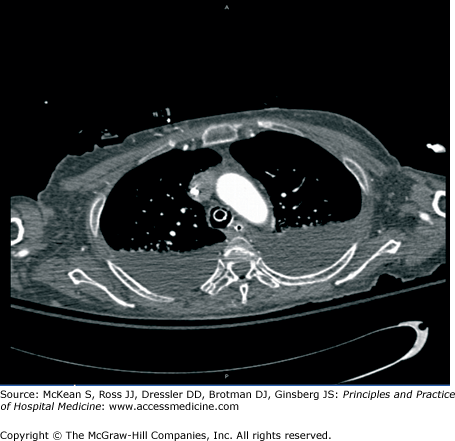
If further visualization of the pleural fluid is necessary to evaluate for the presence of loculations, non-contrast, non-high resolution computed tomography (CT) adequately quantifies the extent of loculation or the presence of a pleural rind prior to definitive drainage procedures (Figure 243-3). Chest CT will also identify parenchymal infiltrates, mediastinal lymphadenopathy, or pleural abnormalities. Chest CT findings which may represent pleural metastasis include pleural thickening, usually greater than 1 cm, or mediastinal pleural involvement. These findings are very specific but not sensitive. Key CT findings suggesting mesothelioma include unilateral effusion and nodular pleural thickening with involvement of the intralobular septa. CT using a pulmonary embolism (PE) protocol will be necessary to identify the presence of PE. See Chapter 108: Advanced Cardiothoracic Imaging.
Positron emission tomography (PET) CT with fluorine-18 labeled glucose has a very high sensitivity and negative predictive value (> 90% for each) for the detection of malignant pleural disease. Specificity and positive predictive value are not as good. False-positives occur in other conditions with increased pleural inflammation (eg, lupus pleuritis).
MRI provides better resolution than the CT, and better visualizes certain structures such as the chest wall and diaphragm. MR is superior to CT for complex pleural effusions and effusions with masses because it can possibly better define the mass dimensions and consistency. CT is often recommended above MRI to evaluate complex pleural effusions due to added expense and limited ability of MRI to visualize the lung parenchyma compared with CT.
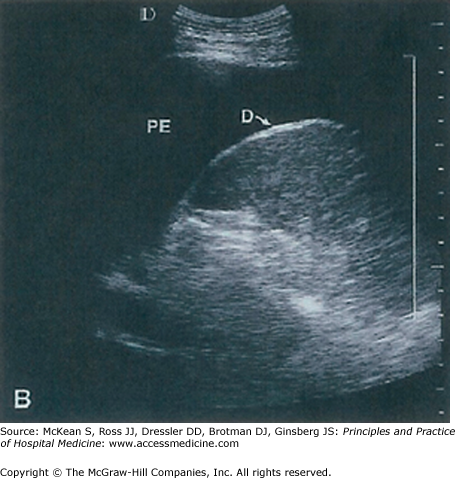
Ultrasound can distinguish solid from liquid pleural fluid with roughly 92% accuracy and combined with chest radiography, the accuracy increases to 98% (Figure 243-4).
Ultrasound helps determine the presence, size, extent, and location of the pleural effusion and thin echogenic bands in the effusion may suggest the presence of a complicated and loculated effusion. Ultrasound guidance for thoracentesis decreases the incidence of pneumothorax in nonventilated and ventilated patients. Ultrasound findings suggestive of malignancy include identification of either solid or hypoechoic pleural densities with irregular borders or increased cellular debris (increased density material within the pleural fluid).
Obtaining a specimen of the fluid for analysis should be done in all patients unless a clear etiology is suggested, such as the presence of pulmonary edema in patients with heart failure, bilateral pleural effusions in patients with the nephrotic syndrome or anasarca, left-sided effusion in patients with acute pancreatitis, or effusions arising in patients having undergone certain surgical procedures. However, if the effusion does not resolve in response to therapy, then a thoracentesis should be performed. See Chapter 117 Thoracentesis, which describes the proper technique for performing a thoracentesis.
The differential diagnosis of pleural effusions includes many clinical diagnoses and systemic disorders. Disorders can be identified based on the patient’s medical history, whether the fluid is a transudate or exudate (Table 243-2), and other characteristics of the pleural fluid (Table 243-3).
| Etiology or Type of Effusion | Gross Appearance | White Blood Cell Count (cells/μL) | Red Blood Cell Count (cells/μL) | Glucose | Comments |
|---|---|---|---|---|---|
| Malignant effusion | Turbid to bloody; occasionally serous | 1000 to < 100,000 M | 100 to several hundred thousand | Equal to serum levels; < 60 mg/dL in 15% of cases | Eosinophilia uncommon; positive results in cytologic examination |
| Uncomplicated parapneumonic effusion | Clear to turbid | 5000–25,000 P | < 5000 | Equal to serum levels | Tube thoracostomy unnecessary |
| Empyema | Turbid to purulent | 25,000–100,000 P | < 5000 | Less than serum levels; often very low | Drainage necessary; putrid odor suggests anaerobic infection |
| Tuberculosis | Serous to serosanguineous | 5000–10,000 M | < 10,000 | Equal to serum levels; occasionally < 60 mg/dL | Protein > 4.0 g/dL and may exceed 5 g/dL; eosinophils (> 10%) or mesothelial cells (> 5%) make diagnosis unlikely |
| Rheumatoid effusion | Turbid; greenish yellow | 1000–20,000 M or P | < 1000 | < 40 mg/dL | Secondary empyema common; high LD, low complement, high rheumatoid factor, cholesterol crystals are characteristic |
| Pulmonary infarction | Serous to grossly bloody | 1000–50,000 M or P | 100 to > 100,000 | Equal to serum levels | Variable findings; no pathognomonic features |
| Esophageal rupture | Turbid to purulent; red-brown | < 5000 to > 50,000 P | 1000–10,000 | Usually low | High amylase level (salivary origin); pneumothorax in 25% of cases; effusion usually on left side; pH < 6.0 strongly suggests diagnosis |
| Pancreatitis | Turbid to serosanguineous | 1000–50,000 P | 1000–10,000 | Equal to serum levels | Usually left sided; high amylase level |
Heart failure causes approximately 60% of all pleural effusions and greater than 90% of transudative effusions. Most pleural effusions due to heart failure are bilateral (75%), but they can also occur unilaterally, with right-sided effusion more common than left. Usually transudates, they may appear exudative after aggressive diuresis. They are straw colored and have low cell count with a mononuclear predominance. These effusions usually resolve with the treatment of the underlying congestive heart failure; they usually do not require diagnostic thoracentesis if a diuretic trial leads to effusion resolution over days to weeks.
Most parapneumonic effusions are sterile, clear exudates that generally resolve with antibiotic treatment and rarely require chest tube drainage. However, a minority (5%) are complicated with loculations and fibrin deposits. The fluid may be infected, as suggested by a low glucose, an elevated LDH, and a low pH on fluid analysis. This stage of pneumonia will not resolve with antibiotics alone and predisposes the patient to complications such as continued pleural sepsis and empyema.
Empyema progresses through three stages: exudative, fibrinopurulent, and organizing (Table 243-4). In the exudative stage, the pleural fluid is nonviscous and freely flowing, with minimally inflamed pleural membranes, and the patient is likely to respond to antibiotics but may require drainage according to Thoracic Society Guidelines. The early fibrinopurulent stage is characterized by increasing viscosity of the fluid, thickening of the pleural membranes, and formations of intrapleural loculations. Patients may respond to antibiotic therapy alone but often require emptying of the pleural space via chest tube drainage. In the organized stage, the patient will likely require surgical debridement of the pleural peel that has formed.
| Exudative | Fibrinopurulent | Organizing | |
|---|---|---|---|
| Fluid viscosity | Free flowing | Increased | Loculations, pus |
| Cells | Neutrophils | Fibroblasts | Fibroblasts and debris |
| pH, glucose | Normal | Decreased | Low |
| Treatment | Antibiotics, drainage | Antibiotics, drainage | Surgery |
All patients with pleural infections should be treated with antibiotics. The proper choice of antibiotics depends on the presumed site of the development of the empyema. In a community-acquired empyema, the primary organisms include streptococcal pneumonia, gram-negative organisms and anaerobic organisms. A third-generation cephalosporin plus metronidazole to cover methicillin-sensitive Staphylococcus aureus (MSSA), gram-negative organisms, and anaerobic organisms. Aminoglycosides should be avoided secondary to poor pleural penetration. For health care associated or hospital-acquired empyema, antibiotic coverage should be broadened to include methicillin-resistant Staphylococcus aureus (MRSA), but anerobic coverage is less important. Piperacillin-tazobactam plus vancomycin are reasonable initial choices.
Drainage of a parapneumonic effusion may be required to prevent progression through the three stages of empyema. Parapneumonic effusions are divided into four categories and assigned a risk for poor outcomes. Large volume drainage intervention, usually by tube thoracostomy procedure, is generally required in three circumstances: (1) effusion > 50% of the hemithorax or loculated effusion or effusion with thickened parietal pleura; (2) fluid-positive bacterial Gram stain or culture or pus; (3) fluid pH < 7.2 (see section below on Tube Thoracostomy). Other circumstances that may meet indication for pleural fluid drainage include glucose < 60 or LDH > 3 times upper limit of normal. Fibinolytic therapy may be considered for loculated pleural effusions, based on several uncontrolled trials showing greater fluid removal.
While parapneumonic effusions and especially empyema may commonly lead to pleural fluid with a low pH, other etiologies may be considered in patients with pleural fluid with a low pH (Table 243-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree