CHAPTER 125
Plantar Fasciitis
(“Heel Spur”)
Presentation
Patients seek help because of gradually increasing inferior heel pain that has progressed to the point of inhibiting their normal daily activities. This fasciitis can develop in anyone who is ambulatory but appears to be more common in athletes (especially runners), those older than 30 years of age, those who stand for prolonged periods of time, and the overweight. There is no defining episode of trauma. The most distinctive clue is exquisite pain in the plantar aspect of the heel when taking the first step in the morning. There is gradual improvement with walking, but as the day progresses, the pain may insidiously increase. First-step pain is also present after the patient has been sitting. The heel is tender to palpation over the medial calcaneal tubercle and may be exacerbated by dorsiflexion of the ankle and toes, particularly the great toe, which creates tension on the plantar fascia. Often the midfascia is tender to palpation too. There is generally no swelling, heat, or discoloration.
What To Do:
 Obtain a general medical history in addition to details of the patient’s current illness. Patients with systemic conditions and those with potential infection will have other areas of involvement or bilateral involvement. Other clues might include a history of diabetes, chemotherapy, retroviral infection, a rheumatologic disorder, or another similar chronic condition. A history of focal pain after localized trauma indicates a contusion to the heel (sometimes referred to as “fat pad syndrome”).
Obtain a general medical history in addition to details of the patient’s current illness. Patients with systemic conditions and those with potential infection will have other areas of involvement or bilateral involvement. Other clues might include a history of diabetes, chemotherapy, retroviral infection, a rheumatologic disorder, or another similar chronic condition. A history of focal pain after localized trauma indicates a contusion to the heel (sometimes referred to as “fat pad syndrome”).
 Increased levels of activity or exercise may indicate that overuse is the cause of the pain. Other potential precipitating factors include recent weight gain, a change in footwear, inappropriate or worn-out shoes, or working on cement floors. If the patient describes the sensation as “burning”, “tingling,” or “numbness,” the cause may be peripheral nerve entrapment. Pain that develops in the evening after physical activity is often seen early in stress fracture.
Increased levels of activity or exercise may indicate that overuse is the cause of the pain. Other potential precipitating factors include recent weight gain, a change in footwear, inappropriate or worn-out shoes, or working on cement floors. If the patient describes the sensation as “burning”, “tingling,” or “numbness,” the cause may be peripheral nerve entrapment. Pain that develops in the evening after physical activity is often seen early in stress fracture.
 Perform a careful foot examination to determine the location of the point of maximal tenderness and to detect any signs of infection, atrophy of the heel pad, bony deformities, bruising, or breaks in the skin. Diagnosis is made by eliciting pain with palpation in the region of the medial plantar tuberosity of the calcaneus (the origin of the plantar fascia). Pain may be worsened by passive dorsiflexion of the foot.
Perform a careful foot examination to determine the location of the point of maximal tenderness and to detect any signs of infection, atrophy of the heel pad, bony deformities, bruising, or breaks in the skin. Diagnosis is made by eliciting pain with palpation in the region of the medial plantar tuberosity of the calcaneus (the origin of the plantar fascia). Pain may be worsened by passive dorsiflexion of the foot.
 Radiographs can be deferred and are not always required. However, as clinical findings demand, they may be obtained to look for stress fractures of the metatarsals, tumors, osteomyelitis, calcifications, or spurs, which are located on the leading edge of the calcaneal inferior surface.
Radiographs can be deferred and are not always required. However, as clinical findings demand, they may be obtained to look for stress fractures of the metatarsals, tumors, osteomyelitis, calcifications, or spurs, which are located on the leading edge of the calcaneal inferior surface.
 Unless contraindicated, prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) for 2 to 3 weeks.
Unless contraindicated, prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) for 2 to 3 weeks.
 Have the patient wear soft (viscoelastic) heel cushions, such as Bauerfeind Viscoheel (Bauerfeind USA, Kennesaw, Ga.), and a sports shoe with a firm, impact-resistant heel counter and longitudinal arch support. AirCast (DJO Global, Vista, Calif.) provides an alternative pneumatic compression dressing for the foot and ankle (AirHeel).
Have the patient wear soft (viscoelastic) heel cushions, such as Bauerfeind Viscoheel (Bauerfeind USA, Kennesaw, Ga.), and a sports shoe with a firm, impact-resistant heel counter and longitudinal arch support. AirCast (DJO Global, Vista, Calif.) provides an alternative pneumatic compression dressing for the foot and ankle (AirHeel).
 Use of dorsiflexion night splints may be particularly beneficial in preventing the severe pain that often comes with the first steps in the morning on awakening. However, compliance is low.
Use of dorsiflexion night splints may be particularly beneficial in preventing the severe pain that often comes with the first steps in the morning on awakening. However, compliance is low.
 Ice massage can be helpful. The patient can roll his heel over a can of frozen juice concentrate, followed by stretching.
Ice massage can be helpful. The patient can roll his heel over a can of frozen juice concentrate, followed by stretching.
 Athletes should practice stretching the Achilles tendon before running by placing the sole flat, leaning forward against a counter or table, and slowly squatting while keeping the heel on the ground. Others may stand, wearing tennis shoes, on the edge of a step, facing up stairs, slowly lowering their heels until they feel a pulling sensation in their upper calf. Hold for ½ to 1 minute or until there is pain. Repeat three times daily, increasing the stretch time to a maximum of 3 minutes per session. Although there may be a transient increase in pain after beginning this program, the heel pain usually begins to resolve within several weeks.
Athletes should practice stretching the Achilles tendon before running by placing the sole flat, leaning forward against a counter or table, and slowly squatting while keeping the heel on the ground. Others may stand, wearing tennis shoes, on the edge of a step, facing up stairs, slowly lowering their heels until they feel a pulling sensation in their upper calf. Hold for ½ to 1 minute or until there is pain. Repeat three times daily, increasing the stretch time to a maximum of 3 minutes per session. Although there may be a transient increase in pain after beginning this program, the heel pain usually begins to resolve within several weeks.
 Have the patient reduce ambulatory activities and try to keep weight off the foot whenever possible. Also, have female patients avoid thin-soled flats and high heels. Have runners decrease their mileage by 25% to 75% and avoid sprinting, running on hard surfaces, and running uphill. A program of cross training incorporating swimming and bicycling maintains cardiovascular fitness while decreasing stress on the feet.
Have the patient reduce ambulatory activities and try to keep weight off the foot whenever possible. Also, have female patients avoid thin-soled flats and high heels. Have runners decrease their mileage by 25% to 75% and avoid sprinting, running on hard surfaces, and running uphill. A program of cross training incorporating swimming and bicycling maintains cardiovascular fitness while decreasing stress on the feet.
 Although not often easily applied, recommend weight loss for those patients who are overweight.
Although not often easily applied, recommend weight loss for those patients who are overweight.
 When conservative measures have failed and there is an exquisitely tender area on the medial calcaneus, local corticosteroid injection may speed recovery. Use with care because there may be increased risk of plantar fasciitis rupture. Palpate the heel pad to locate the point of maximum tenderness. Place the patient in the lateral recumbent position with the lateral aspect of the painful heel resting against the examination surface. Cleanse the skin with povidone-iodine, and using a 25-gauge, 1¼- to 1½-inch needle, inject the area with 2 mL of 0.25% or 0.5% of bupivacaine (Marcaine) along with betamethasone (Celestone Soluspan), 1 mL of 6 mg/mL, or methylprednisolone (Depo-Medrol), 1 mL of 40 mg/mL. Enter medially, perpendicular to the skin, and advance the needle directly down past the midline of the width of the foot to the plantar fascia until you can feel its thick and gritty substance. Inject the mixture slowly and evenly through the middle one third of the width of the foot while the needle is being withdrawn (Figure 125-1). Finish by putting the injected region through passive range of motion to spread the medication. Patients should be cautioned that they may experience worsening symptoms during the first 24 to 48 hours. This may be related to a possible steroid flare, which can be treated with ice and NSAIDs. Two or three injections at intervals of several weeks may be necessary.
When conservative measures have failed and there is an exquisitely tender area on the medial calcaneus, local corticosteroid injection may speed recovery. Use with care because there may be increased risk of plantar fasciitis rupture. Palpate the heel pad to locate the point of maximum tenderness. Place the patient in the lateral recumbent position with the lateral aspect of the painful heel resting against the examination surface. Cleanse the skin with povidone-iodine, and using a 25-gauge, 1¼- to 1½-inch needle, inject the area with 2 mL of 0.25% or 0.5% of bupivacaine (Marcaine) along with betamethasone (Celestone Soluspan), 1 mL of 6 mg/mL, or methylprednisolone (Depo-Medrol), 1 mL of 40 mg/mL. Enter medially, perpendicular to the skin, and advance the needle directly down past the midline of the width of the foot to the plantar fascia until you can feel its thick and gritty substance. Inject the mixture slowly and evenly through the middle one third of the width of the foot while the needle is being withdrawn (Figure 125-1). Finish by putting the injected region through passive range of motion to spread the medication. Patients should be cautioned that they may experience worsening symptoms during the first 24 to 48 hours. This may be related to a possible steroid flare, which can be treated with ice and NSAIDs. Two or three injections at intervals of several weeks may be necessary.
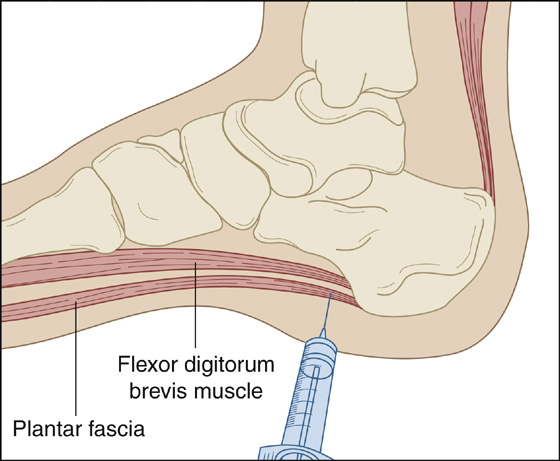
Figure 125-1 Proper location for injection.
 Studies are presently ongoing to evaluate the efficacy of injecting botulinum toxin into the foot. Initial studies have shown benefit; however, more investigation needs to be performed before suggesting this as a treatment.
Studies are presently ongoing to evaluate the efficacy of injecting botulinum toxin into the foot. Initial studies have shown benefit; however, more investigation needs to be performed before suggesting this as a treatment.
 In all cases, orthopedic follow-up should be arranged.
In all cases, orthopedic follow-up should be arranged.
What Not To Do:
 Do not inject into the heel pad itself, which may cause fat atrophy.
Do not inject into the heel pad itself, which may cause fat atrophy.
Discussion
The plantar fascia provides an intimate attachment to the overlying skin and functions to provide protection to the underlying muscles, tendons, arteries, and nerves. The fascia assists in the maintenance of the foot arch and keeps the foot in relative supination through the push-off phase of ambulation. During heel strike, the plantar fascia remains supple and allows the foot to adjust to the ground surface and absorb shock. Then, during the toe-off phase of ambulation, the plantar fascia becomes taut and thereby renders the foot a rigid lever, thus facilitating forward movement.
Plantar fasciitis, the most common cause of heel pain in adults, typically results from repetitive use or excessive load on the fascia. Persons who are overweight, female, or older than 40 years or who spend long hours on their feet are especially at risk for developing plantar fasciitis. Athletes, especially joggers and runners, also develop plantar fasciitis.
Tightness of the Achilles tendon contributes to increased tension on the plantar fascia during walking or running and is therefore an important contributor to plantar fasciitis. Stretching of the Achilles tendon can therefore alleviate some of the pain caused by plantar fasciitis. It should be relayed to the patient, however, that this can initially make the discomfort worse.
Mechanical causes of heel pain are generally synonymous with plantar fasciitis, but some cases are enigmatic in etiology and are deemed idiopathic. Although the word fasciitis implies inflammation, recent research indicates that it is more likely to be a noninflammatory, degenerative process that might be more appropriately called plantar fasciosis.
Acute onset of severe plantar heel pain after trauma or vigorous athletics may indicate rupture of the plantar fascia. The patient may have heard a “pop” or felt a tearing sensation. Findings suggestive of rupture include a palpable defect at the calcaneal tuberosity accompanied by localized swelling and ecchymosis.
If conservative treatment of plantar fasciitis fails to alleviate symptoms, radiographs are advisable to check for other causes of heel pain, such as stress fractures, arthritis, or skeletal abnormalities. Radiographs may show a spur on the leading edge of the calcaneal inferior surface, but this radiographic finding is not pathognomonic of the condition, nor is it necessary for the diagnosis. It is a common finding in the asymptomatic foot and is generally not the cause of a patient’s heel pain.
If a patient with heel pain has persistent bilateral involvement, systemic disease may be the cause. Ankylosing spondylitis, Reiter disease, rheumatoid arthritis, systemic lupus erythematosus, and gouty arthritis all may cause medial calcaneal pain. Calcaneal bursitis and fat pad atrophy are other potential causes of heel pain.
The benefits of using injectable steroids for plantar fasciitis has become somewhat controversial; therefore they should be used only when conservative measures have failed. The main concern with the use of steroid injections is delayed rupture of the plantar fascia. Rupture is typically associated with resolution of plantar fasciitis symptoms, but a majority of these patients may go on to develop long-term sequelae, such as longitudinal arch strain, lateral plantar nerve dysfunction, stress fracture, and development of hammertoe deformity.
In most patients with plantar fasciitis, conservative therapy works best. Symptoms will usually resolve, but this may take many weeks or months. For the 10% or fewer with heel pain that persists for at least 1 year despite treatment, surgery should be considered, especially when the symptoms of plantar fasciitis are disabling. Determining the source of repetitive stress to the plantar fascia and addressing it as part of the treatment is crucial to both facilitating recovery and reducing the risk of recurrence. Chronic recurrences may indicate biomechanical imbalances in the foot, which may resolve with custom orthotics from a podiatrist.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


