Placement of Feeding Tubes
Ulises Torres
Rupal Patel
I. GENERAL PRINCIPLES
A. Introduction.
1. Enteral nutrition (EN) in the critically ill patient compared to parenteral nutrition.
a. Maintains the integrity of the intestinal mucosal barrier.
b. Decreases infectious morbidity and improves wound healing.
c. Reduces cost.
d. EN should be instituted if possible in the first few days after admission to the critical care unit unless the patient exhibits signs of intestinal ischemia or is hemodynamically compromised.
B. Classification.
1. Administration of EN can be classified according to anatomic location of the feeding tube. The selection of the device requires an evaluation of the patient’s disease state, gastrointestinal (GI) anatomy, past surgical history, gastric and jejunal motility, and the estimated time of therapy.
a. Short-term administration (<4 weeks).
i. Can be administered through nasogastric (NG) or orogastric (OG) (polyvinyl chloride tube, 16 or 18 Fr), nasoduodenal, or nasojejunal fine-bore tubes (silicone or polyurethane feeding tube, 6 to 14 Fr).
ii. Multilumen tubes allow gastric decompression while delivering feeding formula into the jejunum. These are not required in the ICU unless gastric feeding intolerance is present.
b. Long-term administration (>4 weeks).
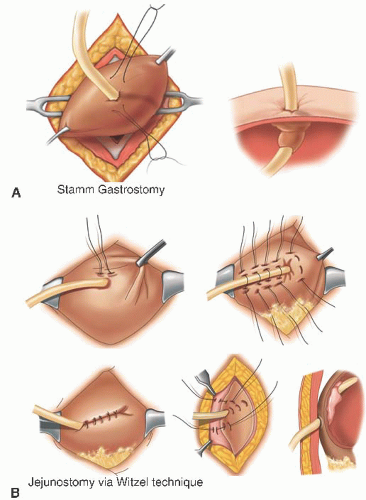
i. Access routes for long-term EN include esophagostomy, gastrostomy, duodenostomy, gastrojejunostomy (Moss tube), and jejunostomy. These tubes are for patients with persistent dysphagia (Fig. 13-1).
2. Anatomic location of the feeding tube.
a. Gastric feeding relies on a functional stomach free of delayed gastric emptying, obstruction, or fistula.
b. Feeding into the duodenum does not decrease regurgitation but has demonstrated better levels of nutrition than gastric feedings; infusion into the jejunum is associated with the lowest risk of aspiration and is indicated for patients with gastroparesis and pancreatitis and also for those patients who need gastric decompression while feeding distally in the bowel (gastrojejunostomy tube).
C. Contraindications for surgical placement of tube (percutaneous endoscopic gastrotomy [PEG] and open technique).
1. Absolute contraindications include coagulopathy, strictures of pharynx or esophagus (contraindication for placement of gastroscope), and abdominal wall infections.
2. Relative contraindications include severe ascites, gastric cancer, gastric ulcer, and recent banding of bleeding esophageal or gastric varices and morbid obesity.
D. Contraindications for tube feeding.
1. Absolute contraindications include intestinal obstruction, severe upper GI hemorrhage, or severe mesenteric ischemia.
2. Relative contraindications include
a. Gastric feeding in patients with increased risk of pulmonary aspiration.
b. Enterocutaneous fistulas, severe inflammatory bowel disease, severe malabsorption, and severe short-gut syndrome.
II. PROCEDURE
A. Placement of nasoenteral feeding tubes or short-term feeding tubes.
1. Appropriate length of the feeding tube: stomach, 30 to 36 in.; duodenum, 43 in.; and jejunum, at least 48 in. (Most tubes are radiopaque and have a tungsten-weighted tip or a stylet to facilitate passage into the duodenum.) Use of an electromagnetic system that allows real-time tracking of insertion of the feeding tube will minimize the risk of placement of the tube within the tracheobronchial tree (Fig. 13-2).