Chapter 9 Physiotherapy and occupational therapy in the hypermobile adult
Introduction
Joint hypermobility syndrome (JHS) is under-recognized, poorly understood and, sadly, often poorly managed (Beighton 1999). The syndrome does not necessarily cause problems and for many individuals it can be an asset, amply illustrated in the world of music, dance and sport. For others it can be a liability, producing significant problems which are often ignored by the medical profession (Phipps 2003, HMSA 2006). Early recognition and appropriate management can decrease suffering, reduce the need for unnecessary tests and invasive procedures, help to avoid surgery, reduce chronic pain and fear (Cherpel & Marks 1999) and prevent the destructive spiral into depression and physical deconditioning. It is the aim of this chapter to discuss the presentation of the syndrome to aid recognition and diagnosis by primary care practitioners and to explore assessment and management strategies to decrease suffering and disability, increase function and enable the hypermobile individual to effectively self-manage the condition.
Presentation
Assessment
Pain is the most common complaint, often being widely distributed, involving several joints and areas of the body, and varying in duration from acute (15 days) to as long as 45 years (El-Shahaly & El-Sherif 1991). A typical presentation is illustrated in Keer & Grahame (2003), and Simmonds & Keer (2007). The onset frequently occurs in childhood or adolescence, particularly in girls between the ages of 13–19 years, with 75% of hypermobile adolescents developing symptoms by the age of 15 (Kirk et al 1967) (Chapters 2, 10 and 11). Anecdotally, onset is also often associated with trauma, pregnancy, childbirth, a change in physical activity, such as a marked decrease contributing to deconditioning, or an unresolved joint problem which leads to compensatory strategies producing other joint problems. In addition, the patient will often report past episodes of medical or therapy intervention which were unhelpful and may even have exacerbated their symptoms. Exploring their history in this respect not only helps to identify potential generalized hypermobility, but will also give valuable information regarding what has not helped in the past, so that mistakes are not repeated.
It is unusual for pain to be the only symptom, so asking for details about other symptoms can give clues to tissues or systems which may be potential causes of the problem and may require examination (Table 9.1). Stiffness is a very common complaint and may seem at odds with the range of movement on testing. This is a subjective feeling of stiffness and although the range of movement may appear normal it may not be normal for that particular patient. Asking ‘have you ever been able to touch the floor with your palms flat’ (Oliver 2000) can be a useful indicator of previous hypermobility, a factor that is acknowledged in both the 5-point questionnaire (Hakim & Grahame 2003) and the Brighton Criteria (Grahame et al 2000) (Chapter 1). The reports of stiffness may also be a reflection of decreasing flexibility with age, or due to injury or muscle stiffness/spasm. Paraesthesiaes are frequently non-dermatomal and there may be an increased disposition to development of a neuropathy (Francis et al 1987, March et al 1988).
Table 9.1 Common symptoms reported and possible tissue or system at fault
| Symptom Reported | System to be Examined |
|---|---|
| Stiffness | Muscle system (muscular tension) |
| ‘Feeling like a 90 year old’ | Joints Hormonal |
| Audible clicking, popping, clunking, sensations of subluxation, vulnerability, instability or frank dislocation | Motor control Stability system |
| Sensations of parasthesiae, tingling, numbness, deadness | Neural system |
| Tiredness, fatigue, faintness, feeling unwell, flu-like symptoms | Autonomic nervous system Physical deconditioning |
Aggravating factors to determine the Severity, Irritability & Nature (SIN) (Maitland 1986) are not clear cut. Latency is frequently a problem, with symptoms developing several hours or even a day later, making it very difficult to identify the aggravating activity. This makes it difficult to judge the response to a physical examination and treatment. Careful questioning about the individual’s response to physical activity will help, although caution is advised with regard to the amount and vigour of testing, particularly initially.
Hypermobile individuals frequently dislike static postures and report difficulty with standing still, such as when queuing, shopping or attending exhibitions, and sitting for prolonged periods of time. Hypermobility of the spine was found to increase the prevalence of back pain in industrial workers working in standing/sitting postures (Larsson et al 1995) and hypermobility of the spine and knees produced symptoms in musicians due to sustained standing postures (Larsson et al 1993).
In addition, hypermobile individuals dislike repetitive activities, being more likely to develop musculoskeletal lesions (Acasuso-Diaz et al 1993) and reporting an increased frequency of previous episodes and more recurrent episodes of overuse soft tissue lesions such as bursitis, tendonitis and fasciitis at a single site (Hudson et al 1995, 1998) as well as fibromyalgia (Goldman 1991, Acasuso-Diaz & Collantes-Estevez 1998) (Chapter 5). It is often the case that pain or injury has occurred with minimal provocation during everyday activities, such that the patient cannot say what has brought the pain on. This can be very frustrating for the therapist and patient alike, but it is worth viewing this as a valuable piece of the jigsaw, leading to more accurate recognition and diagnosis of generalized hypermobility.
Certain aspects of the patient’s history can be valuable in providing clues to hypermobility. Back and knee pain are reported most commonly as a source of pain in childhood (Biro et al 1983) (Chapter 11). Individuals who no longer demonstrate hypermobility due to age, injury or stiffness secondary to pain, may be able to confirm that they were more flexible when younger, or that there is a family history of increased flexibility. Studies have shown that 27–65% of patients with symptomatic hypermobility seen in clinic had relatives with hypermobility (Finsterbush & Pogrund 1982, Biro et al 1983, Bridges et al 1992). There may also be evidence of involvement of other connective tissue, because patients report that they bruise easily (Al-Rawi et al 1985, Kaplinsky et al 1998) and there is frequently a history of varicose veins, hernia, or prolapses (Wynne-Davies 1971, Al-Rawi et al 1985, El-Shahaly & El-Sherif 1991).
Hypermobile individuals frequently recount a long history of soft tissue injuries, strains and sprains (Acasuso-Diaz et al 1993), which can be suggestive of vulnerable tissues or areas of vulnerability due to increased tissue laxity, poor control and muscular weakness. Dislocations and subluxations are more common (Finsterbush & Pogrund 1982). This should prompt a holistic assessment looking at the functioning of the whole body, to identify reasons why a particular area is causing a problem. How well the individual recovered from previous injury/problems will have a bearing on subsequent treatment, expectations and prognosis, particularly as there is anecdotal evidence of poor healing and a slower recovery in this patient group (Russek 2000).
In addition, questions relating to gender, age, ethnicity, weight, details of work or daily activities, leisure and exercise or sport activities will help to give a full picture of the impact of JHS on the individual. It is also important to ask special questions regarding general health and medical history in terms of surgery or illnesses, related or not, such as fatigue, chronic fatigue syndrome and fibromyalgia, as well as details of medication, so that the physical examination can be tailored to the individual’s presentation without risking a flare-up. Discussing medication may also highlight the possibility of JHS as a diagnosis, because there is often a poor response to non-steroidal anti-inflammatory drugs (NSAIDs), and local anaesthetics have been reported as less effective in EDS type III patients (Arendt-Neilson 1990, Hakim et al 2005).
Examination
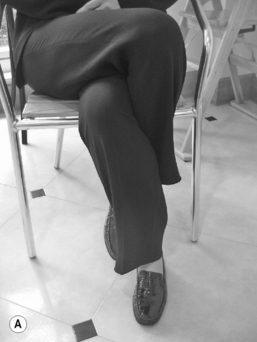
Observation of the patient’s mannerisms and postures during history-taking may give an indication of hypermobility. Contact of the hand to the face may reveal hyperextension of the digits, constantly changing position or fidgeting and/or sitting in an unusual posture (legs wound round each other, slumped to the side or resting on the lateral border of the feet) are familiar sightings (Fig. 9.1).
Skin is a very important feature and helps to confirm a diagnosis of hypermobility. To the touch it is silky, soft, extensible and thin. Elasticity can be tested by picking up a section from the back of the hand between the thumb and first finger (Chapter 2). Wounds may show poor healing with a thinner or papery scar. There may be stretch marks (striae atrophicae) not associated with weight loss or pregnancy, which appear during the growth phase in certain areas such as across the lumbar spine and pelvis, around the hips, thighs and shoulders.
The Beighton scale (Beighton et al 1973) gives an indication of hypermobility in certain joints (JHM), and while it is quick and easy to use in the clinic, it is limited in its application as only a few joints are tested. Other scales are discussed in more detail in Chapter 1. A diagnosis of JHS can be confirmed using the Brighton Criteria (Grahame et al 2000) which assesses the effect of weaker connective tissue on the body as a whole, but its use is primarily as a research tool. In an out-patient setting, making a diagnosis of JHS will depend on a thorough history and physical examination of the whole body.
Pain is also thought to arise because the connective tissue (ligament, tendon, muscle, capsule) in hypermobile individuals is more lax and less resilient and suggests a predisposition to the effects of trauma (acute and chronic) from overuse and misuse. Microtrauma occurs more frequently and with less provocation (Acasuso-Diaz et al 1993, Hudson et al 1998), meaning that even everyday activities can be the cause of tissue trauma and pain. For some, there is the added problem of subluxation, dislocation or instability which can produce, or be the result of, poor movement control. The hypermobile individual has an increased susceptibility to instability due to increased extensibility in the connective tissue restraints (capsule, ligament, muscle, tendon), affecting the passive control system, decreased muscle tone and strength, affecting the active control system, and deficient proprioceptive acuity (Mallik et al 1994, Hall et al 1995), affecting the neural and feedback control system, which is further outlined in Panjabi’s model of stability (1992) (Chapter 12.8).
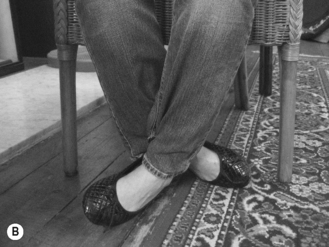
Poor movement control has the potential to lead to further joint problems, setting off a chain reaction or ‘domino’ effect whereby a problem in one joint can develop into widespread pain affecting many joints over a period of time. Increased healing time may lead to more well-developed compensatory strategies which affect other areas, progressing onto chronic pain and physical deconditioning (Fig. 9.2).
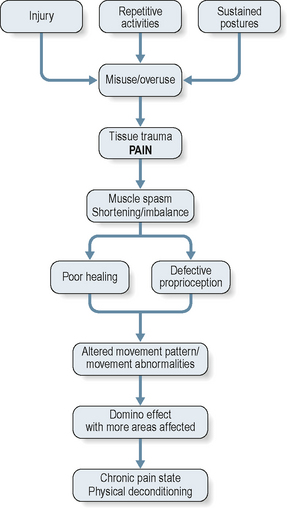
It is helpful to think in terms of compensatory relative flexibility, a concept proposed by Sahrmann (2002). This states that movement occurs more readily at a joint with less stiffness than at a joint with relatively more stiffness. For example, hamstring muscle tension or stiffness either as a result of habitually sitting for long periods, or as a result of injury, will inhibit movement at the hip into flexion during forward bending, potentially leading to overflexion in the spine. It is common to see decreased hip flexion and increased spinal flexion in hypermobile individuals and this may be contributing to low-grade irritation and strain to lumbar spine tissues, producing pain. Figure 9.3a is an example of this and is in contrast to Figure 9.3b which shows well-balanced full range flexion in a hypermobile individual.
There is evidence of neurophysiological defects such as pain enhancement and autonomic dysfunction (Gazit et al 2003) (Chapter 6.1), which will have the effect of increasing disability, leading to less activity and a vicious spiral of chronic pain and physical deconditioning (Rose 1985). Psychological distress is common, with concerns and difficulties occurring around work, home life and raising children, as well as fear of pain, serious illness or permanent disability. Individuals have often had to withstand years of having their complaints dismissed, being misunderstood or not being believed by the medical profession at large (Phipps 2003). This has, understandably in some cases, led to anger, confusion and depression.
The physical examination starts with observation. The patient, undressed to their underclothes and standing in their normal stance, is assessed from all four directions (front, back and each side) and compared with what is considered the ideal skeletal alignment. This is a standard based on sound scientific principles which involves minimal stress and strain on the body tissues and allows maximal efficiency (Kendall et al 1993). Details of a thorough postural examination are given in Kendall et al (1993) and should include postural alignment, symmetry and weight distribution from head to toe.
Hypermobile individuals show a tendency to rest at the end of joint range and have poor postural alignment. Even if they are initially able to stand or sit in a good position, it is difficult to sustain the position for long periods. It is easier for their bodies to take the path of least resistance and settle into a position which requires decreased muscle work, resting on tension in their soft tissues. Familiar postures are slumped sitting, standing with hyperextended knees and hips (Fig. 9.4) and hanging on the hip. This leads to stress and strain in the collagenous tissues. If these postures are sustained, fluid is forced out and tissue nutrition is adversely affected. The tissue undergoes creep, which leads to deformation, stretching and weakening over time. There is also a weakening of surrounding muscles through disuse and changes in how and where load is transferred through the kinetic chain. Hyperextension at the knee provides a good illustration (Kendall et al 1993), with the patella displaced caudally and contact of the femoral condyles on the tibial plateau shifted more anteriorally. This has the potential to weaken and damage tissue, disrupt nutrition of joint tissue and produce pain. There are also effects along the kinetic chain at a distance from the knee, with the ankle joint held in plantarflexion, producing changes in the calf muscles, and also into the hip and lumbar spine.
Active movement
It is helpful to examine the effect of moving one area in the context of the whole body. This may mean examining ease and range of movement in all areas of the spine as well as some peripheral joints, if symptomatic. For instance, full flexion at the shoulders may only be possible with lumbar spine extension, because latissimus dorsi is shortened or overactive (Sahrmann 2002), producing an area of relative stiffness. This has the potential to lead to overuse injuries at the shoulder through repetition of an overhead activity, particularly relevant in the sports person. It would therefore be necessary to assess the shoulder and whole spine. For the less active, it may be as simple as increased pronation in the midfoot as a result of stiffness at the ankle into dorsiflexion, either through talo-crural stiffness (from injury) and/or soft tissue shortness/tightness in the calves or higher in the kinetic chain. Poor movement patterns may also be due to muscle deconditioning and weakness. A case highlighted in Simmonds and Keer (2008) involved an individual lifting with poor muscle control around the wrist which led to the wrist being pushed into ulnar deviation under load, causing strain to the ligament and tendon on the radial side. Close questioning and detailed examination of everyday habitual activities can highlight significant problems, which can be easily rectified once identified.
Functional activities, assessed as relevant to the individual, need to be examined. These include walking (over a set distance), climbing stairs, sitting to standing, bending, mini squat to full squat, one-leg stand, heel raise and any specific activity known to cause problems. In addition to pain, it is also helpful to look for even weight bearing, balance, co-ordination, symmetry and load transfer (Lee & Lee 2007). Pain is not always reproduced on testing unless the problem area is in the acute stage. This appears to be due to the tendency for pain to be aggravated by sustained postures or repeated activities. If repeating an activity or sustaining a posture does not reproduce pain, the examination must rely on an analysis of the quality and patterns of movement throughout the kinetic chain. Forward spinal bend is useful for assessing the relative contribution of lumbar, thoracic and hip joints into flexion as well as highlighting segmental hinging or translation. Mini squat is helpful in assessing lower limb alignment during a functional activity. One-leg stand assesses the ability to transfer load effectively through the pelvis and hip. Heel raise can be helpful in assessing control around the foot and ankle.
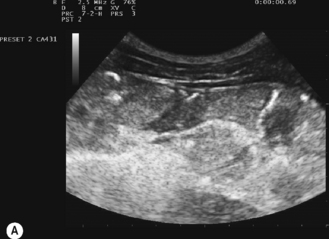
Many hypermobiles suffer from feelings of instability and ‘giving way’, subluxations and dislocations, and due to the lax connective tissue, joints may become unstable through injury. Treatment is therefore focused on control of movement and it is important to assess the local postural muscles associated with trunk stability, such as transversus abdominus, deep multifidus and the pelvic floor muscles in terms of timing, atrophy, loss of tonic function, loss of co-ordination and asymmetry. There is also support for the use of real time ultrasound imaging to assess performance of the deep stability muscles, which can be particularly useful for identifying ‘cues’ which the patient can use to activate the correct muscle (Fig. 9.5).
Proprioception
It is known that proprioceptive acuity is diminished in individuals with JHS (Mallik et al 1994, Hall et al 1995) and this can have a significant effect on the way an individual moves. The research shows that both joint position sense and threshold to detection of movement are impaired such that they have less awareness of approaching the end of joint range (Chapter 6.4). The reason for this impairment is not known but may be related to increased laxity and elasticity in the tissues, which may explain why the application of tape has been found to enhance proprioception in those with a deficit (Callaghan et al 2002, 2008) and also why supportive, tight garments have been reported as helpful in improving proprioceptive feedback (Simmonds & Keer 2007).
In the laboratory, threshold to detection of passive movement has been found to be more reliable than joint position sense (Juul-Kristensen et al 2008), but detection is affected by the position in range of movement when testing (Ageberg et al 2007). In addition, the effect of pain and injury should be taken into consideration as Juul-Kristensen et al (2008) found that proprioception was poorer in elbows with epicondylitis than in the controls’ elbows.