Chapter 10 Physiotherapy and occupational therapy in the hypermobile adolescent
Prevalence
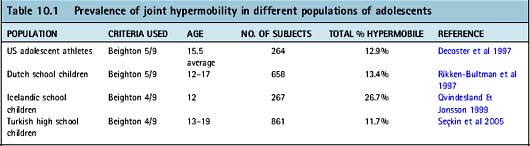
Studies on the prevalence of JHS in children must be viewed with caution because of the variability of diagnostic criteria used. The reported prevalence of JHM in children varies from 6.7% of British school children (Carter & Wilkinson 1964) to 39.6% of Caucasian Brazilian school children (Forleo et al 1993) (Chapter 11). There have been no studies that have specifically investigated the incidence of JHS in adolescents (Table 10.1).
Growth
Growth rates
In early childhood both girls and boys grow at a similar rate in height and weight. The most rapid rate of growth occurs just before birth and it then remains relatively steady until adolescence. The rate of growth is disproportionate throughout the body: until the teenage years the rate of growth is greater in the limbs than the spine, but during adolescence the rate of growth is greater in the trunk. The peak height velocity (adolescent growth spurt) occurs approximately two years after the onset of puberty (Porter 1989). The onset of puberty is approximately 10.5 years of age in girls and 12.5 years in boys. There is a change of body shape and proportion in various body parts during this growth period. On average girls add between 6–11 cm and boys 7–12 cm to their height during this period. Most girls have reached 99% of their adult height by the time they are 15 whereas boys reach adult stature between 18 and 21 years old. Although peak height velocity occurs earlier in girls, boys eventually surpass girls to attain a larger adult stature. By the age of 18, the average boy is 12 cm taller and 10 kg heavier than the average 18-year-old girl (Riddoch 1991).
Co-ordination
There is a perceived ‘adolescent awkwardness’ that accompanies the growth spurt and manifests in poor co-ordination and balance. There is some evidence (Beunen & Malina 1988) that this clumsiness affects one-third of teenage boys, lasts up to 6 months and is probably a result of the disproportionate rate of growth between the trunk and legs.
Flexibility
In adolescence there is often a reduction in flexibility in both those with JHM and those with normal tissues. It has been thought that during the growth spurt, the growth of the bony elements often outstrips that of the soft tissue elements (Thein 1996) and there is a subsequent decrease in strength and flexibility. It is this stage in development that tissues can become overstressed in a cumulative overload, and many adolescents find that their joints are less lax and movements are stiffer. Until the muscles catch up with the increase in bone length they are under a degree of tension that is felt as increased muscle tightness and this may be one of the causes of growing pains in adolescents. In addition, the lumbar fascia may not be able to keep pace with the bony growth spurt during adolescence which can result in increased tension and tethering in the thoracolumbar fascia giving rise to an increased lumbar lordosis. Typical postural changes at this time include:
Some adolescents with JHM will not notice any increase in stiffness, but others will notice a reduction in joint laxity in a range that nevertheless remains hypermobile. As changes occur in the muscles and more sarcomeres (the contractile unit of muscle) are laid down, flexibility may improve again. However, a study of 600 high-school children did not find any correlation between growth and decreased flexibility during the peripubescent period (Feldman et al 1999).
Weight
Weight increases steadily throughout childhood and adolescence. Peak weight velocity follows peak height velocity and is closer to age in boys than girls. In boys the difference between peak height velocity and peak weight velocity ranges from 0.2 to 0.4 years whereas the ratio for girls is 0.3 to 0.9 years (Malina et al 2004). A study measuring pre- and post-puberty weight change showed that boys increase in weight by an average of 113% and girls by an average of 67% (Buckler 1990). This increase in mass (body weight) substantially increases the ground reaction forces to which the joints are subjected, and the more fragile tissues of a child with JHS become vulnerable if joint stability is further compromised by poor muscle control.
Increase in muscle mass and strength are proportional to weight gain during adolescence (Thein 1996). A boy’s muscle mass will double between the ages of 11 and 17 years, and peak height and muscle growth occur simultaneously. A girl’s muscle mass doubles between 9–15 years of age, and the fastest growth is approximately 6 months after peak height velocity. In both sexes increases in muscle strength closely follow increases in muscle mass, which occur approximately 9–12 months after peak height and weight gain (Porter 1989).
Bone
Bone maturation is the process whereby the tissue undergoes changes from the embryonic rudiment of bone to the adult form (Roche 1986). Before puberty chronological age correlates well with bone age but during adolescence bone age is more closely related to adult maturity levels, so that bone age is related to the timing of puberty and growth in height in an individual (Roche 1986). Hence, two adolescents of the same chronological age can have different levels of bone maturation owing to differences in timing of onset of puberty. This can be particularly relevant in teenagers who are playing contact sports (Chapter 13) in teams where the selection criterion is based on age rather than skeletal maturity.
Clinical presentation
The presence of JHM in adolescents, as in other age groups, does not equate to having JHS so that hypermobile individuals do not necessarily develop problems and may even consider the increased flexibility to be an asset (Grahame 2003). Symptoms may arise as a result of hypermobility at any age and JHS is seen more frequently in girls. JHS is a common cause of referral for musculoskeletal symptoms in children and adolescents (Murray & Woo 2001) and one study reported three-quarters of hypermobile subjects had developed symptoms before the age of 15 (Kirk et al 1967). JHS is under-diagnosed and adolescents with the condition are often dismissed as having growing pains or emotional problems (Chapter 2).
Fatigue
Adolescents with JHS may complain of an overwhelming fatigue. In a matched case-control study comparing Beighton joint hypermobility scores (Chapter 1) in 58 consecutive children with chronic fatigue syndrome (CFS) with 58 healthy controls (Barron et al 2002), it was found that there was a higher incidence of JHM in those with CFS than in the control group. Nijs et al (2006) also found that generalized JHM is more common in patients with CFS than in healthy controls (Chapter 6.1).
A study has shown an association between JHM and malnutrition. A cross-sectional field study of 829 children of the lower urban socio-economic strata in Mumbai, aged 3–11 years, found that moderate and severe malnutrition were associated with JHM and that moderately and severely malnourished hypermobile children were more likely to have musculoskeletal symptoms as compared to their non-hypermobile counterparts (Hasija et al 2008).
Common problems in the hypermobile adolescent
Spinal problems
Lumbar spine
Hypermobile subjects are particularly susceptible to low back pain, and the incidence of lumbar disc prolapse, pars interarticularis defects and even spondylolisthesis occurs with increased frequency in hypermobile individuals (Chapter 12.8).
Non-specific low back pain is a common problem in hypermobile adolescents and occurs in the absence of demonstrable radiological change, neurological signs or identifiable back pathology. Studies have shown that there is a relationship between joint laxity and low back pain (Chabot 1962, Hirsch et al 1969, Howes & Isdale 1971, Gedalia et al 1985).
Scoliosis
It is reported that there is a link between adolescent idiopathic scoliosis (AIS) and JHM. A study of a group of 109 Chinese girls with AIS found them to have more joint flexibility than a control group (Binns 1988). Another study set out to compare the influence of physical and sporting activities on AIS (Perrin 2006). It was found that girls with AIS had a higher level of joint laxity than a control group, regardless of whether they were practising gymnasts. The researchers concluded that girls with high joint laxity may be more prone to developing AIS.
Cervical spine
A history of recurrent episodes of acute torticollis is a common finding in adolescent JHS (Chapter 12.7a). This is a painful unilateral condition that develops after minor trauma or an acute respiratory infection (Staheli 2007). It can also manifest on rising in the morning, particularly in teenagers who sleep prone with their head rotated and extended. A sudden uncontrolled movement of the head can cause the neck to become ‘locked or stuck’. Poor control of the deep neck and shoulder girdle stabilizing muscles is a contributing factor, and it has been proposed that overstretching of the neck may cause partial subluxation of the facets, or straining of the muscles and ligaments. A case report in which magnetic resonance imaging (MRI) was performed on a 15-year-old male adolescent within a few hours of onset of an acute torticollis showed there was a signal intensity compatible with a fluid collection at C2–3, and that the lesion was probably linked to a sudden disruption of the disc collagen fibres, thereby causing excessive lateral pressure, pushing C2 to the left; MRI 3 weeks later was unremarkable (Maigne et al 2003).
A study of 564 pre-adolescent children with musculoskeletal pain showed that at 4-year follow-up, neck pain was the most persistent/recurrent musculoskeletal pain and that age, headache, JHM and having combined musculoskeletal pain were found to be independent predictors of pain in adolescence (El-Metwally et al 2004).
Persistent headaches are a feature of JHS in adolescence. Cervical spine JHM has been found to be a possible predisposing factor for new daily persistent headache (Rozen et al 2006).
Peripheral joint problems
The shoulder
The extensible shoulder joint capsule of an adolescent with JHS may allow humeroscapular positions outside the range of balanced stability, and poor neuromuscular control may fail to position the scapula to balance the net humeral joint reaction force. An excessively compliant capsule with relatively weak rotator cuff muscles and poor proprioception will also reduce the stability of the joint. This type of instability is often most prevalent in mid-range positions and simple activities of daily living such as putting on a coat or reaching for an object can cause the shoulder to sublux. See Chapter 12.1 for more detail on shoulder pathology in JHS.
The hip
In hypermobile adolescents a snapping or clicking hip is a common phenomenon. The click may or may not be associated with pain and symptoms (Sanders & Nemeth 1996). The adolescent may complain that it feels as though their hip ‘goes out of joint’ and they may have intermittent difficulty in fully weight-bearing through the hip. Clicking of the hip has also been associated with excessive femoral head translation (in an anterior or posterior direction) that results from poor control of the muscles that stabilize the hip and pelvis (Sahrmann 2002). In particular, these individuals tend to have particularly weak gluteal muscles and iliopsoas. Hip problems associated with JHM are discussed in further detail in Chapter 12.3.