Figure 20.1 A peripheral nerve in short-axis or transverse view: hypoechoic fascicles in a hyperechoic background, often described as “honeycomb” in appearance.
Ultrasound-guided procedure
The selection of an anesthetic agent should be tailored to the specific goals of the PNB. In general, lidocaine provides faster onset times, while bupivacaine and ropivacaine provide longer duration of action. This distinction becomes important when longer durations of anesthesia are preferred, such as with complex lacerations. Situations in which shorter durations of anesthesia are preferred include fractures with a risk of compartment syndrome. There is no evidence to date that any particular anesthetic agent is superior to another in terms of efficacy, or that any significant benefit is gained by mixing different agents together.
First, one must determine the appropriate anesthetic agent and calculate the maximum amount to be used. Ultrasound guidance has allowed providers to deliver lower volumes of anesthetic agent than were classically used with the landmark techniques without sacrificing nerve block quality. For this reason, current dosing recommendations are based upon the maximum safe dose of the agent, and do not reflect the optimal dose for an effective block (Table 20.1). It is important to note that the volume of distribution of anesthetic agents is greater in children than in adults, allowing them to tolerate higher doses on a mg/kg basis without peak plasma levels reaching toxic thresholds. The exception is an infant less than six months of age. In this age group, the volume of distribution is reduced due to lower protein-binding capacity and depressed hepatic metabolism. It is for these reasons that the dose of amide agents should be reduced by 50% in this age group, to safely reduce peak plasma levels and to avoid systemic toxicity.
| Anesthetic agent | Recommended dose (mL/kg) | Onseta | Durationb (h) |
|---|---|---|---|
| Lidocaine 2% | 0.25–0.5 | Fast | 0.75–2 |
| Bupivacaine 0.25% | 0.25–0.5 | Intermediate | 1.5–8 |
| Ropivacaine 0.2% | 0.25–0.5 | Intermediate | 1.5–8 |
Next, the appropriate needles should be chosen. A small-bore needle such as a 27- or 30-gauge needle is generally used for a pediatric PNB. The needle length is dependent upon the depth of the optimal injection site, and should be measured during sonographic nerve identification. A small needle size decreases patient pain during skin puncture and limits the injection rate, both of which are major sources of patient discomfort. However, a smaller needle size can affect the ease of needle visualization by ultrasound. A smaller needle can be challenging to maintain in plane, requiring both very subtle hand movements and a high degree of hand–eye coordination. One may also use injection syringes or similar syringe attachments, which may aid in needle control.
Then, the operator should determine the path for the needle that best avoids surrounding structures. The needle is then inserted using the long-axis, or in-plane, approach (Figure 20.2a) in order to maximize the visualization of the needle and its tip. The needle will appear longitudinally on the screen in this orientation, as it travels under the transducer (Figure 20.2b). Real-time ultrasound visualization of the needle tip is essential during the entire procedure, in order to eliminate the possibility of accidental puncture of surrounding vascular structures. The needle tip location can be confirmed by injecting small amounts of anesthetic agent as the needle is advanced. This is called the “step down” approach, in which hypoechoic spread should occur at the needle tip. Failure to visualize this phenomenon indicates that the needle tip is out of plane and must be found and redirected, prior to further needle advancement or injection at the target nerve.
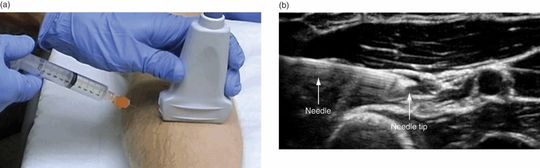
Figure 20.2 The in-plane or long-axis approach to peripheral nerve blocks. (a) The preferred needle orientation is shown in plane with the transducer. (b) The needle appears longitudinally on the screen. Courtesy of William Soares, MD.
Occasionally, a short-axis, or out-of-plane, approach is necessary when performing a PNB on small infants (Figure 20.3). The needle may be too short to reach the target nerve from the edge of the transducer using the in-plane approach, depending upon the size of the transducer, the needle, and the patient. Care should be taken using the short-axis, or out-of-plane, approach in this circumstance, as it is much more challenging to correctly identify the needle tip, which appears as a hyperechoic or bright dot. The “step down” approach is often helpful in identifying the needle tip in the short-axis.
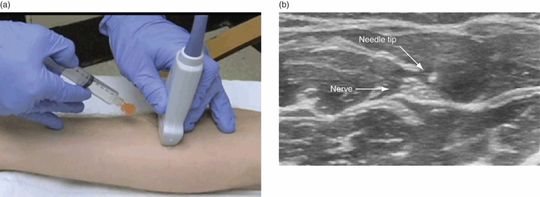
Figure 20.3 The out-of-plane or short-axis needle orientation. (a) Needle orientation is shown out-of-plane with the transducer. (b) The needle appears as a hyperechoic or bright dot on ultrasound.
Finally, it is critical at the time of injection to precisely deliver the anesthetic agent circumferentially around the entire target nerve for optimal efficacy. Ideally, the target nerve will float or bathe in the hypoechoic anesthesia, making the nerve’s hyperechoic structure more prominent and distinct (Figure 20.4). The syringe plunger should always be drawn back prior to any injection, to avoid intravascular injection.
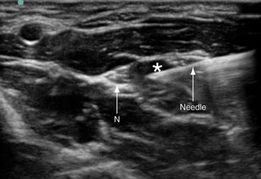
Figure 20.4 Injection of anesthetic agent circumferentially around a target nerve. Anesthetic agent is shown being delivered at the median nerve (N). The anesthetic agent appears hypoechoic or dark (*) on the ultrasound screen. Ideally, anesthetic agent will surround the target nerve at completion of the procedure. Courtesy of William Soares, MD.
Training and education
The ability to successfully execute a PNB using ultrasound guidance requires that the provider be trained both to identify the target nerve, and to deliver the anesthetic agent accurately and safely. It is strongly advised that appropriate training should be sought for both aspects of the procedure on phantom models, prior to performing in the clinical setting. Special attention should be given to the physical act of needle insertion and injection while in plane with the ultrasound transducer, using a single hand (the single-operator method). The quantity and quality of training to ensure overall procedural competence and proficiency remains unclear.
Specific scanning techniques
Forearm nerve block
Anatomy
It is important to become familiar with the anatomy of the forearm (Figure 20.5). Vascular structures run throughout the forearm, and are located close to the radial and ulnar nerves within their neurovascular bundles. These arteries and veins must be identified, in order to avoid unnecessary puncture and associated complications.
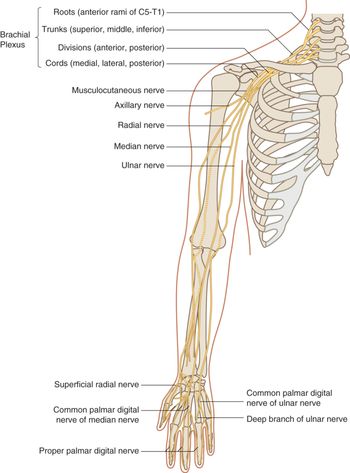
Figure 20.5 Anatomy of the forearm. It is important to be familiar with the radial nerve, the ulnar nerve, and the median nerve, and their associated neurovascular bundles. Artwork created by Emily Evans © Cambridge University Press.
The innervation of the hand must be conceptualized in three dimensions. Three nerves innervate the hand: the median nerve, the ulnar nerve, and the radial nerve. The selection of these nerves for blockade is dependent upon the location within the hand that the provider intends to anesthetize (Figure 20.6). For example, a deep palmar laceration may require a radial nerve blockade and a median nerve blockade, in order to guarantee the complete anesthesia of all deep structures. The routine blockade of all three nerves ensures a successful outcome, regardless of anatomical variation of the nerves and their innervation within the hand.
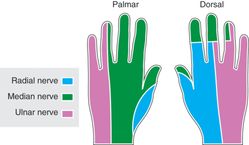
Figure 20.6 The nerve innervation of the hand. Shown is the median, radial, and ulnar nerve distribution of the hand. Artwork created by Emily Evans © Cambridge University Press.
Technique
In order to sonographically identify the three target nerves in the forearm, a systemic approach is utilized. The transducer is placed at the distal forearm and moved proximally to the mid-forearm (Figure 20.7). Once the nerve is identified, the transducer should be firmly anchored. Even subtle movement of the transducer may result in the loss of needle visualization and prolonged time to complete the procedure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








