Perioperative Management of Patients and Equipment Selection for Neural Blockade
James C. Crews
Vincent W. S. Chan
The essential elements for optimal perioperative management of patients for neural blockade include a physician, well-trained in the principles and techniques of regional anesthesia, working in a well-equipped, well-staffed anesthetizing location designed for safe and efficient patient care. The anesthesiologist must be skilled, not only in the technical aspects of how to accomplish a selected neural blockade technique, but also in its indications and contraindications, as well as appropriate intraoperative patient management. Ideally, these skills and knowledge are taught beginning early in the anesthesia training period by experts in the subspecialty. From this beginning, the anesthesiologist who has a sincere interest in neural blockade, and who is convinced of its efficacy, will continue to apply and refine her technical skills until they become an essential part of the anesthetic armamentarium.
A thorough knowledge of the pertinent anatomy, obtained from textbooks and atlases, should be reinforced through the study of cadavers and surgical specimens. In addition, one should be familiar with the physiology of neural blockade, the pharmacology of the local anesthetic agents themselves, and the physiologic effects and potential complications associated with the various regional anesthetic techniques. One can, therefore, anticipate changes in the patient’s status and not only determine the suitability of a given technique for a specific patient and procedure, but also be prepared to institute appropriate therapy if and when these changes occur.
Finally, this thorough knowledge of the requirements for successful neural blockade also requires that the anesthesiologist undertake these activities in a location well equipped with not only suitable neural blockade equipment, but also with all other appropriate monitors, resuscitation drugs, and equipment. This equipment should be located in such a way as to allow easy access to commonly used monitors and supplies, and allow ample room for the patient, the anesthesiologist, and an assistant. The anesthesiologist and the assistant must have ample room to move about without feeling confined. The area should also allow the patient adequate privacy from other nearby patients or visitors.
Patient Selection
The most important determinant in the selection of a regional anesthetic technique is the suitability of that technique to that specific patient for that specific procedure. Unless thorough and careful consideration is given to the patient, all else will likely fail. Specific patient factors to be considered include the patient’s anatomy, coexisting medical conditions, and neuropsychological state.
Because nearly all regional anesthetic techniques are based on the identification and utilization of anatomic landmarks, both surface and bony, it is useful that the patient display those landmarks to a sufficient degree. Examples of anatomic impediments to the conduct of a successful neural blockade technique include morbid obesity, arthritis, and other physical deformities that would limit patient positioning or palpation of local landmarks at the site of the block. The use of ultrasound imaging may be helpful in some situations in which anatomic surface landmarks are difficult to determine.
Complicating coexisting medical conditions may be either local or systemic. Local conditions such as infection, anatomic abnormalities, trauma, burns, or dressings could all preclude the opportunity to perform a satisfactory block technique. More subtle, and often more important, are the systemic problems of the patient. Clearly, a severely hypovolemic patient should not be considered for a technique that involves major sympathetic neural blockade unless appropriate fluid resuscitation is accomplished beforehand. Patients with neurologic disease, coagulopathies, or severe cardiovascular disease require a thorough preanesthetic medical and laboratory evaluation of their pathology. In some circumstances, one type of block technique will be contraindicated whereas another might be perfectly acceptable. It must be remembered that the anesthetic choice involves not only the selection of a block technique but also consideration of the risks and benefits of all anesthetic options tailored to the individual patient for the best possible outcome. Coincident with the assessment of the patient’s pathophysiology is the consideration of the patient’s
preoperative medications. Special management considerations may be required for some neural blockade techniques in patients receiving antihypertensive agents, β-adrenergic receptor blockers, anticoagulant medications, antiplatelet agents, or high-dose opioid analgesics. The use of certain neural blockade techniques for patients with various preexisting medical conditions (e.g., patients with coagulopathies or history of anticoagulant/antiplatelet therapy, patients with preexisting neurologic disease or deficits, and patients with localized or systemic infections) is a controversial and highly subjective issue. The literature does not contain absolute documentation of when it is safe or unsafe, indicated or contraindicated, preferable or optional to apply a given anesthetic technique or agent. The decision is multifactorial but ultimately becomes the responsibility of the attending anesthesiologist (1). The risks versus benefit of any given technique must be viewed in the context of the individual patient.
preoperative medications. Special management considerations may be required for some neural blockade techniques in patients receiving antihypertensive agents, β-adrenergic receptor blockers, anticoagulant medications, antiplatelet agents, or high-dose opioid analgesics. The use of certain neural blockade techniques for patients with various preexisting medical conditions (e.g., patients with coagulopathies or history of anticoagulant/antiplatelet therapy, patients with preexisting neurologic disease or deficits, and patients with localized or systemic infections) is a controversial and highly subjective issue. The literature does not contain absolute documentation of when it is safe or unsafe, indicated or contraindicated, preferable or optional to apply a given anesthetic technique or agent. The decision is multifactorial but ultimately becomes the responsibility of the attending anesthesiologist (1). The risks versus benefit of any given technique must be viewed in the context of the individual patient.
Finally, the patient’s attitude or preconceptions regarding regional anesthesia may play a role in determining patient acceptance of a specific neural blockade technique. For example, an individual patient may accept a peripheral nerve block for open fixation of an ankle fracture yet might be completely opposed to consideration of a spinal anesthetic for the same procedure. A study by Matthey in 2004 demonstrated that the general public is not very well informed about the matters related to regional anesthesia, and that people’s fears and conceptions about regional anesthesia are greatly distorted (2). Preoperative discussion of reasonable anesthetic options for a surgical procedure may require some degree of patient education regarding regional anesthesia versus general anesthesia or the selection of an individual block technique. Tetzlaff and colleagues found in patients undergoing reconstructive shoulder surgery that interscalene block was found to be highly acceptable to those who had undergone previous shoulder surgery with general anesthesia. These authors supported the belief that the key to patient acceptance of regional anesthesia involves patient education and preparation (3).
The anesthesiologist must also undertake all the other common elements of a preanesthetic evaluation, including a complete history and physical examination. The usual elements of systemic disease, current medications, past operations and anesthetics, allergies, airway and dentition, and family history of anesthetic problems must be recorded. Laboratory studies essential for the conduct of a general anesthetic must also be recorded. Patients must first be evaluated as candidates for general anesthesia and then evaluated for suitability for regional anesthesia.
Patient Interview
Once the anesthesiologist has determined an anesthetic plan, it is discussed with the patient and informed consent is obtained. A broad but useful definition of informed consent is the obligation to explain to the patient the risks and benefits of the selected anesthetic plan, as opposed to the risks and benefits of an alternate plan. A significant number of patients refuse a regional anesthetic because “they don’t want to be awake during the operation.” It is essential, therefore, that the anesthesiologist describe in chronological detail the events that will occur from arrival in the surgical/anesthesia area through admission to the recovery area. Patients should be assured that as soon as an intravenous (IV) infusion is established, systemic sedatives will be given to make the patient comfortable prior to the anesthetic. Patients also need to be told, early in the interview, that they will be provided with additional systemic drugs throughout the operation to produce a state of sedation (with possible progression to general anesthesia) as needed for their comfort. When available, the use of headphones with music, visual screens, and other distracting techniques should be discussed.
The anesthesiologist should describe in detail the performance of the block and the patient’s role in that process. This description should include the need for starting of an IV infusion, and the requirement for patient positioning. The neural blockade procedure should be described, including the possibility of producing paresthesias, neuromuscular stimulation, or the use of ultrasound guidance, as well as the signs and symptoms of normal onset of neural blockade, and the possibility of systemic effects and adverse events.
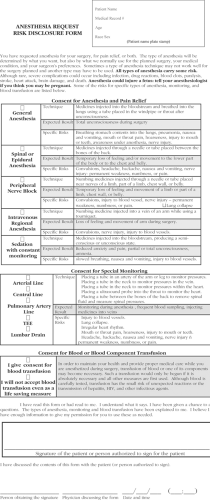
Informing the patient about the rationale for neural blockade will further motivate patients toward acceptance. Factors such as a reduced likelihood of side effects from inhalational general anesthetics, muscle relaxants, and endotracheal intubation should be noted. The increased public awareness of postoperative pain relief facilitates patient acceptance of regional anesthesia. The painless emergence from operative sedation in the recovery unit with a plan for earlier discharge with fewer risks of inhaled anesthetic- or opioid analgesic-related side effects, and the possibility of extending neural blockade into the postoperative period with continuous catheter techniques should also be discussed. The amount of information given will vary for each patient; however, such discussions invariably increase the confidence of the patient and may positively affect the recovery. Figure 8-1 shows an informed consent document developed at Wake Forest University that outlines the risks of various selected regional anesthesia and general anesthesia techniques separately to allow the patient a clearer understanding of the risks associated with individual procedures and techniques.
Premedication of Patients for Neural Blockade Technique
Just as the principles applied to preoperative preparation of a patient for a regional anesthetic technique are primarily those used for general anesthesia, so too are the basic tenets similar in the administration of the preanesthetic medications.
Preanesthetic Fasting
In the past, all patients scheduled to receive any type of anesthetic were restricted from all oral intake for a minimum of 6 hours and preferably from midnight the day before surgery. The efficacy of this practice was reexamined in the early 1990s. Because unconsciousness may be a required or desired part of any surgical procedure performed with a regional anesthetic, the rationale for preanesthetic fasting should be the same as that for a surgical procedure performed with a general anesthetic. There are many individual circumstances, especially in pediatric procedures, where these practices will be modified, but some general guidelines are helpful.
Phillips et al. (4) prospectively compared the effect of allowing unrestricted clear fluids until the time of oral medication (2 hours prior to surgery). Patients otherwise underwent conventional fasting. The residual volume and pH of gastric contents after induction of anesthesia were measured in 100 elective surgical patients allocated randomly to a group
allowed unrestricted fluids or to a control group who fasted for 6 hours (mean = 388 mL versus 0 mL). There was no significant difference in mean residual gastric volume (22 mL versus 19 mL) or pH (2.64 versus 2.26) between the study group and the control group. Problems with aspiration were not encountered. The authors concluded that elective surgical patients could be allowed to drink clear fluids until 2 hours before anesthesia to enhance patient comfort without compromising safety. An accompanying editorial in the British Journal of Anaesthesia (5) also stated: “Returning to elective operations which concern the vast majority of patients requiring an anaesthetic, it is clear that ‘nil by mouth after midnight’ should be abandoned. In its place, there should be agreement by anesthetists, surgeons, and nurses on guidelines that both day-case and inpatients may take, if they wish, clear fluids by mouth up to 3 hours before surgery.” The list of clear fluids excluded alcoholic drinks and those containing milk or sugar but it did include orange juice and apple juice.
allowed unrestricted fluids or to a control group who fasted for 6 hours (mean = 388 mL versus 0 mL). There was no significant difference in mean residual gastric volume (22 mL versus 19 mL) or pH (2.64 versus 2.26) between the study group and the control group. Problems with aspiration were not encountered. The authors concluded that elective surgical patients could be allowed to drink clear fluids until 2 hours before anesthesia to enhance patient comfort without compromising safety. An accompanying editorial in the British Journal of Anaesthesia (5) also stated: “Returning to elective operations which concern the vast majority of patients requiring an anaesthetic, it is clear that ‘nil by mouth after midnight’ should be abandoned. In its place, there should be agreement by anesthetists, surgeons, and nurses on guidelines that both day-case and inpatients may take, if they wish, clear fluids by mouth up to 3 hours before surgery.” The list of clear fluids excluded alcoholic drinks and those containing milk or sugar but it did include orange juice and apple juice.
In 2002, the American Society of Anesthesiologists released its Practice Guidelines for Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration: Application to Healthy Patients Undergoing Elective
Procedures (6), and made the following recommendations for preanesthesia fasting:
Procedures (6), and made the following recommendations for preanesthesia fasting:
It is appropriate to fast from intake of clear liquids for 2 or more hours before procedures involving general anesthesia, regional anesthesia, or sedation/analgesia. … Examples of clear liquids include but are not limited to water, fruit juices without pulp, carbonated beverages, clear tea, and black coffee.
These guidelines are not intended to include patients with coexisting diseases or conditions that might affect gastric emptying or fluid volume (e.g., pregnancy, obesity, diabetes, hiatal hernia, gastroesophageal reflux disease, ileus or bowel obstruction, emergency care, or enteral tube feeding) or patients in whom airway management might be difficult. In urgent, emergent, or other situations in which gastric emptying is impaired, the fasting status of the patient and the risk potential for pulmonary aspiration of gastric contents must be considered in determining the timing of the intervention and the degree of sedation/analgesia.
Preanesthetic Medications
The advent of ambulatory surgery and the current practice that most patients are seen for the first time by their anesthesiologist a few hours before surgery has changed the rationale and types of drugs used for premedication. Even the former practice of writing preanesthetic medication orders for inpatients “on-call to the OR” has generally been abandoned in favor of receiving unmedicated patients into the preanesthesia holding area and then providing preanesthetic sedation after a final opportunity for discussing the anesthetic and answering patient’s questions immediately prior to the surgical procedure.
Timing of Administration
Premedication has as its goals the rapid onset of anxiolysis, amnesia, and analgesia with a relatively short duration of action. It is essential that all preanesthetic and presurgical discussions and consents be obtained and documented prior to
administration of any premedication. Not infrequently, changes in the surgical or anesthetic plan may be required for a variety of reasons. Patients may fail to arrive on time for the procedure, they may have eaten prior to arrival, they may have previously unknown (or missing) abnormal laboratory values, electrocardiogram (ECG) changes, or chest radiographic results, there may have been an interim illness since the last office visit requiring reevaluation with the potential for surgical postponement or cancellation. Thus, the anesthesiologist must be sure that a scheduled procedure will take place, and that the surgeon and patient have had an opportunity to resolve all relevant issues that may require an addition, deletion, or revision of the surgical consent before administering sedative premedications to the patient.
administration of any premedication. Not infrequently, changes in the surgical or anesthetic plan may be required for a variety of reasons. Patients may fail to arrive on time for the procedure, they may have eaten prior to arrival, they may have previously unknown (or missing) abnormal laboratory values, electrocardiogram (ECG) changes, or chest radiographic results, there may have been an interim illness since the last office visit requiring reevaluation with the potential for surgical postponement or cancellation. Thus, the anesthesiologist must be sure that a scheduled procedure will take place, and that the surgeon and patient have had an opportunity to resolve all relevant issues that may require an addition, deletion, or revision of the surgical consent before administering sedative premedications to the patient.
Table 8-1 Observer’s Assessment of Alertness/Sedation (OAA/S) scale | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||
Before administration of sedatives or analgesics, it should be verified and confirmed that the patient is the correct patient, for the correct procedure, to be performed on the correct side of the body, and that these parameters are clearly outlined in the patient’s consent for surgery and anesthesia. This interaction may occur as a “time-out” session, during which these issues are verified by the patient and confirmed by a member of the anesthesia or surgical team and a witness. After this confirmation of correct patient and procedure, and attention to any last-minute patient question’s or concerns, the anesthesiologist may proceed with premedication and positioning of the patient for the neural blockade procedure.
Monitoring During Sedation
Any time supplemental IV agents are being used, it is especially important that the anesthesiologist have an assistant to monitor the patient’s vital signs and level of consciousness and ensure maintenance of proper patient positioning for the procedure. Minimum monitoring standards for patients undergoing neural blockade procedures should include pulse oximetry monitoring of pulse rate and oxygen saturation (7). ECG and blood pressure should monitored or monitoring equipment should be immediately available. For patients receiving supplemental sedative-hypnotic or opioid analgesic drugs, supplemental oxygen administration should be considered, and supplemental oxygen administration is recommended for all patients receiving moderate or deeper levels of sedation, or for patients receiving combinations of drugs or dose titrations (Table 8-1). Following the administration of supplemental sedative or analgesic drugs or performance of the neural blockade procedure, the patient should be intermittently monitored and should not be left alone until adequate recovery of consciousness and respiratory function has been established. Regular verbal contact should be maintained to ensure consciousness and comfort until the patient has recovered from the effects and the potential side effects of all drugs administered and until delayed systemic toxicity from the local anesthetics is ruled out.
Selection of Sedative/Analgesic Medications
The goal of the anesthesiologist is to provide the patient with a pleasant anesthetic experience throughout the entire perioperative period. The amount of additional supplemental sedative or analgesic medication required for the nerve block procedure depends not only on the specific requirements of the patient, but also on the degree of painful stimulation associated with the performance of the selected block technique. Most patients require little additional supplementation for the simple, single-injection procedures such as spinal, epidural, and axillary block. In fact, patients often are more easily positioned and responsive to paresthesias or nerve stimulation if they are not heavily medicated. Conversely, procedures such as deep paravertebral blocks (psoas compartment, celiac plexus, and sympathetic blocks) or multiple intercostal nerve blocks are quite painful and will likely require additional parenteral sedation and/or analgesics. Nervous or hypersensitive patients may also benefit from additional parenteral supplementation.
As discussed earlier, the selection of sedative or analgesic drugs for administration prior to and during performance of a neural blockade procedure is as individual as the choice of premedication. The common goal, however, is to produce adequate sedation, analgesia, and anxiolysis while maintaining meaningful contact with the patient throughout the procedure. If deeper levels of sedation are required for brief periods during the procedure, very short-acting medications that will allow a rapid return of consciousness are preferable. Excessive sedation
incurs the risks of airway obstruction or circulatory collapse and will also mask the early warnings of complications of the block, such as an unintentional high spinal or epidural block, a painful intraneural injection, or an intravascular injection. Excessive doses of some of the psychotropic or dissociative drugs may also render a previously cooperative patient excitable or unmanageable. Short-acting IV drugs given in small doses or by a continuous infusion can be carefully titrated to produce the desired level of sedation and analgesia and still ensure a rapid recovery at the conclusion of the block.
incurs the risks of airway obstruction or circulatory collapse and will also mask the early warnings of complications of the block, such as an unintentional high spinal or epidural block, a painful intraneural injection, or an intravascular injection. Excessive doses of some of the psychotropic or dissociative drugs may also render a previously cooperative patient excitable or unmanageable. Short-acting IV drugs given in small doses or by a continuous infusion can be carefully titrated to produce the desired level of sedation and analgesia and still ensure a rapid recovery at the conclusion of the block.
Anticholinergics
Most practitioners of regional anesthesia have abandoned the routine use of anticholinergic drugs unless they plan to combine their technique with an inhalation anesthetic. Those abandoning the preoperative use of these drugs considered their action as primarily antisialagogue. Anticholinergic drugs in adult, premedication doses do not alter gastric fluid pH or volume (8). A published review of postoperative nausea and vomiting states that “the incidence of nausea and vomiting during spinal anesthesia is decreased by the intravenous administration of atropine.” However, the quoted references date to the late 1950s and raise the question of whether such conclusions are still valid (9).
In summary, the preanesthetic use of this class of drugs is limited to a knowledge of their various clinical actions and the application of that action to the specific needs of a select patient. Routine use of anticholinergics as premedications for regional anesthesia is not recommended.
Antiemetics
One of the inducements anesthesiologists offer to patients when comparing regional and general anesthesia is the reduced likelihood of postoperative nausea and/or vomiting (PONV) with regional anesthesia, especially as compared to general anesthesia using volatile anesthetic agents. Postoperative nausea and vomiting remains as a significant perioperative occurrence despite recent advances and treatment. Patients generally consider PONV to be among the most undesirable perioperative anesthesia-related concerns (10). PONV continues to be among the most common factors delaying inpatient discharge from the post anesthesia care unit (PACU), outpatient discharge to home, and unanticipated hospital admission for ambulatory surgery patients (11). Volatile anesthetics, nitrous oxide, large-dose neostigmine, and intra- or postoperative opioids are well established anesthesia-related risk factors for PONV (12), and regional anesthesia techniques generally avoid or minimize the exposure of the patient to these agents. Although some randomized, controlled clinical studies have confirmed that general anesthesia may cause a greater frequency or severity of PONV than regional anesthetic techniques, the results are far from conclusive (13,14,15,16). Although regional anesthesia may be considered as an attractive alternative to general anesthesia, the confusion arises from the practice of using concomitant IV sedatives and opioids during regional anesthesia to provide anxiolysis and analgesia. Thus, it is difficult to separate the emetic effects of the sedative/analgesic medications from those associated with neural blockade.
The incidence of emesis associated with central neuraxial block is greater than with peripheral nerve block because of the side effects of the resultant sympathetic nervous system blockade (i.e., hypotension and perhaps central hypoxemia). Studies of the actual benefit of central neuraxial block in reducing emesis are conflicting. Even studies with local anesthesia and monitored anesthesia care fail to document conclusively that neural blockade is better. Clearly, the multifactorial causes of perioperative nausea and vomiting are influenced more by total patient management than by the use of any single drug or technique. Reviews of PONV confirm this point (12,17). Therefore, for patients undergoing surgical procedures with regional anesthesia, as for those with general anesthesia, routine prophylactic treatment of PONV with antiemetic agents such as ondansetron, droperidol, dexamethasone, or promethazine should be limited to at-risk patients. With respect to reducing the risk for PONV in patients undergoing surgical procedures with regional anesthesia, attention to maintenance of adequate hydration, administration of supplemental oxygen, and judicious use of oral or IV analgesic adjuvants while minimizing perioperative opioid exposure may be the best strategies to allow the benefits of regional anesthesia to be most clearly demonstrated.
Analgesics
A popular belief among many anesthesiologists is that induction of anesthesia is not painful and thus does not require administration of an analgesic agent in the preanesthetic period. However, practitioners of regional anesthesia or other potentially painful invasive procedures should give strong consideration to their use. Furthermore, the regional anesthetic renders only portions of the patient’s anatomy analgesic. An analgesic will enhance total body comfort and likely reduce the dosage of supplementary sedation.
Two major determinants for the inclusion of an opioid preanesthetic are the type of nerve block and the mental attitude of the patient. Nerve blocks that require paresthesias or multiple insertions, especially paravertebral, are painful and analgesia is beneficial. Similarly, the more apprehensive or excitable the patient, the greater the need for both analgesia and sedation. Excitable patients heavily medicated with sedatives may tend to be drowsy and relaxed until painfully stimulated, when they are likely to overreact or react inappropriately and uncooperatively during an invasive procedure.
Selection of a specific opioid as a preanesthetic analgesic must be made with a consideration of the patient’s analgesic requirements during the ensuing procedure and recovery period. For a brief period of painful stimulus associated with positioning or placement of a nerve block, a short-acting opioid with a fast onset is best. Fentanyl is probably the preanesthetic opioid of choice for analgesia during nerve block procedures because its analgesic effects at 50- to 150-μg doses produce few side effects and provide a cooperative patient with a relatively clear sensorium.
Sedatives
Early practitioners of regional anesthesia combined short-acting barbiturates with opioids as their premedication of choice. Usually, atropine or scopolamine accompanied that combination. As noted earlier, most anesthesia practices today are for same-day patients, many of whom will leave the hospital or surgical facility 1 to 3 hours after their procedure. In addition to the desirable analgesia prior to regional anesthesia, most patients prefer to be sedated and usually amnestic during presurgical procedures. Just as the selection of an analgesic considers the needs and duration of the procedure, so too does the selection of a sedative. The chosen drug may be continued into the operative management of the patient as well.
The benzodiazepines, principally midazolam, are commonly used as sedative agents because of their wide spectrum of central nervous system (CNS) depressant activity, low incidence of side effects, and wide margin of safety. All
benzodiazepines possess the same properties of anxiolysis, amnesia, and sedation to varying degrees. A secondary benefit of using benzodiazepines as premedication for regional anesthesia techniques is their anticonvulsant properties. De Jong (18) first reported the superiority of diazepam over barbiturates in preventing seizures from local anesthesia overdose in animals. As a result of those studies, diazepam enjoyed widespread use as a prophylactic against local anesthetic seizures as well as for its sedative properties. A serious criticism must be given, however, against the use of benzodiazepines as a prophylactic to permit the use of larger than recommended safe doses of local anesthetic. Many factors contribute to a given patient’s toxicity threshold to local anesthetics. It is important, therefore, that the selected dose of a local anesthetic be at or below that recommended dose. Currently, midazolam is the most frequently used benzodiazepine for preanesthetic sedation. Because it is water-soluble, it causes significantly less pain on injection than diazepam (19). Midazolam has a rapid onset of action and a short elimination half-life (2–4 hours) and is significantly more potent than diazepam. Refer to Table 8-2 for commonly used sedative agents and dose recommendations. The other benzodiazepines, lorazepam and oxazepam, are potent amnestic agents but have such a prolonged duration of action that they are less suitable as premedication or supplements to most regional anesthesia procedures (20,21).
benzodiazepines possess the same properties of anxiolysis, amnesia, and sedation to varying degrees. A secondary benefit of using benzodiazepines as premedication for regional anesthesia techniques is their anticonvulsant properties. De Jong (18) first reported the superiority of diazepam over barbiturates in preventing seizures from local anesthesia overdose in animals. As a result of those studies, diazepam enjoyed widespread use as a prophylactic against local anesthetic seizures as well as for its sedative properties. A serious criticism must be given, however, against the use of benzodiazepines as a prophylactic to permit the use of larger than recommended safe doses of local anesthetic. Many factors contribute to a given patient’s toxicity threshold to local anesthetics. It is important, therefore, that the selected dose of a local anesthetic be at or below that recommended dose. Currently, midazolam is the most frequently used benzodiazepine for preanesthetic sedation. Because it is water-soluble, it causes significantly less pain on injection than diazepam (19). Midazolam has a rapid onset of action and a short elimination half-life (2–4 hours) and is significantly more potent than diazepam. Refer to Table 8-2 for commonly used sedative agents and dose recommendations. The other benzodiazepines, lorazepam and oxazepam, are potent amnestic agents but have such a prolonged duration of action that they are less suitable as premedication or supplements to most regional anesthesia procedures (20,21).
Table 8-2 Commonly used IV and inhalation sedative and analgesic drugs and doses recommendations | |||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||
Other drugs have been used as preanesthetic adjuvants prior to administration of regional anesthesia. The tranquilizing drugs (phenothiazines and butyrophenones) were popular earlier, but their hypotensive effects in conjunction with sympathetic blocks resulting from regional anesthesia led to some major complications. The perceived advantage of the butyrophenones is their ability to produce a state of mental calm and indifference with little hypnotic effect. It was discovered, however, that larger doses, especially without analgesic or sedative drugs already present, could produce hallucinations, restlessness, and even extrapyramidal dyskinesia (22). Droperidol is still useful, however, in low doses (0.625 mg), as a potent antiemetic. Excess sedation and delayed discharge time are likely only after doses of droperidol greater than 2.5 mg (23).
Although not truly in the category of preanesthetic medication, the need for a rapid-acting sedative or analgesic to alleviate the anxiety or pain during the positioning for or the performance of a regional block technique can be effectively met with thiopental, methohexital, propofol, or ketamine. (These agents are discussed later in this chapter.) During a regional blockade procedure, small IV bolus doses may be given with close monitoring of the patient’s airway, vital signs, and level of consciousness. The advantage of the use of low doses of these drugs is the rapid recovery of sensorium soon after the block technique is completed. This allows for accurate patient response to onset and level of sensory and motor blockade. The disadvantage of using these drugs lies primarily in their extreme potency and potential for relative overdose, resulting in significant respiratory depression (or apnea) that may require ventilatory support. It must be kept in mind that neither the barbiturates or propofol are analgesic, and may perhaps be even hyperalgesic, so supplemental analgesia may be required with opioid analgesics if these drugs are used for producing brief, moderate or deep levels of sedation.
For patients with painful medical conditions or associated injuries requiring extensive repositioning for an indicated neural blockade procedure, IV ketamine titrated in small, intermittent doses should be considered as an additional adjuvant to the benzodiazepines and opioids. It is our practice for patients in whom we are anticipating significant discomfort associated with positioning for neural blockade (e.g., patient’s with multiple extremity fractures, rib fractures, burn injury, etc.) to titrate doses of midazolam 2 to 3 mg and fentanyl 100 to 200 μg, followed by small IV doses of ketamine (10–20 mg, in 5- to 10-mg increments) to a level of sedation and analgesia that allows positioning without pain.
Perioperative Adjuvant Analgesics
In addition to the administration of sedatives and analgesics to provide sedation, anxiolysis, and analgesia for the performance of neural blockade techniques, it is common to administer adjuvant analgesic agents in the preoperative period to help
manage pain in the intra- and postoperative period. Commonly administered adjuvant analgesics include acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), cyclo-oxygenase inhibitors (COXIBs), and, more recently, gabapentin. Acetaminophen, NSAIDs (such as ibuprofen, naproxen, or ketorolac), and COXIBs (such as celecoxib), with administration starting preoperatively or immediately postoperatively and continued during the postoperative period, have demonstrated a 15% to 55% reduction in postoperative opioid requirement (24,25,26). Meta-analysis of clinical trials with the use of perioperative NSAID administration have also demonstrated significant reductions in opioid-related side effects such as nausea, vomiting, and sedation (26). Recent studies have demonstrated that gabapentin in preoperative oral doses of 600 to 1,200 mg can improve analgesia and reduce postoperative opioid requirement as well (27,28). Although the use of local anesthetics in neural blockade for infiltration, peripheral nerve block, or neuraxial block remains the most potent of the nonopioid analgesic techniques, these other nonopioid analgesics are important adjuvants in the multimodal approach to postoperative pain management. A more thorough discussion of multimodal analgesia in postoperative pain management can be found in Chapter 43.
manage pain in the intra- and postoperative period. Commonly administered adjuvant analgesics include acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs), cyclo-oxygenase inhibitors (COXIBs), and, more recently, gabapentin. Acetaminophen, NSAIDs (such as ibuprofen, naproxen, or ketorolac), and COXIBs (such as celecoxib), with administration starting preoperatively or immediately postoperatively and continued during the postoperative period, have demonstrated a 15% to 55% reduction in postoperative opioid requirement (24,25,26). Meta-analysis of clinical trials with the use of perioperative NSAID administration have also demonstrated significant reductions in opioid-related side effects such as nausea, vomiting, and sedation (26). Recent studies have demonstrated that gabapentin in preoperative oral doses of 600 to 1,200 mg can improve analgesia and reduce postoperative opioid requirement as well (27,28). Although the use of local anesthetics in neural blockade for infiltration, peripheral nerve block, or neuraxial block remains the most potent of the nonopioid analgesic techniques, these other nonopioid analgesics are important adjuvants in the multimodal approach to postoperative pain management. A more thorough discussion of multimodal analgesia in postoperative pain management can be found in Chapter 43.
Equipment, Supplies, Location, and Patient Positioning
Equipment and Supplies
Prior to performing any neural blockade procedure, the anesthesiologist should locate and ensure the proper functioning of the necessary monitoring and resuscitation equipment and drugs. Minimal basic resuscitation drugs and equipment for airway management (airways, suction equipment, laryngoscope, endotracheal tubes, muscle relaxants), support of cardiorespiratory function (oxygen, mask and reservoir bag, epinephrine, anticholinergic drugs, inotropic and/or vasopressor drugs), and sedative/induction agents (benzodiazepines, barbiturates) should be immediately available in case of adverse patient reaction associated with the procedure or the anesthetic agents administered. The Regional Anesthesia Section at Wake Forest University have developed a special “Local Anesthetic Toxicity” box, with special equipment and supplies to treat patients in the event of an unintentional intravascular injection of local anesthetic, in addition to routine resuscitation drugs and equipment.
Monitoring should include, at a minimum, the application of a pulse oximeter to monitor pulse rate, peripheral perfusion, and oxygen saturation (7). For all but the least invasive, least complicated procedures, one should consider electrocardiograph and blood pressure monitoring as well. Peripheral temperature monitoring may be helpful if monitoring for effects of sympathetic blockade.
Location
The location most appropriate for performance of neural blockade procedures will vary according to the type of procedure and practice setting. Local anesthetic infiltration and minor neural blockade procedures may be safely performed in outpatient locations such as physicians’ offices and emergency departments. More complex neural blockade procedures should be carried out in an otherwise suitable anesthetizing location such as the preinduction area, operating room, PACU, or an appropriately equipped special procedure area (radiologic procedure area, pain management unit, etc.). Regardless of the location, an area of sufficient size, with proper lighting and equipment to safely and efficiently perform the procedure, is required. Neural blockade procedures for surgical patients may be more conveniently and efficiently performed in a dedicated regional anesthesia holding area, similar to induction areas, where the block can be performed while a preceding operative procedure is being completed or while the operating room is being prepared for the patient. This system has been used in several centers and provides a significant efficiency advantage in terms of improving operating room turnover times, improving the success rate of neural blockade procedures, and improving overall acceptance of regional anesthesia techniques (Fig. 8-2).
Patient Positioning and Documentation
Considerations for patient positioning for neural blockade procedures should ensure patient safety and comfort and optimize the successful performance of the anesthetic procedure. Some
neural blockade procedures may require the enlistment of an assistant to help maintain patient safety and comfort. Special care should be taken with patients placed in the sitting position following or during the administration of sedative medications.
neural blockade procedures may require the enlistment of an assistant to help maintain patient safety and comfort. Special care should be taken with patients placed in the sitting position following or during the administration of sedative medications.
Appropriate documentation of neural blockade procedures is important for continuity of patient care, medicolegal considerations, and billing and compliance issues. Simple neural blockade procedures may only require a brief note on the anesthetic record or in the progress notes of the patient’s chart. More extensive procedures may require more extensive documentation including the patient’s consent, patient positioning, sedative agents administered, skin preparation, block technique, needle or catheter used, local anesthetic used and total dose administered, patient response, and documentation of any problems or complications. Because of the amount of space required on the anesthetic record for this level of documentation, and to standardize and improve efficiency of documentation of regional anesthesia procedures, a standardized neural blockade procedure note may be helpful (Figs. 8-3 and 8-4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree