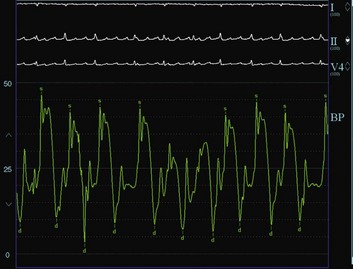
6 ETIOLOGY OF PERICARDIAL EFFUSION AND TAMPONADE DIAGNOSTIC ROLE OF ECHOCARDIOGRAPHY CATHETER-BASED DIAGNOSTIC AND THERAPEUTIC STRATEGIES OPEN SURGICAL PERICARDIAL WINDOW PERCUTANEOUS BALLOON PERICARDIOTOMY Percutaneous Balloon Pericardiotomy Technique Outcome Data after Percutaneous Balloon Pericardiotomy Pericarditis or pericardial effusion or both may result from an infectious, metabolic, inflammatory, autoimmune, or neoplastic process (Box 6.1).1–3 The frequency of specific causes depends on the geographic location, time period, and characteristics of the populations studied. In one European series of patients presenting with moderate and severe pericardial effusions, acute idiopathic pericarditis and iatrogenic causes accounted for most cases.1 In a smaller series in the United States comprising patients presenting to a tertiary medical center with large pericardial effusions, malignancy was the most common cause.4 Pericardial effusions occurring after radiation therapy, myocardial infarction, and surgical and interventional cardiac procedures are increasing in incidence. Uremia and hypothyroidism remain important causes but are seen less frequently given the prompt diagnosis and treatment of these disorders. Pericardial fluid can be either a transudate or an exudate. Although transudative effusions typically occur in patients with congestive heart failure, exudative effusions may occur with most types of pericarditis and are characterized by a high concentration of proteins and fibrin. Pericardial effusions may be serous (or serosanguineous), suppurative, or hemorrhagic. Although the presence of suppurative effusion is pathognomonic for an acute infectious cause, usually bacterial, hemorrhagic pericardial effusion is commonly related to chronic infections, with tuberculosis a classic example, particularly in developing countries. In developed countries, hemorrhagic pericardial effusions are likely to be iatrogenic or malignant in origin. In a retrospective analysis of 150 patients in the United States who underwent pericardiocentesis for relieving cardiac tamponade, 64% of patients had a hemorrhagic pericardial effusion (with iatrogenic causes and malignancy accounting for most cases).5 The normal pericardium is a fibroelastic sac composed of visceral and parietal layers separated by the pericardial cavity and containing a thin layer (20 to 50 mL) of straw-colored fluid surrounding the heart.3 The normal pericardium has a steep pressure-volume curve: It is distensible when the intrapericardial volume is small, but becomes gradually inextensible when the volume increases. In the presence of pericardial effusion, the intrapericardial pressure depends on the relationship between the absolute volume of the effusion, the speed of fluid accumulation, and pericardial elasticity. Although the rapid accumulation of small amounts of fluid (150 to 200 mL) can result in cardiac tamponade, the slow accumulation of larger effusions (>1 L, as in uremic pericardial effusions) is usually well tolerated.6,7 The clinical presentation is not only related to the size of the effusion, but also, and more importantly, to the rapidity of fluid accumulation. Pericardial tamponade is a clinical syndrome with defined hemodynamic and echocardiographic abnormalities, which result from the accumulation of intrapericardial fluid and impairment of ventricular diastolic filling.7,8 The ultimate mechanism of hemodynamic compromise is the compression of cardiac chambers secondary to increased intrapericardial pressure.8 Pericardial tamponade is usually a clinical diagnosis, with patients showing elevated systemic venous pressure, tachycardia, dyspnea, arterial pulsus paradoxus, muffled heart sounds, and evidence of electrical alternans on electrocardiogram (ECG).3 Pulsus paradoxus, which describes the exaggerated inspiratory decline in arterial blood pressure (>10 mm Hg), is largely attributed to interventricular dependence within the confined pericardial space. Although its diagnostic utility was recognized many decades earlier,9 various conditions may lead to its absence in patients with cardiac tamponade (e.g., in patients with concomitant aortic regurgitation, atrial septal defects, severe left ventricular dysfunction, aortic regurgitation, severe hypotension, pericardial adhesions, pulmonary artery obstruction, or positive-pressure ventilation).8 The ECG shows sinus tachycardia and low voltage. Electrical alternans, which describes the beat-to-beat alterations in the QRS complex reflecting cardiac swinging in the pericardial fluid, is a relatively specific sign for tamponade and is rarely seen with very large pericardial effusions alone.10 Patients with pericardial effusions have an enlarged cardiac silhouette with clear lung fields on chest radiograph. The pericardial effusion has to reach 200 mL in volume to appear on the chest radiograph, and this volume occurs usually in slowly accumulating pericardial effusions (which are less likely to cause tamponade).11 Rapidly accumulating small pericardial effusions may cause tamponade and have a normal chest radiograph. The diagnosis of pericardial tamponade is best confirmed by a two-dimensional echocardiogram that shows a pericardial effusion, right atrial compression, and abnormal respiratory variations in the right and left ventricular dimensions and in the tricuspid and mitral valve flow velocities (Fig. 6.1).12 The classic hemodynamic findings of pericardial tamponade include arterial pulsus paradoxus, elevation and diastolic equalization of right and left ventricular diastolic pressures with pericardial pressure, and depression of cardiac output.8 Because patients with critical tamponade operate on the steep portion of the pericardial pressure-volume curve, drainage of even a small pericardial volume causes a dramatic reduction in intrapericardial pressure and rapid clinical and hemodynamic improvement (by shifting the stretched pericardium back to the flat portion of the pericardium pressure-volume curve).8 Echocardiography is recognized as a particularly useful imaging modality for pericardial disease.13,14 Currently, two-dimensional echocardiography has become the gold standard diagnostic modality because it provides a highly sensitive and specific noninvasive imaging technique for pericardial disease.12,15 It is also an important tool for the longitudinal follow-up of pericardial effusions over time (given a class IIa recommendation in the American Heart Association/American College of Cardiology guidelines for the clinical application of echocardiography).12 Classically, a persistent echo-free space throughout the cardiac cycle between the parietal pericardium and the epicardium is pathognomonic for pericardial effusion by M-mode echocardiography.13 Two-dimensional echocardiography allows delineation of the size and distribution of the effusion, including loculated effusions, and helps assess the success of pericardiocentesis. The echocardiogram also can provide a reasonable estimate of the total volume of the effusion.15 Circumferential effusion greater than 1 cm in width is considered large (>500 mL). Moderate effusions (100 to 500 mL) are usually circumferential but less than 1 cm, whereas small effusions (<100 mL) are usually localized posterior to the left ventricle and measure less than 1 cm. Classification criteria differ significantly among various echocardiographers and institutions. The typical echocardiographic signs of pericardial tamponade are listed in Box 6.2. The nature of the pericardial fluid is difficult to identify by echocardiography. Increased echogenicity is suspicious, however, for the presence of proteins or cells or both in the pericardial fluid. Fibrin deposits localized in the epicardial surface can be identified as echogenic masses. In one study of 42 patients with tuberculous and viral or idiopathic pericardial effusions, intrapericardial echocardiogram abnormalities, such as a greater degree of pericardial thickening, frequency and thickness of exudative coating or deposits, and strands crossing the pericardial space, were useful criteria in the diagnosis of tuberculous pericardial effusion and in differentiating it from chronic idiopathic pericardial effusion.16 The classic echocardiographic signs of cardiac tamponade are right atrial and right ventricular diastolic collapse. The right atrium and right ventricle are compliant structures. As a result, increased intrapericardial pressure leads to their collapse when intracavitary pressures are only slightly exceeded by those in the pericardium. At end diastole (i.e., during atrial relaxation), right atrial volume is minimal, but pericardial pressure is maximal, causing the right atrium to buckle. Right atrial collapse, especially when it persists for more than one third of the cardiac cycle, is a highly sensitive but less specific sign for tamponade. Early diastolic collapse of the right ventricle (usually occurs in early diastole when the ventricular volume is still low) is present when the intrapericardial pressure exceeds the right ventricular pressure and is a highly specific sign for tamponade. Right ventricular collapse may not occur when the right ventricle is hypertrophied, or its diastolic pressure is greatly elevated. Left atrial collapse is seen in nearly 25% of patients and is specific for tamponade. Left ventricular collapse is less common because the wall of the left ventricle is more muscular. Dilation of the inferior vena cava with lack of inspiratory collapse (usually <50% reduction in its diameter) and swinging of the heart also are seen in patients with pericardial tamponade. Doppler echocardiography provides direct assessment of the ventricular filling patterns in pericardial tamponade.11,12,17,18
Pericardial Tamponade
Clinical Presentation, Diagnosis, and Catheter-Based Therapies
Etiology of Pericardial Effusion and Tamponade
Clinical Presentation
Diagnostic Role of Echocardiography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Anesthesia Key
Fastest Anesthesia & Intensive Care & Emergency Medicine Insight Engine