Bony anatomy of the pelvis.
Focused history and physical exam
History
Location of pain is important. (see Table 5.1)
Trauma
Should try to distinguish whether this is high energy, low energy, or repetitive stress.
Timing of pain or other symptoms is important.
Pain occurring with running for some time that gets abruptly worse may indicate a stress fracture.
A pop or snapping sensation may indicate a muscular or tendinous disorder.
Resolution of pain with rest can be indicative of several disorders such as stress fracture or a vascular issue.
| Groin | Core muscle weakness or injury Pelvic fracture Osteitis pubis Athletic pubalgia Femoral neck stress fracture Femoroacetabular impingement Snapping hip Acetabular labral tear Slipped capital femoral epiphysis Hip fracture Hip dislocation Transient synovitis of the hip Septic arthritis Osteonecrosis of the hip Osteoarthritis of the hip |
| Anterior hip and upper leg | Core muscle weakness or injury Hip pointer Pelvic fracture Athletic pubalgia Femoral neck stress fracture Femoroacetabular impingement Snapping hip Acetabular labral tear Slipped capital femoral epiphysis Hip fracture Hip dislocation Transient synovitis of the hip Osteonecrosis of the hip Quadriceps hernia Quadriceps strain or tear |
| Posterior hip and upper leg | Core muscle weakness or injury Sacroiliac joint dysfunction Pelvic fracture Piriformis syndrome Ischial tuberosity avulsion fracture Femoroacetabular impingement Snapping hip Hip fracture Hip dislocation Osteonecrosis of the hip Hamstring strain or tear |
| Lateral | Core muscle weakness or injury Hip pointer Snapping hip Trochanteric bursitis Hip fracture Hip dislocation Osteonecrosis of the hip Meralgia paresthetica Iliotibial band syndrome |
Physical Exam
Pelvis/hip exam done in five positions: Standing, Seated, Supine, Lateral position, and Prone
Physical exam will be discussed in the order of position, which is the most efficient way to do the exam.
Normal values for hip range of motion can be found in Table 5.2.
Standing Exam
Spinal alignment assessed by looking at:
Shoulder/iliac crest height
Lumbar lordosis
Scoliosis
Pelvic alignment assessed by comparing contralateral:
Anterior superior iliac spines and iliac crests
Gait
Watching patient walk in the room or in the hallway may provide a lot of information.
Antalgic gait is a sign of hip pain
Excessive internal or external rotation
Short leg limp indicates leg length discrepancy.
Trendelenburg gait indicates core muscle weakness.
Trendelenburg test
Have patient stand comfortably then stand on one leg (Figure 5.2)
When on one foot, the contralateral hemipelvis should raise slightly or at least stay at the same height (Figure 5.3).
A drop in the contralateral hemipelvis is a sign of core muscle weakness, specifically of the gluteus medius (Figure 5.4).
Seated Exam
Active internal rotation of hip (Figure 5.5)
Active external rotation of hip (Figure 5.6)
Be sure to check passive range of motion if active range of motion is limited
Supine Exam
Vascular evaluation
Femoral artery
Popliteal artery
Dorsalis pedis artery
Posterior tibial artery
Capillary refill
Neurologic evaluation
See Table 5.3 for central nerve roots and corresponding sensory and motor innervation.
Evaluation for open-book pelvis or unstable pelvis (Figure 5.7)
Thumbs should be placed inferior to anterior superior iliac spine with palms resting between iliac crest and greater trochanter.
Pelvis should be squeezed in an attempt to bring thumbs together.
Pelvis should NEVER be opened by attempting to separate thumbs further as this could lead to disruption of clot and precipitate massive hemorrhage
Passive ROM
Log roll of leg will be painful with most intra-articular processes as well as hip fractures.
Hip flexion, abduction, adduction (see Table 5.2)
Straight leg raise is performed by passively flexing hip with fully extended knee (Figure 5.8).
Positive test for diagnosis of sciatica is pain that radiates down leg and past the knee when flexed from 15–70°.
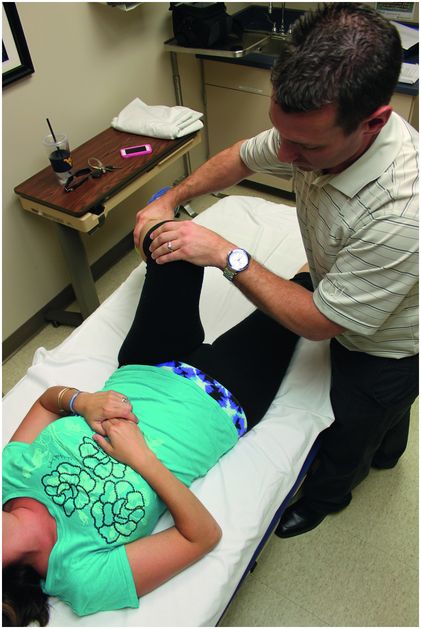
Flexion Abduction External Rotation (FABER) test, also called Patrick test (Figure 5.9)
Place patient in cross-legged position then apply posterior pressure to knee.
Posterior pain indicated sacroiliac dysfunction.
Groin pain may indicate intra-articular hip process or possibly adductor strain.
Lateral pain may indicate femoroacetabular impingement. (FAI)
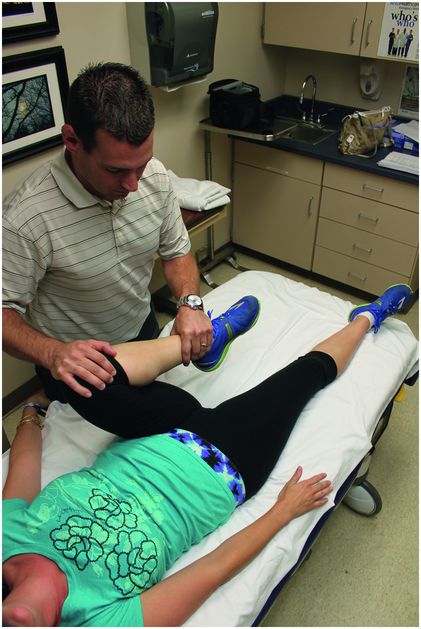
Flexion Adduction Internal Rotation (FADDIR) test (Figure 5.10)
Most preferred test for FAI
While supine, place patient into full hip flexion, adduction, and internal rotation
This will cause reproducible and very uncomfortable groin pain in a positive test.
Acetabular labrum testing
There are several tests for acetabular labral tears that involve passively moving the femur about the pelvis.
These will not be covered in detail here, but the main finding with each is a reproducible painful motion, click, or burning sensation typically felt in the groin.
Thomas stretch test (Figure 5.11)
Nonaffected leg into extreme flexion
Unable to keep contralateral hip extended indicates tight iliopsoas musculature
Strength testing
Hip abduction/adduction tested with hips and knees flexed
Iliopsoas
Only 15°
Palpation
Abdominal fascia
Iliac crest
Anterior superior iliac spine
Anterior inferior iliac spine
Ilioinguinal ligament
Pubic symphysis
Resisted sit-up (Figure 5.12)
Lateral Exam
Active/Passive ROM
Hip extension
Ober’s test (Figure 5.13)
Test for iliotibial band tightness
Adduct/extend hip with knee flexed
Positive test: Knee unable to drop below neutral position
Piriformis test (Figure 5.14)
Hip and knee flexed with knee hanging off table
Stabilize pelvis and down on knee gives pain in buttock
Strength testing
Hip abduction
Palpation
Greater trochanter
Tensor fascia lata and iliotibial band
Prone Exam
Passive ROM
Hip internal/external rotation
Femoral nerve stretch test (Figure 5.15)
Stabilize pelvis, other hand under thigh.
Extend hip keeping knee flexed
Strength testing
Hip internal rotation
Gluteus maximus isolated by extending hip with knee flexed to 90° (Figure 5.16).
Piriformis isolated by externally rotating hip with the hip in full internal rotation and the knee flexed to 90° (Figures 5.17 and 5.18).
Ischial tuberosity
Piriformis muscle
Sciatic nerve
| Flexion Extension Abduction Adduction External rotation Internal rotation | 0–120° 0–30° 0–45° 0–30° 0–50° 0–40° |

For the Trendelenberg Test, the patient should stand on the painful leg. On a normal test (Figure 5.3) the contralateral hemipelvis raises slightly or stays at the same height. On an abnormal test (Figure 5.4) the contralateral hemipelvis drops.
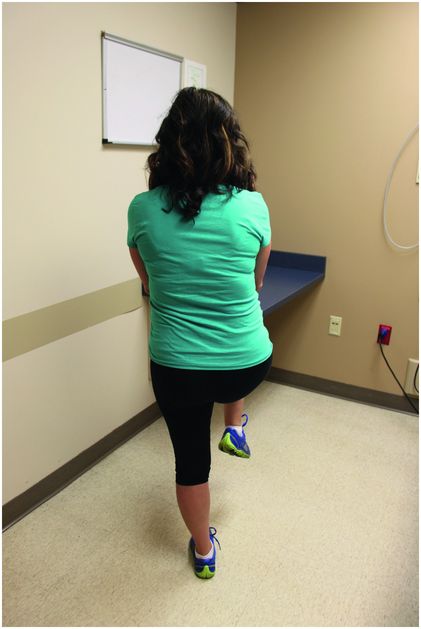 Figure 5.3.
Figure 5.3.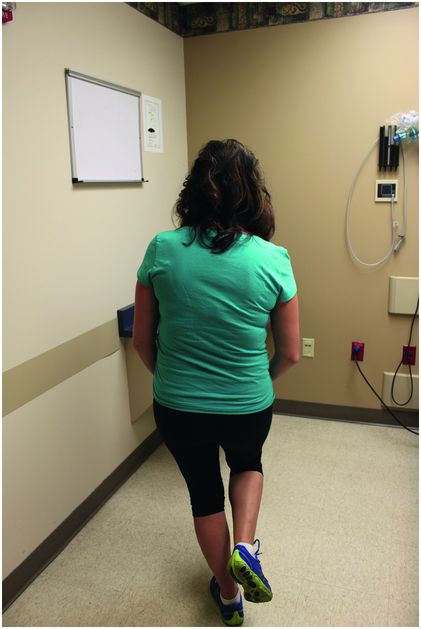 Figure 5.4.
Figure 5.4.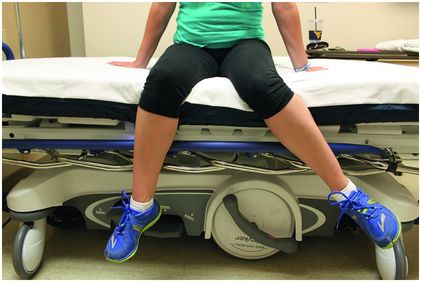
This is internal rotation of the hip. Note that the foot actually moves laterally.
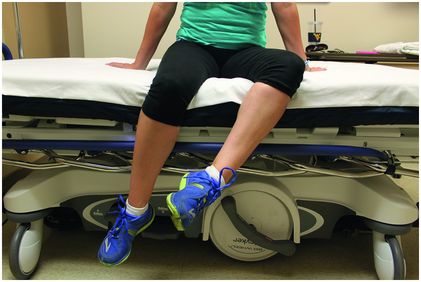
This is external rotation of the hip. Note that the foot actually moves medially.
| Nerve Root | Sensory | Motor |
|---|---|---|
| L1 | Just below inguinal ligament | Hip flexion |
| L2 | Middle anterior thigh | Hip adduction |
| L3 | Lower anterior thigh | Knee extension |
| L4 | Medial lower leg and foot | Ankle dorsiflexion |
| L5 | Lateral lower leg and dorsal foot | Great toe MTP and IP extension |
| S1 | Lateral foot | Plantar flexion and eversion of the foot |

This shows the beginning position for testing for an unstable pelvic fracture or open-book pelvis. The examiner should then attempt to squeeze thumbs together. With an unstable fracture, the examiner will get his thumbs closer together when squeezing.
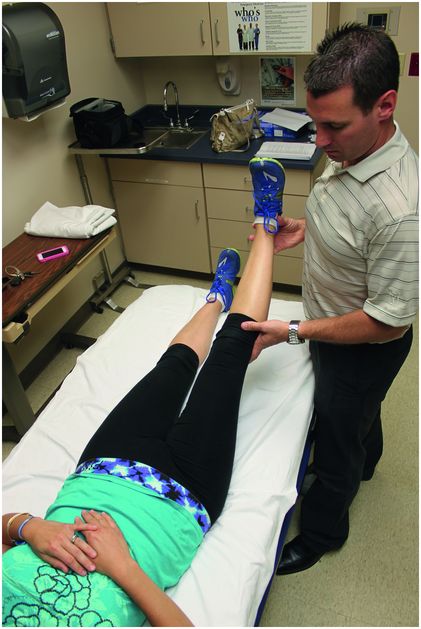
The straight leg raise test may be helpful for diagnosing sciatica.

The FABER test may be helpful in the diagnosis of several disorders including sacroiliac dysfunction, femoroacetabular impingement, or intra-articular hip pain.
The FADDIR test is the most preferred test for femoroacetabular impingement.
The Thomas stretch test may indicate tight iliopsoas musculature.

The resisted sit-up may aid the diagnosis of athletic pubalgia or “sports hernia” but may also be painful in other disorders such as osteitis pubis.
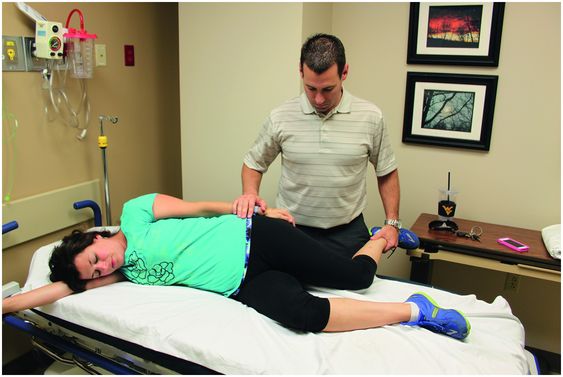
Ober’s test places stress on and may indicate tightness of the iliotibial band.

Piriformis test places stress on the piriformis muscle and may recreate the symptoms of piriformis syndrome.
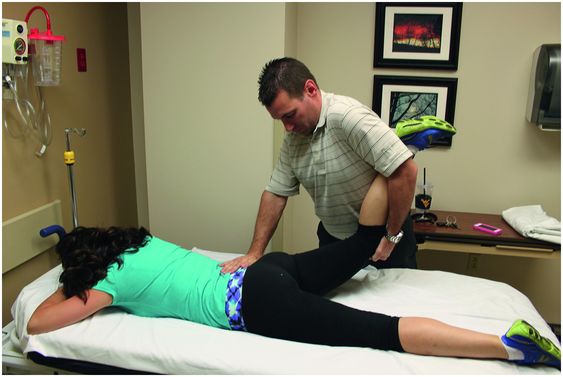
This shows the position for the femoral nerve stretch test.
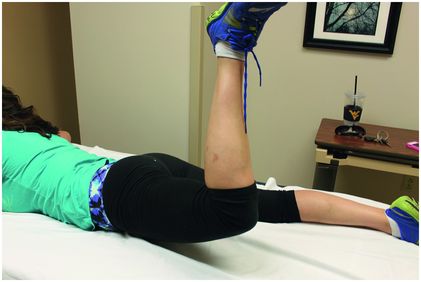
Testing strength in this position may isolate the gluteus maximus.

When testing the strength of the piriformis muscle, start in the position shown in Figure 5.17 and move the foot medially to the position shown in Figure 5.18.
 Figure 5.18.
Figure 5.18.Differential Diagnosis – Emergent and Common Diagnoses
Pelvis
Core muscle weakness or injury
Hip pointer
Sacroiliac joint dysfunction
Pelvic fracture
Piriformis syndrome
Osteitis pubis
Ischial tuberosity avulsion fracture
Athletic pubalgia (Sports hernia)
Hip
Thigh
Meralgia paresthetica
Iliotibial band syndrome
Quadriceps hernia
Hamstring strain or tear
Quadriceps strain or tear
| Emergent Diagnoses | Common Diagnoses |
|---|---|
| Unstable pelvic fracture | Core muscle weakness or injury |
| Slipped capital femoral epiphysis | Hip pointer |
| Hip fracture | Sacroiliac dysfunction |
| Hip dislocation | Piriformis syndrome |
| Septic arthritis of the hip | Trochanteric bursitis |
| Legg–Calve–Perthes disease | Transient synovitis of the hip |
| Complete hamstring or quadriceps tear | Osteoarthritis of the hip |
| Iliotibial band syndrome | |
| Hamstring and quadriceps strain |
Pelvis
Core Muscle Weakness or Injury
General Description
The muscles of the abdominal wall, pelvis, buttock, and hip are generally referred to as the core muscles.
Together, these muscles stabilize the trunk and pelvis to provide the base for coordinated movement.
Several injuries and areas of pain are associated with core muscle weakness or abnormality.
Mechanism
Core weakness or injury results in a derangement of the mechanics of ambulation or movement of the trunk
This derangement typically causes overcompensation by the other muscles of the core.
Pain may result from the initial injury or the overcompensation.
Presentation
May present with back pain, sacroiliac pain, hip pain, groin pain, or pelvic pain.
Physical exam
Attempt to isolate movement or movements that elicit pain since this will indicate affected muscle or muscle group.
Trendelenburg test or Trendelenburg gait signifies weakness of the contralateral gluteus medius.
Essential Diagnostics
Bone injury should be ruled out with radiographs or CT scan.
Stress injury of pelvis or hip may need MRI or bone scan evaluation.
Musculoskeletal ultrasound may show muscle abnormalities in the hands of an experienced operator.
ED Treatment
Splint: None needed
Weight-bearing status: As tolerated
If stress fracture strongly suspected, non–weight-bearing is appropriate
Instructions on core strengthening exercises such as yoga poses which may be done once a day for 30–60 seconds per pose
High plank (Figure 5.19) and low plank (Figure 5.20)
Downward facing dog (Figure 5.21) and upward facing dog (Figure 5.22)
Chair (Figure 5.23)
Halfway lift (Figure 5.24) and Warrior 1 (Figure 5.25)
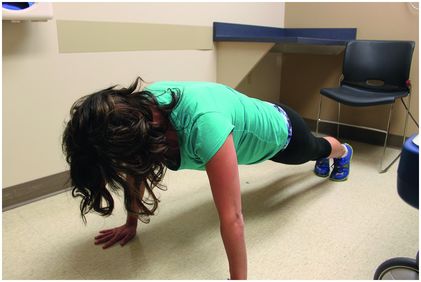
High plank position.

Low plank position.
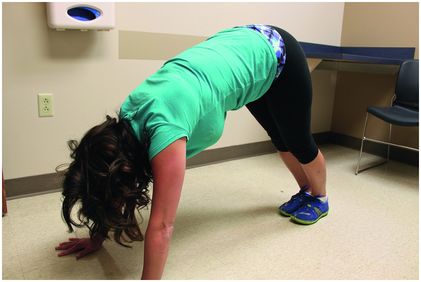
Downward facing dog position.

Upward facing dog position.
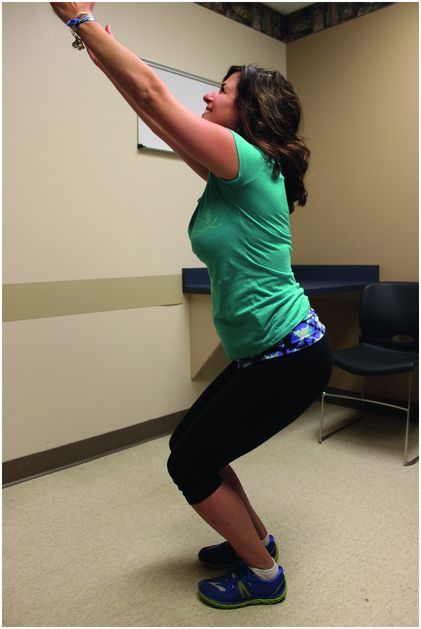
Chair position.
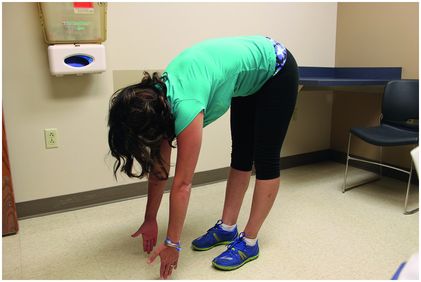
Halfway lift position.

Warrior 1 position.
Disposition
Discharge unless not safe at home due to severe limitation in ambulation
Follow-up with primary care provider (PCP)or sports medicine physician in next one to two weeks who may order physical therapy if needed
Return to work or sports as tolerated
Complications
Severe chronic weakness may lead to early degenerative changes in hip due to derangement in gait.
Pediatric Considerations
Take special care to evaluate physes on exam and with radiographs since avulsion fractures may be easily confused for muscular abnormalities.
At times of rapid growth, core weakness or relative imbalance is common and may resolve with time alone.
Pearls and Pitfalls
Bony injury should be ruled out.
Simple core strengthening exercises are the treatment of choice.
Musculoskeletal ultrasound may be helpful in the hands of an experienced operator.
Hip Pointer
General Description
This is a contusion of the iliac crest that is often associated with a subperiosteal hematoma.
This injury most commonly occurs in football players.
Mechanism
This is due to a direct blow to the area usually following a collision or a fall.
Presentation
Athlete will usually complain of pain in the area of the iliac crest.
Often they will relate a history of trauma.
Essential Diagnostics
Anteroposterior pelvis x-ray to rule out fracture
ED Treatment
Relative rest, ice and anti-inflammatories to reduce swelling
May recommend gentle range of motion and strengthening exercises as tolerated
Disposition
Discharge
Follow-up with sports medicine or PCP in one week
May return to sport once pain and swelling have subsided enough to allow safe return
Complications
Usually self-limited condition
Occasionally, significant hemorrhage into muscle may occur and lead to prolonged limitations and disability
Pediatric Considerations
If this injury occurs in a child with open growth plates it is possible to sustain an avulsion fracture of the anterior superior iliac crest
These are some of the last growth plates to close
These injuries are rare and may usually be managed conservatively.
Initial treatment is with rest, ice, and non weight-bearing with crutches for two to three weeks until able to ambulate without pain.
Initiate stretching and strengthening program
Athletes may usually return to sports eight to twelve weeks after injury.
Pearls and Pitfalls
Usually a benign, self-limiting injury
Extra caution is needed in younger patients with open growth plates who are at risk of sustaining an avulsion fracture at the anterior superior iliac spine.
Sacroiliac Joint Dysfunction
General Description
Broad term that many view as a “wastebasket” diagnosis
Relatively immobile joint
High-energy pelvic injuries frequently cause fractures here, but sacroiliac joint dysfunction typically refers to low-energy disorders
Mechanism
Arthritis in the sacroiliac joint may be caused by rheumatologic disorders or trauma.
Septic arthritis should be considered in the appropriate clinical picture.
Presentation
Pain attributed to the sacroiliac joint may cause buttock or posterior thigh pain
Physical Exam
Classically, FABER test (Figure 5.9) used to elicit pain in this area
Tenderness of sacroiliac joint
Essential diagnostics
High-energy injuries require CT scan to rule out pelvic fractures which may be easily missed on plain films.
CT scan with IV contrast or MRI may be needed to evaluate for sacroiliitis especially when infectious etiology suspected.
When infectious etiology is being considered, labs ordered should include complete blood count (CBC), C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR).
Basic metabolic panel is typically included as well in case intravenous antibiotics are needed.
ED Treatment
Splint: Not needed.
Weight-bearing status: As tolerated
Ice and non-steroidal anti-inflammatory drugs (NSAIDs) are typically acute treatments.
Short period of rest may also be necessary
If infectious sacroiliitis, intravenous antibiotics should be started as early as possible.
If patient is being taken to the operating room for washout, consulting orthopedist may delay initial antibiotics until cultures are obtained.
Appropriate if patient is stable and relatively uncomplicated (i.e., no diabetes or immunosuppression).
Disposition
Discharge typically appropriate unless being admitted for intravenous antibiotics
Orthopedic consultation needed when infectious process is suspected.
Follow-up in one to two weeks with PCP or sports medicine physician is typically appropriate.
Return to work or sports as tolerated
May take several weeks for return to normal
Complications
May be due to ankylosing spondylitis which includes other serious symptoms such as spine deformities, lung problems, and heart problems.
When resulting in gait abnormalities, early degenerative changes may occur.
Pediatric Considerations
Rheumatologic conditions should be considered in children.
Follow-up with PCP and possibly rheumatologist will be useful since the majority of rheumatologic testing will be done as outpatient.
Pearls and Pitfalls
Overlooked infectious etiology may result in severely disabling consequences and even sepsis.
For noninfectious etiology, ice and NSAIDs are the typical treatments.
Short rest period may be needed, but patient should be encouraged to get back to normal activities as soon as possible
Pelvic Fractures
General Description
Large range of injuries typically from a high-energy impact but may result from relatively minor trauma when bones are weak such as in osteoporosis or cancer.
Mechanism
Falls and motor vehicle crashes are common causes of pelvic fractures.
Since the pelvis is a bony ring, once a fracture is seen great care should be taken to find a second fracture or ligamentous disruption (i.e., sacroiliac joint derangement).
Presentation
Pain is typically localized to near the fracture.
Groin pain may indicate acetabular or intra-articular fracture.
Physical Exam
Pelvis palpated for tenderness.
Evaluate for unstable pelvis by squeezing pelvis as described earlier in physical exam section (Figure 5.7).
Log roll of leg to evaluate for intra-articular fracture or hip fracture
Essential Diagnostics
Pelvis radiographs may show fracture but do not exclude fractures.
Diastasis at pubic symphysis greater than 1 cm indicates pubic instability except in women post childbirth.
Diastasis greater than 2.5 cm indicates sacroiliac ligamentous disruption.
CT scan is imaging modality of choice for pelvic fractures.
ED Treatment
If pelvis unstable, pelvic binder should be applied low on the pelvis as instructed.
If no binder is available, a sheet may be tied low and tight on the pelvis at the level of the greater trochanters.
For unstable fractures, patient should be non weight-bearing.
For stable fractures such as pubic rami fractures and many iliac crest fractures, patient may be toe-touch weight-bearing to start and progressed as pain allows, but this should be coordinated with the orthopedist who will be following the patient.
Narcotic pain medications are typically used for the first few days to weeks after a fracture but should be phased out as soon as possible.
Disposition
Unstable fractures are admitted.
Emergent consult to orthopedics for unstable pelvic fracture (i.e., any time binder is applied) especially with hemodynamic instability.
Should consult for other fractures as well
Open reduction with internal or external fixation will be needed for unstable fractures.
Return to work or sports to be determined by extent of fractures.
Complications
Unstable pelvic fractures are associated with large amounts of bleeding into the pelvis that may be life threatening.
Unstable pelvic fractures also have a high association with urethral injuries so Foley catheter should not be inserted in the ED unless a retrograde urethrogram has been performed.
Pearls and Pitfalls
If one fracture is found, look hard for a second fracture since pelvis is a bony ring.
Urethral catheter insertion should be deferred until retrograde urethrogram performed if unstable pelvis fracture.
Stable fractures may be treated conservatively with crutches and outpatient follow-up.
Piriformis Syndrome
General Description
Irritation of the sciatic nerve which runs over the piriformis muscle.
In 20 percent of the population, the piriformis is split with the sciatic nerve actually dividing the muscle.
Mechanism
Several etiologies have been proposed such as hyperlordosis, muscle anomalies with hypertrophy, anatomic variants of the course of the sciatic nerve or its’ divisions.
Also may be caused by external forces such as sitting for a long period of time or on an object such as a wallet.
Foot abnormalities, such as Morton foot, may precipitate piriformis syndrome due to compensation needed by the piriformis to correct the gait abnormality.
Presentation
Pain may be localized deep in posterior hip or buttock.
If sciatic nerve is irritated, pain may be described as burning or may radiate down leg.
Physical Exam
Pain precipitated by passive internal rotation and active external rotation (Figures 5.5 and 5.6).
Piriformis test described earlier (Figure 5.14)
Essential Diagnostics
Very little may be needed for this diagnosis in the emergency department.
Testing would typically center around ruling out other causes such as cauda equina.
Outpatient testing may include MRI of lumbar spine to exclude disc herniation.
ED Treatment
Splint: Not needed
Weight-bearing status: As tolerated.
NSAIDs are used frequently.
Steroid burst for five days may be used but typically not first line for most practitioners.
Other medications such as gabapentin or pregabalin are prescribed for neuropathic pain but are frequently ineffective.
Disposition
Discharge to home
Indications to consult orthopedics (spine) would include concern for cauda equina or rapidly progressing neurologic changes.
Follow-up in one to two weeks with PCP or sports medicine physician.
Physical therapy is the typical first-line treatment but injections may be attempted.
Return to work or sports as tolerated.
Once sciatic nerve irritated, full recovery may take a few months.
Complications
Sciatica as a result of piriformis syndrome may be quite debilitating and painful.
Severe and chronic piriformis dysfunction may cause gait abnormalities and early degenerative changes.
Pearls and Pitfalls
May be easily confused for lumbosacral sciatica.
Due to course of sciatic nerve, some patients will be predisposed to problems arising from the piriformis and should be counseled about high likelihood of future events.
Osteitis Pubis
General Description
Inflammation of pubic symphysis seen after suprapubic surgery or in athletes.
May be related to core weakness or a traumatic event.
Mechanism
Likely results from repetitive microtrauma to pubic symphysis from several sources
Pregnancy and childbirth
Major trauma
Repeated minor trauma
Urologic or gynecologic surgery
Athletic activities that require cutting movements
Core muscle weakness and sacroiliac joint hypermobility or hypomobility may cause additional stress on pubic symphysis.
Infectious etiology and osteomyelitis also a possible cause.
Presentation
Pain directly over pubic symphysis is common.
Other possible presenting complaints:
Inguinal pain on one or both sides
Weakness and difficulty ambulating
Clicking or popping around pubic symphysis when standing or rolling over in bed
Physical Exam
Tenderness over pubic symphysis
Tenderness over superior pubic rami
If sacroiliac dysfunction is involved, FABER testing (Figure 5.9) may elicit pain in sacroiliac joint.
Pain with resisted hip adduction
Make sure to rule out inguinal, femoral, or sports hernia
Essential Diagnostics
Other diagnoses must be entertained such as pubic rami stress fracture.
Radiographs of the pelvis should be obtained.
CT scan of pelvis may be useful to rule out other pathology but is not required. This may be performed as an outpatient
MRI may be necessary but very rarely, if ever, needed in the emergency department.
If concerned for infectious etiology, ESR and CRP ordered in addition to CBC.
ED Treatment
Splint: Not needed.
Weight-bearing status: As tolerated.
If concerned for osteomyelitis, antibiotics should be started as soon as possible.
NSAIDs may be useful and should be started in the ED unless contraindicated.
An oral steroid course may be useful as well but is typically reserved for protracted case.
Disposition
Discharge unless osteomyelitis needing IV antibiotics.
Orthopedic consult in the ED likely only needed for osteomyelitis.
Follow-up recommended in one to two weeks.
Activity modification
Return to work or sports should be cautious depending on activities.
Complications
Average time to full recovery is between seven and ten months.
May take up to thirty-two months.
For athletes who refuse to modify activities or rest, aggressive physical therapy and judicious use of medications may return them to prior level of activity.
Pediatric Considerations
For young athletes, the importance of activity modification and rest should be emphasized.
Typical duration of symptoms may significantly disrupt the young athletes’ goals and success so treatment should be aggressively undertaken.
Pearls and Pitfalls
May be a very long course with average time to resolution of seven to ten months.
Osteomyelitis and stress fracture should be on the differential when considering osteitis pubis.
Activity modification, rest, and anti-inflammatory medications are the typical recommendations.
Ischial Tuberosity Avulsion fracture
General Description
Avulsion fracture of ischial tuberosity due to forceful contraction of hamstring muscle complex.
May be final endpoint of stress fracture of ischial tuberosity.
Mechanism
Hamstring attaches to ischial tuberosity and forceful contraction causes avulsion of bone.
Stress reaction and stress fracture of ischial tuberosity may weaken the bone here and predispose the patient to avulsion.
Presentation
Likely has severe pain with abrupt onset.
Patient can usually recall the exact kick or step when it happened.
May have been preceded by aching pain in this area in case of stress reaction/stress fracture.
Pain localized to buttock or proximal hamstring.
Physical Exam
Tenderness of ischial tuberosity and proximal hamstring.
Pain aggravated by resisted knee flexion.
May see bruising of proximal posterior leg.
Essential Diagnostics
Radiographs are key to diagnosis.
Musculoskeletal ultrasound may be beneficial for ruling out hamstring tear.
CT may be necessary if clinical suspicion is high.
ED Treatment
Splint: Not needed.
Weight-bearing status: Non-weight bearing
Pain control
Disposition
Discharge likely
Orthopedic consultation only for significantly displaced fractures to arrange early surgical intervention.
Follow-up in next two to three days with orthopedics or sports medicine (if not significantly displaced)
Return to work or sports will likely take several weeks for active work or sports.
Complications
If not treated early, hamstring contracture will make repair and recovery of function much more difficult.
Pediatric Considerations
Open physes may make this diagnosis more difficult but unequal physes should be worked up further.
Due to relative weakness of physes compared with bone, tendon, and muscle, avulsions will likely happen directly through physes resulting in Salter–Harris I fractures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








