KEY POINTS
Hemorrhage from pelvic injuries is frequently underestimated, leading to delayed diagnosis and treatment.
Pelvic ring injuries are commonly associated with other significant injuries resulting in major morbidity and mortality.
Initial management of pelvic injuries requires hemorrhage control and volume resuscitation.
Provisional acute stabilization of the pelvis using a binder or external fixation is a key element in the initial control of hemorrhage from pelvic fractures.
Extremity fractures, though frequently not life threatening, require accurate diagnosis and appropriate management to prevent significant disability and morbidity.
Complications of extremity injuries, such as compartment syndrome and neurovascular compromise, can best be detected by a high index of suspicion, careful assessment, and institution of appropriate preventive measures.
Knowledge of the mechanism of injury is important in predicting the type and severity of extremity injuries.
PELVIC RING INJURIES
Patients sustaining major pelvic and extremity trauma frequently are managed in the ICU setting. These patients may present with significant hemodynamic abnormality owing to their associated injuries, and this can be compounded by inadequate resuscitation resulting from underestimation of the volume of blood loss associated with such injuries. The following information is provided to assist the intensivist in understanding extremity and pelvic ring injuries, thus allowing early diagnosis with prompt and appropriate management aimed at preventing major morbidity and mortality.
Significant force is required to sustain an injury to the pelvic ring. In various epidemiologic studies, mortality rates of up to 25% have been reported, depending on the pattern and severity of the pelvic injury.1,2 While the direct cause of death is usually attributed to a head or thoracic injury,3 pelvic bleeding significantly contributes to this high rate of mortality. There is an increased risk of mortality in association with open pelvic fractures, a high injury severity score (ISS), or concomitant head, thoracic, abdominal, or neurologic injury.4 The incidence of associated injuries is relatively common (Table 121-1).3 A team approach is required to treat trauma victims adequately, including the trauma team leader, surgical team (general, thoracic, orthopedic, and neurosurgery), and intensivist.
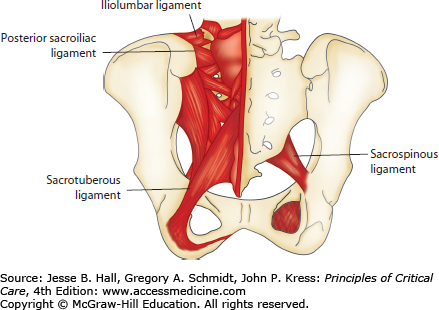
The pelvis is composed of the two innominate bones (hemipelvis) and the sacrum joined anteriorly by the pubic symphysis and posteriorly by the anterior and posterior sacroiliac ligaments, as well as the interosseous sacroiliac ligaments. Within the pelvic floor, the pelvis is further reinforced by the sacrospinous and sacrotuberous ligaments, as well as the muscles and fascia of the pelvic floor (Fig. 121-1).
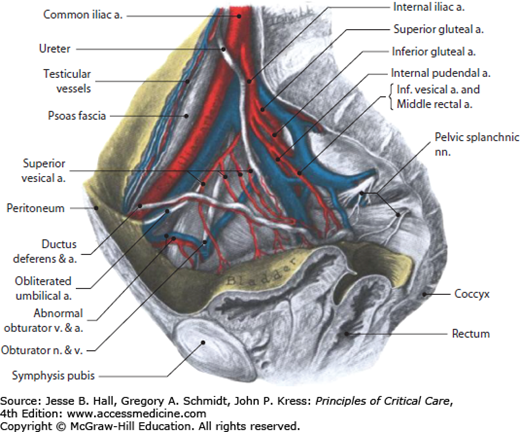
Running over the sacral ala and into the pelvis are the common iliac artery and vein, bifurcating to the external and internal iliac vessels above and below the pelvic brim, respectively. These vessels run close to the innominate bones, thus making them vulnerable to injury with any disruption of the pelvic ring. In particular, there is a plexus of veins running along the walls of true pelvis below the pelvic brim that is commonly disrupted by pelvic injuries, contributing to the rapid venous blood loss seen with these injuries (Fig. 121-2).
Arterial injuries are less common, however when present, account for 20% of pelvic exsanguinating deaths.5 The arteries most at risk are the internal pudendal, superior gluteal, obturator, and lateral sacral arteries, usually as they exit the pelvis or at a branching or tethering point within the pelvis.
The bladder lies directly behind the pubic symphysis, with the urethra exiting inferiorly, making both these structures vulnerable to injury. Similarly, the sigmoid colon and rectum are vulnerable as they run along the posterior pelvis and through the pelvic floor.
The lumbar and lumbosacral plexi composed of the ventral nerve roots also lay against the posterior pelvis, and the resulting peripheral nerves, particularly the sciatic nerve, can be injured as they exit the pelvis. The sacral nerve roots are particularly vulnerable with injuries that involve a fracture through the sacral foramen.
The mechanism of injury is an important part of the presenting history in that it can be used to predict what type of pelvic injury has been sustained, as well as the pattern of associated head, thoracic, abdominal, and extremity injuries.2 For example, in motor vehicle crashes, side impacts are more likely to result in a pelvic ring injury than a frontal impact.6 Associated injuries that can be expected with a side impact include a closed head injury, cervical spine injury, rib fractures with pneumo- or hemothorax, splenic or liver laceration, lateral compression pelvic injury, and ipsilateral extremity fractures. A fall from a height has a pattern of injury including closed head injury, shearing injuries of the great vessels in the thorax, spinal burst fractures, vertical shear injuries of the pelvis, femoral neck fractures, and other lower-extremity fractures.
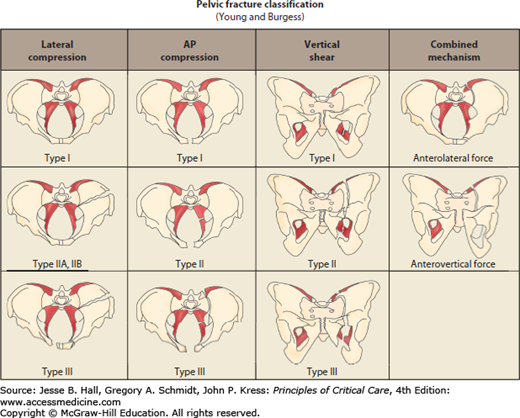
Several pelvic fracture classifications exist to assist in deciding the appropriate treatment. The Young-Burgess classification stratifies the injury first by mechanism, that is, anteroposterior compression (APC), lateral compression (LC), vertical shear (VS), and combined, and then subclassifies by severity of injury (Fig. 121-3). Higher grades of injury within each mechanistic subclass usually require operative fixation. The Tile classification stratifies the injury first by instability, that is, stable (A), rotationally unstable only (B), and vertically and rotationally unstable (C), and then subclassifies by pattern of injury (Table 121-2). Type B and C injuries usually require operative fixation. Both these commonly used classification systems have their merit, in that they communicate information about the pattern of injury, functional stability, and appropriate treatment.
Tile Classification of Pelvic Fractures
| Type A—stable |
| A1 Avulsion fractures |
| A2 Isolated fractures of the iliac wing, undisplaced ring fractures |
| A3 Transverse fractures of the sacrum and coccyx |
| Type B—vertically stable, rotationally unstable |
| B1 Open book injury |
| B2 Lateral compression injury |
| B3 Bilateral partially stable injuries |
| Type C—vertically and rotationally unstable |
| C1 Fracture of the ilium |
| C2 Fracture or fracture dislocation of the sacroiliac joint |
| C3 Fracture of the sacrum |
Acetabular fractures are not uncommon in association with pelvic fractures. For the most part, they are also associated with similar visceral injuries as pelvic fractures. The classification system is descriptive in nature and can also be used to predict concomitant injuries.
A pelvic ring injury is suspected if there is any visible swelling, ecchymosis, or compound wounds around the pelvis. Scrotal or labial swelling and ecchymosis, that is, bleeding from the urethral meatus, vagina, or rectum, are also good clinical signs of pelvic injury (Fig. 121-4). Obvious rotational deformity or shortening of the lower extremities may also be indicative of injury.
Physical examination of the pelvis includes manual palpation for tenderness anywhere around the pelvic ring. Next, the clinical stability is tested by anterior compression of the pelvis at the anterosuperior iliac spines, followed by lateral compression of the iliac wings. Any gross pelvic motion that is felt indicates an unstable pelvic ring injury.
The peripheral pulses are palpated, and a detailed neurologic examination of the lower extremities should be recorded to document the baseline function and to determine whether any neurologic dysfunction is related to peripheral nerve versus nerve root involvement.
The routine anteroposterior (AP) pelvis film obtained during the advanced trauma life support (ATLS) resuscitation is adequate to correctly identify 90% of pelvic ring injuries.7 Virtually any clinically relevant pelvic instability can be identified (Fig. 121-5). Indicators of instability include greater than 5 mm of displacement of the posterior elements in any plane and greater than 2.5 cm of widening of the pubic symphysis, avulsion fractures of the ischial spines or tuberosities, and avulsion fractures of the L5 transverse process. Additional inlet and outlet radiographs are helpful to assess AP displacement and superior migration of the hemipelvis, respectively.
For sacral fractures and subtle sacroiliac joint disruptions, the CT scan can further delineate fracture displacement.
The most important aspect of management of the patient with a pelvic ring injury is the systemic resuscitation of hypovolemic shock as per the ATLS protocol.8 During the circulatory assessment, the presence of other thoracic, abdominal, or extremity sources of blood loss should be ruled out. Massive fluid replacement, including transfusions, may be necessary.
Initial stabilization of the pelvis is important to minimize or decrease bleeding from the pelvis and to stabilize intrapelvic vascular clots.9,10 Historically, military antishock trousers (MAST) were used for this, but they have been found to contribute to decreased ventilatory ability and lower-extremity compartment syndrome.11 Recently, it has been shown that simply wrapping and tying a sheet around the pelvis can effectively provide initial provisional stability12 (Fig. 121-4). A variety of commercially available pelvic binders can be used to this effect, providing easier adjustment of compression and removal for access to the anterior pelvis. Alternatively, a two-pin anterior external fixator or the pelvic C-clamp can be applied quickly to the anterior pelvis in the emergency room and provide adequate stability (Fig. 121-6). Caution should be exercised in using the pelvic C-clamp posteriorly because improper pin placement can easily result in visceral, neurologic, or arterial injury. There is a greater margin of safety if the technique is applied using fluoroscopic assistance.13,14
The next priority is the identification and treatment of all significant sources of bleeding. If the patient is responding to the fluid resuscitation and becomes hemodynamically stable, other imaging, such as contrast-enhanced CT scanning, can be used to further delineate other sources of blood loss. An intrapelvic contrast blush on contrast CT can identify an arterial pelvic bleed.15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree