| Expected gestational age at appearance (wks) | β-hCG level (mIU/mL) | |||
|---|---|---|---|---|
| Transabdominal | Endovaginal | |||
| IUP | Gestational sac | 5.5–6 | 4.5–5 | >2,000 |
 | Yolk sac | 6–6.5 | 5–5.5 | 7,000 |
| Fetal pole | 7 | 5.5–6 | 11,000 | |
| Cardiac activity | 7 | 6 | ||
| Fetal parts | >8 | 8 | ||
In addition to the assessment of vaginal bleeding and abdominal pain in early pregnancy, the emergency physician may occasionally be called upon to perform sonographic evaluations of patients in their second or third trimester. The differential diagnosis for vaginal bleeding and abdominal pain changes during this crucial period and largely consists of placenta previa and placental abruption. It is highly recommended that an obstetrician perform the evaluation of symptomatic pregnant patients of greater than 20 weeks gestational age, since the fetus may be viable. Understandably, many practitioners work in remote or austere environments where an immediate obstetrics consultation is not available. In addition, many children’s hospitals do not have an obstetrics service immediately available. Therefore, learning to identify these clinical entities is an important skill for emergency physicians, depending on their region or scope of practice.
This chapter reviews the indications for pelvic ultrasonography in the pregnant patient. The techniques for the evaluation, including the transvaginal and transabdominal approaches, are reviewed. It is important to recognize the limitations of ultrasonography in evaluating the pregnant adolescent patient and in diagnosing an IUP. Readers are encouraged to explore the topic further to enhance their knowledge and comfort level with the use of ultrasound in the evaluation of the complicated pregnant patient.
Background
Point-of-care pelvic ultrasonography has become part of the standard workup for a pregnant patient presenting to the emergency department. Emergency physicians have been shown to reliably and accurately be able to identify an intrauterine pregnancy. A 1997 study was the first to prospectively evaluate all first-trimester pregnancy patients for ectopic pregnancy using point-of-care ultrasound when presenting to the emergency department with complications. Durham et al. showed that point-of-care ultrasonography correlated with formal ultrasonography in 97% of patients, thereby showing that emergency physicians can perform and interpret pelvic ultrasonography with reliable and accurate results. Shortly thereafter, Dart et al. found that the presence of echogenic material seen within the endometrial cavity on point-of-care ultrasound could reliably exclude the diagnosis of a normal IUP. However, this finding did not exclude the possibility of an ectopic pregnancy. The vast majority of the patients (93%) had abnormal IUPs and 5% had ectopic pregnancies. Tayal et al. investigated the outcomes of patients with first-trimester pregnancy complications and “indeterminate” emergency department ultrasounds, when an IUP was not identified. They found that there was a substantial proportion of embryonic demise (53%) and ectopic pregnancy (15%), with a low proportion of IUP as the final diagnosis. Therefore, an indeterminate pelvic ultrasound yields poor outcomes, with high rates of fetal demise and ectopic pregnancy. Recently, Wang et al. investigated indeterminate ultrasounds in conjunction with a “discriminatory zone” for β-hCG. Using a discriminatory zone of 3,000 mIU/mL yielded a sensitivity of only 35% and specificity of 58% for ectopic pregnancy. The overall sensitivity and specificity for detection of an IUP was 71% and 99%, respectively. Therefore, when point-of-care ultrasonography does not demonstrate an IUP, β-hCG levels are not reliable in differentiating an IUP from an ectopic pregnancy. Overall, Stein et al. performed a meta-analysis showing that point-of-care ultrasonography has a pooled sensitivity of 99.3% and negative predictive value of 99.96%. As a result, point-of-care pelvic ultrasonography is a reliable screening tool, with the visualization of an IUP being sufficient to rule out an ectopic pregnancy. To date, there have been no lawsuits against emergency physicians resulting directly from performance of or incorrect interpretation of point-of-care pelvic ultrasounds. The only identified lawsuit was for failure to perform a pelvic point-of-care sonogram in a patient who had a ruptured ectopic pregnancy a few days later.
Additional components of pelvic ultrasonography in the emergency department include the evaluation of the fetal heart rate and gestational age in order to determine fetal viability and the possibility of miscarriage or spontaneous abortion. In 2000, Choi et al. sought to determine the outcome of pregnancies that had documented fetal heartbeats on first-trimester transvaginal ultrasonography. Previously, the obstetrics literature reported a 90% delivery of normal, full term infants among patients with first-trimester complications who had an ultrasound finding of a fetal heartbeat documented at their presentation. In contrast, in the higher-risk emergency department population, they ultimately found that 23% of the pregnancies were non-viable and only 77% were viable and carried to full-term delivery. Recently, Saul et al. showed that emergency physicians can accurately perform a gestational age measurement. When compared with formal ultrasound studies (by radiologists), the median discrepancy was only two days, with a correlation coefficient of 0.978. In 2012, Mallin et al. performed the first prospective evaluation of emergency department patients with a documented IUP and fetal heart tones. The spontaneous abortion rate of 14.8% is consistent with previously reported rates. This information may help to guide the clinician and give some prognostic information to patients.
Thus far, there is no specific research to be found on the use of point-of-care ultrasound examination in pregnant adolescent patients. A recent study showed that pelvic ultrasonography performed by emergency medicine or pediatric emergency medicine physicians reduced lengths of stay. However, the burgeoning art of point-of-care ultrasound has yielded peer-reviewed research on the use of ultrasound for pregnant patients in the emergency department in general, and the results of these studies may be carefully applied to the adolescent population.
Embryology and anatomy
It is important to recognize the normal anatomy of the uterus and ovaries, and their relationship to the iliac vessels and bladder (Figure 13.1).
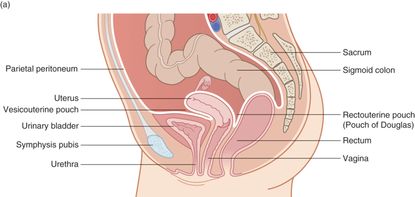
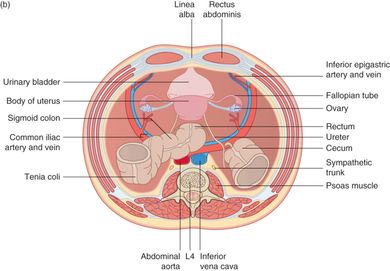
Figure 13.1 Anatomy of the female pelvis. Note the uterus and ovaries and their relationship to the iliac vessels. (a) Median section of the pelvic contents. Note the relationship between the uterus, bladder, and rectum. (b) Transverse section of the pelvic contents. Note the orientation of the uterus, ovaries, bladder, and rectum. Artwork created by Emily Evans © Cambridge University Press.
The common convention when referring to pregnancy age is to count from the first day of the last menstrual period (LMP). Ovulation occurs approximately 14 days after the LMP (two weeks of gestational age), and fertilization of the oocyte must occur within 24 hours of this event. Once the spermatocyte and oocyte fuse, they become a zygote. During the week following fertilization, the early zygote transforms into a ball of 16 cells, known as the morula, as it travels down the fallopian tube (Figure 13.2). The morula proceeds to develop into the blastocyst, a structure containing an outer ring of trophoblast cells and an inner cell mass, which are destined to become the placenta and embryonic stem cells, respectively. The blastocyst implants into the maternal endometrium approximately seven days after fertilization (three weeks of gestational age). After implantation, the embryo begins to produce β-hCG. By four weeks of gestational age, many home urine pregnancy tests, which measure β-hCG, may be positive. The embryo continues to develop and differentiate the major organs until the end of the 11th gestational week, at which time the pregnancy becomes known as a fetus.
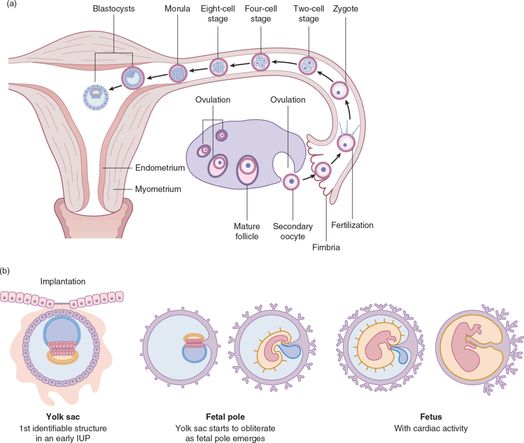
Figure 13.2 Embryologic structures. (a) Illustration depicting path of an egg from fertilization to implantation. (b) The development of embryologic structures: a yolk sac is the first identifiable form of an intrauterine pregnancy, followed by the fetal pole, and finally the fetus with cardiac activity. Artwork created by Emily Evans © Cambridge University Press.
The structure to develop first includes the gestational sac, which appears at approximately four weeks of gestational age. The endometrium changes as a result of the influence of progesterone and creates a “double decidual sign,” which is the apposition of the decidualized endometrium layer against the outer layer of the gestational sac. It is important to recognize that the decidual sign may be present in ectopic pregnancies, in which case it represents a pseudo-gestational sac. The first embryologic structure to appear within the gestational sac is the yolk sac. This is the first reliable indicator of an IUP. The next structure to appear is the fetal pole. Initially it is juxtaposed next to the yolk sac but, as the pregnancy progresses, it can appear connected to the yolk sac by a linear structure known as the vitelline duct. The amniotic sac may be seen as a separate membrane around the embryonic structure at approximately six weeks of gestation. By 14 to16 weeks of gestational age, the amniotic sac has grown to fill the entire chorionic cavity and no longer appears as a separate membrane. It is helpful to recognize at what gestational age one can expect certain embryonic structures to appear, and when they can be visualized by both transabdominal and transvaginal ultrasonography (Table 13.1).
Technique
The first sonographic approach to a patient should always be transabdominal. If the transabdominal examination yields the required information, then the more invasive transvaginal examination is not necessary. However, if the transabdominal approach does not unequivocally reveal an IUP, then the practitioner should perform a transvaginal examination. A particularly useful sequence for the performance of obstetric ultrasound in the emergency setting is to first perform the transabdominal examination while the patient is supine with a filled bladder. Next, the patient is asked to void her bladder, as the examination table and the ultrasound machine are prepared for the transvaginal examination. The practitioner then performs a speculum and bimanual examination, followed by the transvaginal sonographic examination, if required.
Imaging in the late second and third trimesters is almost exclusively performed via the transabdominal approach. Many emergency departments will triage pregnant patients with an estimated gestational age greater than 20 weeks and apparent obstetric complaints such as vaginal bleeding, cramping, or decreased fetal movement, directly to the labor and delivery ward. However, some small or remote community settings may not have immediate obstetric consultation available, in which case the emergency physician may be called upon to evaluate second- and third-trimester patients. As such, there are several conditions that present later in pregnancy that emergency clinicians should be aware of and trained to evaluate if necessary.
Point-of-care questions
Transabdominal
Transducer selection and orientation: transabdominal
For the transabdominal examination, a low-frequency (2–5 MHz) curvilinear or phased-array transducer is best used, since it provides the necessary penetration to evaluate abdominal structures (Figure 13.3). As in most abdominal ultrasound examinations, it is important to visualize the structures of interest in two planes in order to get a three-dimensional understanding of structures in space. The initial placement of the transducer is in the suprapubic region of the abdomen. In the transverse view, the indicator will be oriented to the right side of the patient (Figure 13.4a), while in the sagittal abdominal view it will be oriented towards the patient’s head (Figure 13.5a). For scanning in later pregnancy, the transducer is swept across the abdomen until the structures of interest (placenta, fetal heart, etc.) are visualized and identified.

Figure 13.3 Low-frequency transducers utilized for the transabdominal pelvic ultrasound examination.
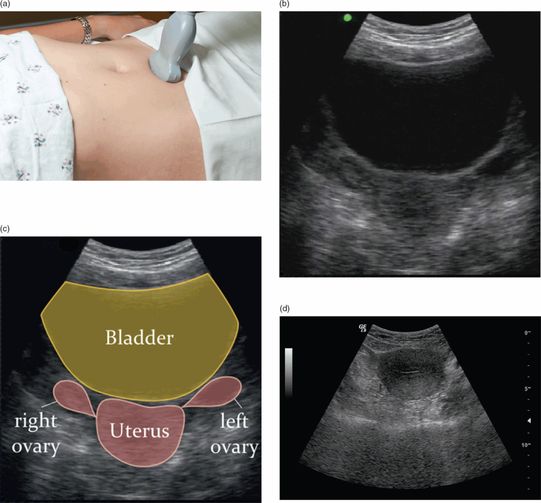
Figure 13.4 Transabdominal pelvis imaging, transverse view. (a) Transducer placement, with the indicator towards the patient’s right side. (b) Ultrasound image of the transverse pelvic view. (c) Illustration of the structures visualized in the ultrasound image: uterus, bladder, and ovaries. Illustration by Laura Berg, MD. (d) Ultrasound image of the transverse view or cross-section of the uterus itself.
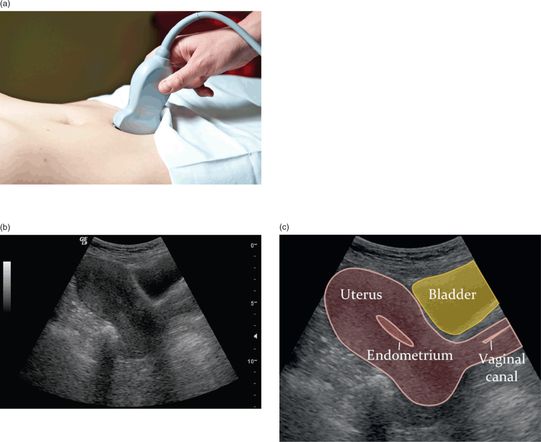
Figure 13.5 Transabdominal pelvis imaging, sagittal view. (a) Transducer placement, with the indicator towards the patient’s head. (b) Ultrasound image of the sagittal pelvic view. (c) Illustration of the structures visualized in the ultrasound image: uterus and bladder. Illustration by Laura Berg, MD.
Patient position and preparation: transabdominal
For the transabdominal examination, a full bladder can aid in the visualization of the uterus and ovaries by providing an acoustic window. The patient should be in a supine position or with slight reverse Trendelenburg position for better visualization of free fluid in the pelvis for the transabdominal portion of the examination.
Ultrasound imaging: transabdominal
It is important to recognize key structures on the normal transabdominal pelvic ultrasound. In the transverse view, the bladder appears as an anechoic rectangular or trapezoidal structure. The uterus and ovaries are located posterior, or deep to the bladder (Figure 13.4b). On the sagittal view, the bladder appears as a wedge. The uterus is to the left of the bladder (Figure 13.5b). It is important to have the patient with a full bladder, since it will act as an acoustic window to better visualize the uterus and ovaries.
Transvaginal
Transducer selection and orientation: transvaginal
The endovaginal probe (Figure 13.6) is a high-frequency (5–9 MHz) transducer that provides higher-resolution images for superficial structures. The transvaginal approach allows for near immediate approximation of the transducer against the uterus, so the depth of essential anatomic structures is rarely an issue in the first trimester. In addition to providing a more detailed view of the uterus, it allows for clearer imaging of the ovaries as there is no intervening bowel gas and the transducer is in closer proximity to the ovaries.

Figure 13.6 Endovaginal, or endocavitary, probe, 5–9 MHz is used to perform the transvaginal ultrasound exaimation. The higher frequency allows for high resolution of structures in near proximity to the transducer, such as the ovaries and uterus. Note the indicator on the transducer handle.
The endovaginal transducer requires special preparation given its use within the vagina. A moisture impermeable cover must be placed over the transducer. A layer of gel is needed within the probe cover: a layer of sterile gel is also needed on the outside of the probe cover (Figure 13.7). It is crucial to eliminate as many bubbles as possible between the transducer and the cover in order to obtain adequate images. Otherwise, the air will cause bright ring-down artifacts through sectors of the image. Additionally, the cleaning and disinfecting of the endovaginal transducer requires a well-thought-out and institutionally approved infection control plan, as the transducer can come into contact with many sexually transmitted microbes. Once the probe cover is removed and discarded, the transducer is washed with water and/or soap and then soaked in or wiped with a disinfecting agent e.g. Cidex®, according to machine-specific manufacturer recommendations.
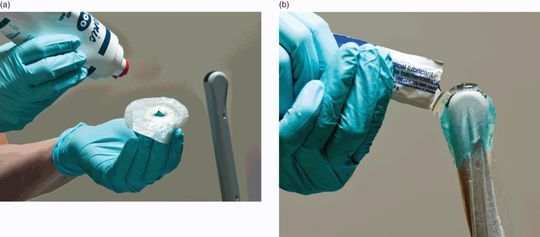
Figure 13.7 Endocavitary probe preparation. Proper preparation of the endocavitary probe is required in order to perform the transvaginal ultrasound examination. Note that the gel is placed (a) inside and (b) sterile lubricant on the outside of the probe cover, in order to allow for conduction of the sound waves.
The orientation of the endocavitary probe may at first seem complex to the novice sonographer. As the transducer is introduced into the vaginal orifice, the indicator should be pointing “up” towards the ceiling to produce a sagittal view through the uterus (Figure 13.8a). At the same time, the index finger “trigger” grip is in the 6 o’clock position. The transducer is then fanned from right to left in order to locate the uterus, which is not always a midline structure. This transducer orientation allows for easier localization of the uterus within the pelvis and is performed first. Next the transducer is rotated 90° counterclockwise, such that the indicator is now oriented towards the patient’s right side (Figure 13.9a); the index finger “trigger” is oriented towards the patient’s left side. This transducer position is commonly referred to as the transverse position but, anatomically speaking, is actually a coronal view of the pelvis.

Figure 13.8 Transvaginal pelvis imaging, sagittal view. (a) Transducer placement, with the indicator towards the ceiling in a 12 o’clock orientation. (b) Ilustration depicting how the sagittal orientation of the endovaginal probe in the pelvis results in the anterior aspect of the patient on the left of the monitor screen and the more caudal structures being located near the bottom of the image. Note the hyperechoic endometrial stripe within the myometrium. Additionally, trace free fluid is noted in the rectouterine space. Illustration by Tony Berger, MD. (c) Sagittal transvaginal view of the uterus. (d) Illustration depicting the transvaginal sagittal image of the uterus. Illustration by Laura Berg, MD.
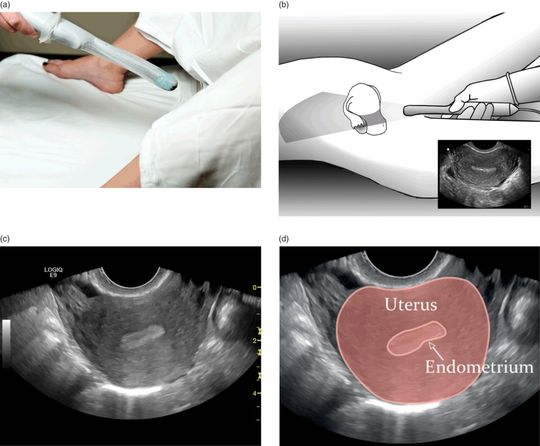
Figure 13.9 Transvaginal pelvis imaging, coronal view. (a) The indicator is rotated towards the patient’s right side in order to obtain a coronal view of the pelvis. (b) Illustration depicting how the transverse orientation of the endovaginal probe results in the structures on the right side of the patient being located on the left side of the image. More caudal structures are located at the bottom of the image. Illustration by Tony Berger, MD. (c) Transvaginal coronal image of the uterus. A clear endometrial stripe is seen without any gestational sac or other evidence of IUP. (d) Illustration depicting the transvaginal coronal image of the uterus. Illustration by Laura Berg, MD.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








