Pediatric Cervical Spine Injuries
Shauna Jain MD, FRCPC
INTRODUCTION
Maintain a high index of suspicion for spinal cord injuries.
Especially important in multiply injured patient.
Hemodynamic and other life-threatening injuries take priority.
Avoid unnecessary manipulation of the spine.
Children are a challenge to assess and treat as they are:
Not able to communicate location of pain or neurologic symptoms.
Difficult to restrain if agitated or frightened.
Immobilize and limit movement by:
Having parent at their side.
Using distraction techniques.
Removing the hard board as soon as possible.
Administering adequate analgesia.
Investigation of cord injuries in children requires knowledge of:
Specific differences between the adult and pediatric spine.
Differences in injury patterns.
Anatomic variants and radiographic characteristics.
EPIDEMIOLOGY OF PEDIATRIC C-SPINE INJURIES
The majority of spinal injury (60-80%) occurs in the cervical spine.1
The major cause for pediatric spinal injuries is motor vehicle accidents, followed by falls and child abuse.2
Goals of spinal injury treatment are to prevent secondary injury by3:
Maintaining a high index of suspicion.
Immobilization of the C-spine.
Minimizing spinal manipulation.
Ensuring the patient’s hemodynamic stability and oxygenation.
ANATOMIC CONSIDERATIONS
By 8 years of age the spine becomes anatomically similar to the adult spinal column.
Age differences of C-spine injury location and type:
Children <14 years tend to have higher C-spine injuries (C1-C4).
Children <10 years tend to have dislocations and Spinal Cord Injury without Radiologic Abnormality-type (SCIWORA)-type injuries and injury patterns.
Children >10 years tend to have fractures.1
Children are prone to dislocation and SCIWORA injuries because of the pediatric spine’s greater mobility from weaker neck musculature, larger headbody ratio, greater ligament and joint capsule laxity, anterior vertebral wedging, underdeveloped uncinate processes, and horizontal articulating facet joints.1,4
Congenital spinal abnormalities, such as atlantoaxial instability in trisomy 21 and Klippel-Feil syndrome, and bony weaknesses such as os odontoideum and block vertebra, place these children at greater risk for spinal injury.4
SPINAL STABILIZATION
Indications for C-Spine Stabilization
A high index of suspicion for spinal cord injury is always necessary.
When in doubt, immobilization is always the appropriate choice.
Pedestrian or cyclist hit by a vehicle at >30 km/hr.
Passengers in motor vehicle collisions occurring at >60 km/hr.
Serious injury of other occupants of the vehicle.
Patient thrown from a vehicle.
Fall from more than 3 meters.
Patient kicked by a horse or a fall from a horse.
Being backed over by a car.
Being thrown over the handlebars of a bicycle.
Thrown by electric shock.
Neck pain or neurologic symptoms at any time after the injury.
Neck tenderness.
Neurologic deficit.
Unexplained hypotension or bradycardia.
Acute torticollis after trauma.
Evidence of major trauma from other significant injuries.
Keys to Immobilization of Children:
Proper immobilization involves:
A fitting semirigid cervical collar and fixation to a spinal board.
Ensuring the collar is appropriately and properly fitted.
Children <3 years of age: May use sandbags on either side of the child’s head.
Fixation to the spinal boards:15
Children have large heads relative to their bodies, causing their heads to flex.
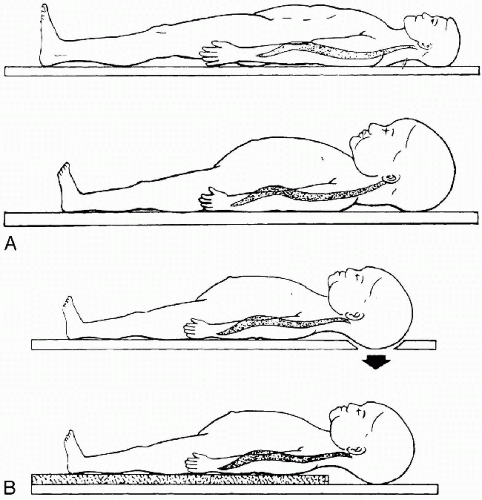
For neutral alignment: Elevate the torso with padding or recess the occiput through a hole in the spinal board (Fig. 9-1).
Proper alignment is when the external auditory canal is in line with the shoulders.
Use tape straps across the forehead, shoulders, pelvis, and thighs (Fig. 9-2).
Do not tape across the chest as this may restrict respiratory movement.
Ensure patient is off backboard within 2 hours to prevent pressure sores.
THE C-SPINE AND THE AIRWAY
See Chapter 3 on Airway Management for details.
Proper airway alignment MUST be maintained at all times.
During intubation ONE person must maintain the cervical spine in neutral alignment.
When intubation is difficult, bagging with 100% oxygen is an acceptable and preferred alternative.
It may be necessary to use a jaw thrust or an oral airway to ensure airway patency.
Never force the neck out of neutral alignment.
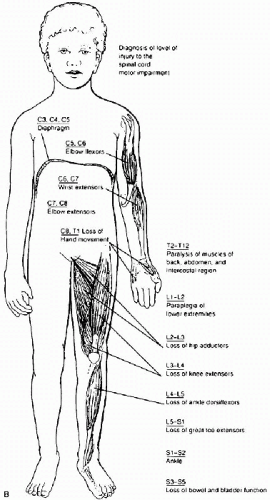
A high C-spine injury may result in diaphragmatic (C3-C5) or intercostal muscle paralysis leading to respiratory failure.
These patients require intubation to provide adequate respirations.
CLINICAL ASSESSMENT FOR SPINAL INJURY
Ensure a complete neurologic exam.
Look for evidence of spinal cord injury, including an exam of the spinal cord tracts:
Corticospinal tract:
Lies posterolaterally in the cord.
Controls ipsilateral motor function.
Tested by examination of muscle strength (voluntary or involuntary to a painful stimulus).
Spinothalamic tract:
Lies anterolaterally in the cord.
Responsible for contralateral pain and temperature sensation.
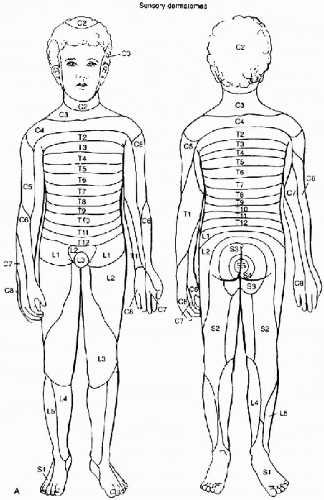
Test by checking sensation to pinprick, temperature, and light touch in all dermatomes.
Posterior columns:
Lie posterior in the cord.
Control proprioception and vibration sense.
Tested by position sense and vibration of fingers and toes.
Clinically, the neurologic level is determined from the major dermatomes and myotomes (Fig. 9-3).
Complete versus incomplete lesions:
A complete spinal injury implies no motor or sensory function below a certain level.
With an incomplete spinal injury, some motor or sensory function is preserved with possible sacral sparing (loss of all motor and sensory function below a certain nerve root level but sensation persists perianally).
Spinal shock occurs when injury to the spinal cord causes it to temporarily lose function below the level of injury.
Results in flaccidity and areflexia.
Return of the bulbocavernous reflex signals resolution of the spinal shock state, patients generally recover within 24 hours.21
Incomplete spinal cord lesions:
Spinal cord injury may follow certain clinical patterns that may be useful in identifying the type and location of injury.
1 Central cord syndrome:
Typically after hyperextension injury.
Injury to anterior spinal artery which supplies the central cord.
Clinically see motor loss greater in upper extremities than lower extremities.
2 Anterior cord syndrome:
Anterior spinal injury causing anterior cord infarction.
Paraplegia and loss of pain and temperature sense below affected sensory level but preserved posterior column function (position and vibration sense).
3 Brown-Séquard syndrome:
Hemisection injury to the cord.
Ipsilateral corticospinal and posterior column loss (motor, vibration, and proprioception) and contralateral spinothalamic (pain and temperature) injury one to two levels below the motor loss.
SPECIFIC PEDIATRIC SPINAL INJURIES
SCIWORA (Spinal Cord Injury Without Radiologic Abnormality)
Particularly seen in younger children and cervical spine injuries.6
Bony radiologic imaging is normal but underlying cord injury may have occurred.1
Pediatric spinal column can stretch more than the spinal cord.
In cadaver neonates, the spinal column would stretch by 2 cm but the cervical cord would only stretch by ¼ inch before there was spinal injury.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree