Fig. 18.1
Increased uptake lower left thyroid consistent with parathyroid adenoma
Patient #2: History of High Calcium
Following the administration of 24 mCi of Tc99m sestamibi injected intravenously, immediate and delayed imaging of the head, neck, and upper chest were obtained in the anterior projection.
The impression of abnormal sestamibi scan demonstrated persistent activity in the projection of the inferior right thyroid. A prior ultrasound demonstrated a hypoechoic nodule in the right inferior thyroid lobe (Fig. 18.2).
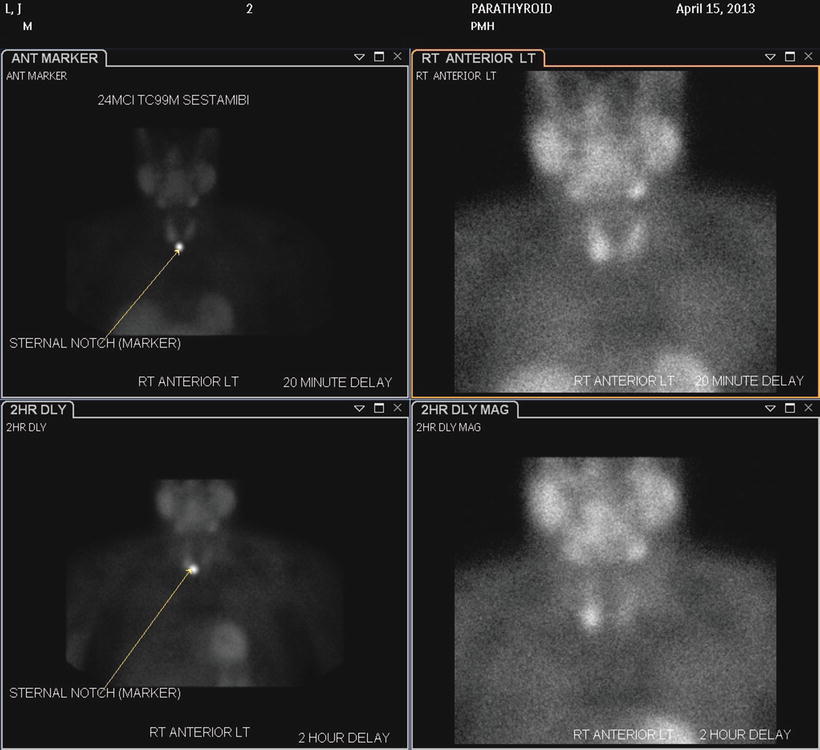
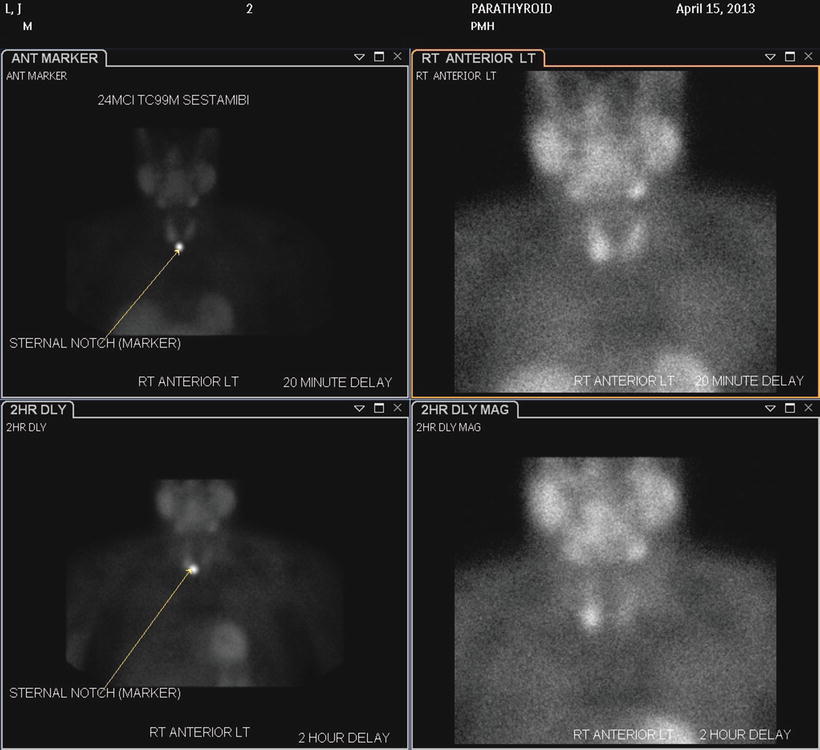
Fig. 18.2
Increased uptake lower right thyroid consistent with parathyroid adenoma
Operative Procedure
A 5–6 cm low collar incision is made two finger-breadths above the suprasternal notch and deepened through the cervical fascia and platysma. The strap muscles are carefully separated in the midline and care is taken to avoid injury to the anterior jugular veins (Figs. 18.3 and 18.4).
Fig. 18.3
The incision is 5–6 cm in length and two finger-breadths above the suprasternal notch
Fig. 18.4
The strap muscles are gently separated taking care not to injure the anterior jugular vein
After separating the strap muscles in the midline, the soft tissues around the thyroid are gently dissected using a stroking motion. The middle thyroid veins are double clipped and divided. The thyroid gland is grasped gently and elevated. The recurrent laryngeal nerve is found in the tracheoesophageal groove and the middle thyroid artery is noted and may be superficial or deep to the recurrent laryngeal nerve.
The superior parathyroid is present adjacent to the gland 80 % of the time. It is much more reliable in its position on the superior aspect of the thyroid gland.
The inferior parathyroid, however, is more variable with some reports noting up to 42 % variation in the location of the inferior glands. A careful inspection on the surface is done and if not found then a careful dissection inferiorly of the tissue beneath the thyroid dissecting down to the thymus and into the anterior mediastinum may be done.
In gently massaging an area suspected of containing the inferior gland and then obtaining a rapid PTH assay is one technique for localization of the gland. Most parathyroid surgeons have carried out many thyroid operations and understand the need for a meticulous and purposeful dissection. The anatomy on the left side proves to be much easier to find the recurrent laryngeal nerve in the tracheal esophageal groove than the right side. A focused dissection of the parathyroid gland is done based upon the preoperative sestamibi scan (Fig. 18.5).
Fig. 18.5
(Left) The soft tissues around the thyroid are dissected and the middle thyroid veins are clipped and divided. The thyroid is grasped, elevated, and retracted to the midline to expose the tracheoesophageal groove
The right side, however, is localized in much the same manner by dividing the middle thyroid veins and gently dissecting the thyroid gland toward the midline. Careful Kittner dissection to expose the recurrent laryngeal nerve traveling vertically and the horizontal thyroid artery is done (Fig. 18.6). Occasionally it is necessary to dissect the thymus and expose the surface of that gland in order to identify the mediastinal parathyroid.
Fig. 18.6
(Right) Retract the right thyroid lobe to expose and ligate the middle thyroid veins. The right recurrent laryngeal nerve usually ascends in a groove between the esophagus and larynx
The actual removal of the adenoma should be done with direct vision by dividing the artery on the proximal side of the adenoma. Careful exposure of the recurrent laryngeal nerve and its relationship to the middle thyroid artery is mandatory to avoid injury.
Although the upper parathyroids on the left and right are more predictable in their location, occasionally one of these may be hidden in the carotid sheath. The carotid sheath can be easily opened with hemostat dissection and superior lateral retraction. This dissection can be carried upward toward the pharynx.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








