PANCREATITIS
CASE SCENARIO
A 54-year-old man with no past medical history presents to the emergency department with 24 hours of abdominal pain. The pain started the day prior to presentation in the epigastrium and is still most intense there, but also radiates to the back. He denies similar episodes in the past. In addition to his pain, he has suffered three episodes of non-bloody, non-bilious vomiting. He takes no medications. He consumes approximately 15 alcoholic beverages per week, mostly on the weekends, and admits to 9 drinks on the day prior to symptom onset.
The patient is afebrile, his heart rate is 115 beats per minute, and other vital signs are normal. He is uncomfortable lying in bed and has diffuse mild abdominal tenderness, with the most severe tenderness in the epigastrium. His laboratory evaluation is notable for a white blood cell count of 12, an amylase of 1500 U/L, and a lipase of 780 U/L.
EPIDEMIOLOGY
Acute pancreatitis is the most common gastrointestinal disorder requiring hospitalization in the United States, and its incidence appears to be increasing.1 In the United States, cases are evenly distributed between men and women, although alcohol is more commonly the cause in men and gallstones are more commonly the inciting factor in women. The incidence rises with increasing age, although the greatest number of cases occur in patients in the fifth or sixth decade of life. Pancreatitis affects black patients 2 to 3 times more frequently than the white population.1,2
The most common causes of pancreatitis are ethanol ingestion and gallstones. Less frequent causes include instrumentation of the bile or pancreatic ducts (endoscopic retrograde cholangiopancreatography [ERCP]), medications (especially diuretics, anti-epileptics, and protease inhibitors), hypertriglyceridemia, hypercalcemia, congenital anatomic or genetic conditions (e.g., pancreas divisum or cystic fibrosis transmembrane receptor [CFTR] mutation), mumps, pancreatic neoplasm, autoimmune disease, and trauma or hypoperfusion. In 10% to 15% of cases a cause is not identified.
Chronic pancreatitis has an incidence rate 15% to 30% that of acute pancreatitis.3 While the incidence of acute pancreatitis continues to increase with age, chronic pancreatitis incidence plateaus in middle age. Like acute pancreatitis, it is more common in blacks than in whites. The most important risk factors are alcohol use and smoking, but a range of genetic mutations (such as in CFTR and SPINK-1), autoimmune conditions, and environmental stimuli may be important contributors.4
Most acute pancreatitis is mild and self-limited. Approximately 20% of patients develop some degree of necrosis of the pancreatic parenchyma. Of these, about 30% develop infected pancreatic necrosis requiring intervention. The overall mortality is 2% to 4%.5
PATHOPHYSIOLOGY
The pathophysiology of acute pancreatitis is poorly understood. Among patients with risk factors (heavy alcohol use, gallstones, hypercalcemia, etc.), only a minority develops acute pancreatitis over a lifetime, and the factors differentiating these patients from those who never develop the disease is unknown. As previously described, the most common causes of acute pancreatitis can be broken down into mechanical (gallstones, ERCP) or systemic (alcohol, medications, hypercalcemia, hypertriglyceridemia). There are two suggested mechanisms whereby the mechanical causes result in acute pancreatitis: obstruction of the ampulla, or bile reflux into the pancreatic ductal system. How various systemic agents trigger acute pancreatitis is unclear.
Most investigators agree that, whatever the inciting mechanism, acute pancreatitis is caused by activation of trypsin within the pancreatic acinar cells. The pancreas has mechanisms for preventing intracellular trypsin activation and counteracting low levels of activation, but when these mechanisms are overwhelmed, pancreatic autodigestion ensues, which can progress beyond the gland itself and into the surrounding peripancreatic tissues. This local injury can in turn activate a variety of systemic inflammatory mediators (complement, interleukins, phospholipase A2), which may precipitate the systemic effects seen in severe acute pancreatitis.5
Chronic pancreatitis is a progressive inflammatory disease of the pancreas resulting in fibrosis and calcification of the gland. The exact mechanisms are unclear, and, as above, its perpetuation probably depends on interaction between a variety of environmental and genetic factors. As with acute pancreatitis, intrapancreatic trypsin activation may play a role in inciting inflammation. Once chronic inflammation is under way, large- and small-duct obstruction due to calcification, which increases pressure within the pancreatic ductal system, may be responsible for the persistent pain.6
CLINICAL PRESENTATION
Acute pancreatitis typically presents with epigastric abdominal pain that radiates to the back. Classically the pain is more abrupt in onset with gallstone pancreatitis than with other etiologies. This is usually accompanied by nausea and vomiting. On examination, the abdomen is usually at least mildly distended and tenderness may be diffuse, although a careful examination will show the point of maximum tenderness to be in the epigastrium. Of note, acute pancreatitis is one of the most common “nonsurgical” causes of peritonitis. Jaundice may be present if there is persistent biliary obstruction.
Other associated signs and symptoms are related to systemic inflammation and correlate with the severity of disease. Dyspnea may be related to pleural effusions, abdominal distension, or the acute respiratory distress syndrome. Tachycardia, hypotension, and oliguria arise from the systemic inflammatory response and resulting fluid sequestration. They may be absent in mild pancreatitis, and marked in more severe cases.5
Pain is also the primary symptom of chronic pancreatitis. Early in the course of disease it may occur in discrete attacks, but typically becomes chronic and more continuous. A minority of patients do not have significant pain, but present instead with endocrine or exocrine insufficiency.
DIFFERENTIAL DIAGNOSIS
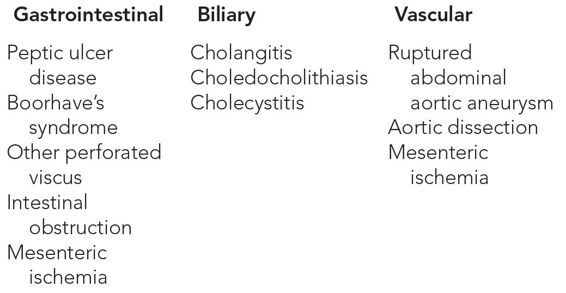
See Table 14–1.
WORKUP AND CHOICE OF IMAGING
The diagnosis of acute pancreatitis is based on the identification of two of the following three criteria: (1) clinical—upper abdominal pain, often with associated nausea and vomiting; (2) laboratory—serum amylase or lipase greater than three times the upper limit of normal; (3) radiographic—imaging (usually computed tomography [CT] or magnetic resonance imaging [MRI], possibly ultrasound) characteristic of acute pancreatitis. Imaging is rarely required to make the diagnosis of acute pancreatitis, which can usually be made on the basis of clinical and biochemical parameters alone.7
The etiology for pancreatitis should be sought to guide prevention of recurrent episodes. When there is no obvious inciting factor such as heavy alcohol use or recent ERCP, abdominal ultrasound should be performed to evaluate for gallstones as a potential cause.
CT remains the standard imaging modality for acute pancreatitis, but is probably overused. As mentioned previously, it is rarely required for diagnosis, although it may be useful in equivocal cases, to assess other possible entities in the differential diagnosis, or in the critically ill patient when clinical signs and symptoms cannot be elicited. Its most important role is in diagnosing and defining the extent of pancreatic and peripancreatic necrosis and identifying other local complications. This is seldom relevant at the time of presentation, since necrosis typically progresses for 3 to 5 days after the onset of pancreatitis, and other local complications such as pseudoaneurysm, venous thrombosis, and organized or infected necrosis occur later in the course of disease. Since early CT seldom alters management, does not enhance prognostic data, and has the disadvantages of cost, radiation exposure, and nephrotoxicity, it should be used selectively early in the course of acute pancreatitis.7
In contrast, axial imaging with CT or MRI is indispensible later in the course of severe disease. These studies with intravenous contrast can identify the most important complications of acute pancreatitis, including necrosis, pseudoanerysm, peripancreatic fluid collections, splenic vein thrombosis, and pseudocyst. Such imaging is absolutely essential when planning intervention for any of these entities.7
Chronic pancreatitis must be suspected on clinical grounds. Serum pancreatic enzyme measurement is not useful for diagnosis. Glucose intolerance suggests endocrine dysfunction, and steatorrhea suggests exocrine dysfunction. Calcifications are seen on plain abdominal x-ray in 30% of patients. Ultrasound, CT, and MRI can all show calcifications and ductal dilation. MRI with magnetic resonance cholangiopancreatography (MRCP) may be the most versatile test due to excellent resolution of the ductal anatomy without radiation exposure.8
IMAGING FINDINGS
 Ultrasound
Ultrasound
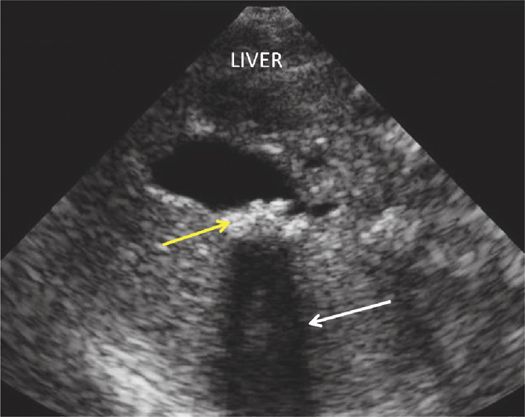
Ultrasound is primarily used to investigate for gallstones, although it may also help to diagnose pancreatitis. Gallstones are seen as echogenic foci with acoustic shadowing; they are frequently dependent (Figure 14–1). Biliary sludge is a microprecipitate mixture of bile, cholesterol crystals, and calcium bilirubinate that forms when bile becomes supersaturated, but has not formed discrete stones. It is not important to distinguish between gallstones and sludge as they are managed identically. Ultrasound has a sensitivity and specificity of 85% and 99%, respectively, for detection of gallstones, but is highly operator dependent.
Figure 14–1 Right upper quadrant ultrasound showing cholelithiasis. Gallstones appear as echogenic, dependent foci (yellow arrow) with acoustic shadowing (white arrow).
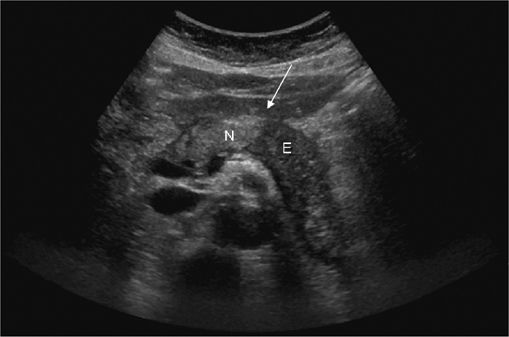
Ultrasound may also show a diffusely enlarged and hypoechoic pancreas when there is acute pancreatitis, but the sensitivity and specificity are poor (Figure 14–2). Peripancreatic fluid or ascites can also be identified (Table 14–2).
Figure 14–2 Ultrasound of acute pancreatitis. Arrow shows line of demarcation between normal pancreatic head (N) and edematous pancreatic tail (E).