Chapter 72 Pain Management in The Intensive Care Unit
3 How can pain be assessed in critically ill patients?
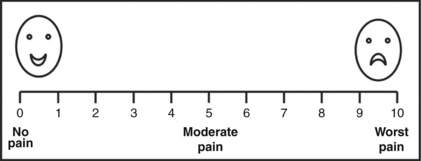
Pain should be assessed and documented at regular intervals. Pain is a subjective experience and is most reliably measured by using a subjective scale such as the numeric rating scale (Fig. 72-1), which can be employed in patients as young as 5 years. Younger patients’ pain is assessed by using the faces scale (Fig. 72-1), which is a modified visual analog scale. In patients unable to communicate, reliance on objective measures (physiologic or behavioral) becomes necessary. Whereas use of physiologic measures (blood pressure, heart rate, tearing, diaphoresis, mydriasis) can cause underreporting and overreporting of pain, use of behavioral measures such as observation of facial expression has been demonstrated to correlate with subjective reporting.
5 What are the treatment options for a critically ill patient in pain?
 Nonpharmacologic treatment of pain includes proper positioning of patients, stabilization of fractures, elimination of irritating physical stimulation, and environmental modification to promote comfort. Because sleep deprivation as well as anxiety and delirium may diminish the pain threshold, it is important to minimize stimuli that can disturb the normal diurnal sleep pattern (noise, artificial light) and treat anxiety and delirium promptly.
Nonpharmacologic treatment of pain includes proper positioning of patients, stabilization of fractures, elimination of irritating physical stimulation, and environmental modification to promote comfort. Because sleep deprivation as well as anxiety and delirium may diminish the pain threshold, it is important to minimize stimuli that can disturb the normal diurnal sleep pattern (noise, artificial light) and treat anxiety and delirium promptly.
 Pharmacologic treatment of pain works by inhibition of the release of local mediators in damaged tissue (nonsteroidal antiinflammatory drugs [NSAIDS], acetaminophen), blocking nerve conduction (regional anesthesia), or altering pain neurotransmission in the central nervous system (opioids, acetaminophen, ketamine, dexmedetomidine).
Pharmacologic treatment of pain works by inhibition of the release of local mediators in damaged tissue (nonsteroidal antiinflammatory drugs [NSAIDS], acetaminophen), blocking nerve conduction (regional anesthesia), or altering pain neurotransmission in the central nervous system (opioids, acetaminophen, ketamine, dexmedetomidine).
7 Which opioids are recommended for routine administration in ICU patients?
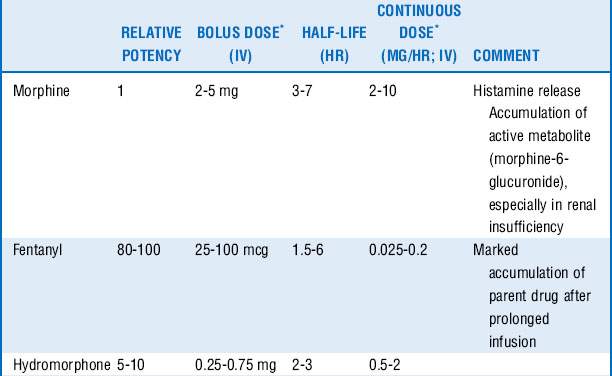
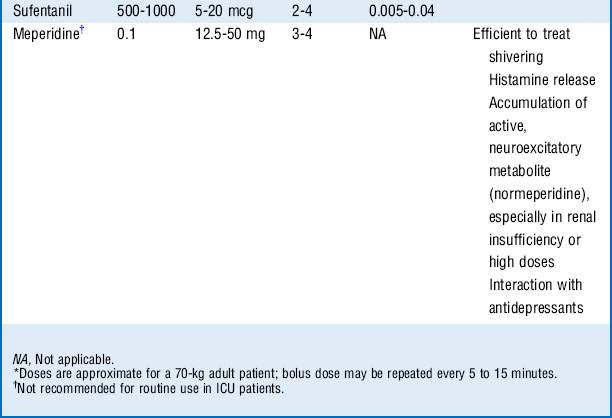
Morphine, fentanyl, hydromorphone, and sufentanil are the analgesic agents most commonly used and recommended in the ICU (Table 72-1).
8 How do you decide which opioid to use?
 Morphine is a naturally occurring, relatively hydrophilic opioid with a long clinical history and therefore familiarity with its use. The onset of action is slow (effect site equilibration time 15-30 minutes), and duration of action is 2 to 4 hours. However, it has relatively rapid hepatic clearance and tends not to accumulate because of its water solubility, which limits the volume of distribution, although glucuronide metabolites with sedative-analgesic properties may accumulate in the setting of renal insufficiency.
Morphine is a naturally occurring, relatively hydrophilic opioid with a long clinical history and therefore familiarity with its use. The onset of action is slow (effect site equilibration time 15-30 minutes), and duration of action is 2 to 4 hours. However, it has relatively rapid hepatic clearance and tends not to accumulate because of its water solubility, which limits the volume of distribution, although glucuronide metabolites with sedative-analgesic properties may accumulate in the setting of renal insufficiency.
 Fentanyl is a synthetic, potent, and highly lipid-soluble opioid. The lipid solubility is responsible for the rapid onset of action (effect site equilibration time 1-3 minutes). This makes it a preferable analgesic in the acutely distressed patient. Fentanyl has a short duration of action (30-45 minutes after one bolus); however, repeated dosing may cause accumulation and prolonged action (long context-sensitive half-life). Cardiovascular side effects are minimal.
Fentanyl is a synthetic, potent, and highly lipid-soluble opioid. The lipid solubility is responsible for the rapid onset of action (effect site equilibration time 1-3 minutes). This makes it a preferable analgesic in the acutely distressed patient. Fentanyl has a short duration of action (30-45 minutes after one bolus); however, repeated dosing may cause accumulation and prolonged action (long context-sensitive half-life). Cardiovascular side effects are minimal.
 Hydromorphone is a semisynthetic opioid that is approximately 10 times more potent than morphine and has lipid solubility between those of morphine and fentanyl. Compared with morphine, its onset and duration of action are slightly shorter (effect site equilibration time 10-20 minutes, duration of action 1-3 hours). There is less histamine release and greater hemodynamic stability, and there is no clinically significant active metabolite.
Hydromorphone is a semisynthetic opioid that is approximately 10 times more potent than morphine and has lipid solubility between those of morphine and fentanyl. Compared with morphine, its onset and duration of action are slightly shorter (effect site equilibration time 10-20 minutes, duration of action 1-3 hours). There is less histamine release and greater hemodynamic stability, and there is no clinically significant active metabolite.
 Sufentanil is a synthetic, highly lipid-soluble opioid with high selectivity for the μ-receptor. It has been shown to cause less respiratory depression compared with other opioids; thus it may be preferred in patients with spontaneous ventilation. Sufentanil accumulates less compared with fentanyl (shorter context-sensitive half-life).
Sufentanil is a synthetic, highly lipid-soluble opioid with high selectivity for the μ-receptor. It has been shown to cause less respiratory depression compared with other opioids; thus it may be preferred in patients with spontaneous ventilation. Sufentanil accumulates less compared with fentanyl (shorter context-sensitive half-life).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree