ACUTE PAIN MANAGEMENT
Acute pain = pain that occurs as direct result of tissue damage, <3 mos in duration
• Can occur as a result of trauma, surgical insult, labor, infection, or inflammation
• Acute postoperative pain → inflammation is a major cause
Treatment
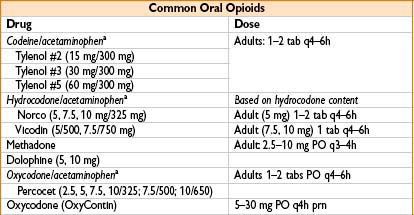
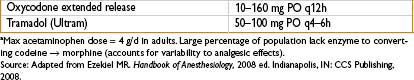
• Includes opioid & nonopioid meds
• Opioids commonly used—can be given parenterally, helpful immediately postop
Opioid Rotation
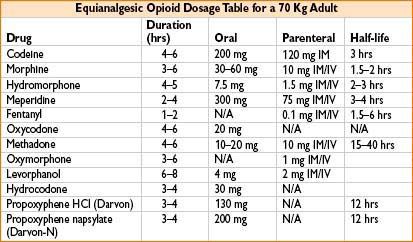
• Definition: Using different opioids interchangeably & via different routes
• Presence of major organ dz (liver/kidney dysfx) can markedly ↓ dose required for adequate clinical response
• Lack of complete cross tolerance between different opioids
→ Essential to use lower than equianalgesic doses
• Oral & parenteral doses often dissimilar (due to pharmacokinetic differences)
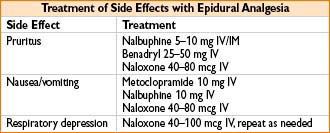
• Opioid-associated itching: Dilute naloxone & benadryl → can both be used
• Naloxone 400 mcg in 1 L of LR or NS given at 75 mL/hr
• Avoid benadryl in advanced age


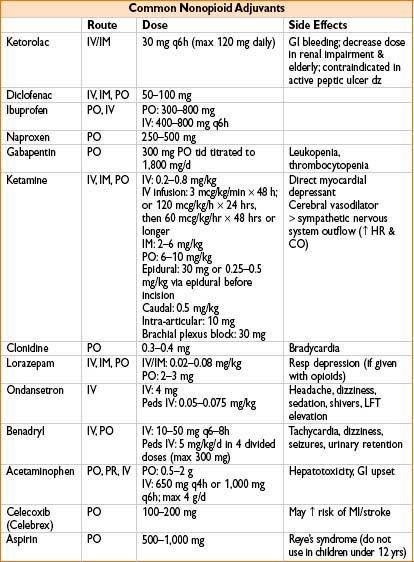
MULTIMODAL APPROACH TO PAIN CONTROL (ALSO SEE CHAPTER 27)
Analgesic Delivery Systems
• PO
• Not optimal for immediate postop pain (delayed time to peak effect)
• Opioids commonly combined with COX inhibitors
• SC/IM
• Less desirable routes (pain on injection & erratic absorption)
• Cyclical period of sedation → analgesia → inadequate analgesia common
• Intravenous administration
• Requires close respiratory monitoring
• Common in PACU, ICU, & specialized units
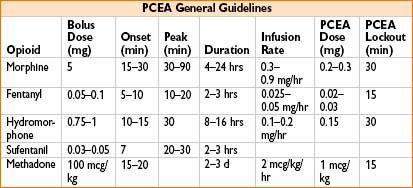
• Patient-controlled analgesia (PCA)
• Allows pt to self-administer opioids with button push
• Physician specifies dose, minimum time period between doses (lockout), basal infusion rate, max delivered dose

Neuraxial Analgesia
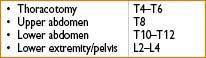
• Intrathecal or epidural routes; effective for postop pain after abd, pelvic, thoracic, & orthopedic surgeries of lower extremity
• Opioid infusions often combined with local anesthetics (bupivacaine, lidocaine, ropivacaine)
• Clonidine & buprenorphine also used epidurally
Epidural Opioids
• Site of action = pre- & postsynaptic receptors in dorsal horn substantia gelatinosa
• Opioid drugs enter CSF at rate dependent on physicochemical properties
• Molecular weight, pKa, oil:water solubility
• Direct transport via spinal cord blood supply can occur
• Diffusion through dural cuff regions to spinal cord can occur
• Lipid-soluble opioids (sufentanil, fentanyl) enter spinal cord faster
• Also eliminated faster by vascular uptake, leading to a short duration of action
• Morphine = water-soluble opioid (slower action onset, longer duration of action)

Epidural Clonidine
• Dose = 3–5 mcg/kg; can be added to epidural mix (local or opioid)
• Prolongs duration of epidural local anesthetic by ≈50%
• ↓ epidural opioid requirements ≈30%
• Side effects: Severe bradycardia (if used >1 mcg/kg/hr)
Epidural Placement Levels
Signs of an Inadequate Epidural
• Pain at rest & with movement (pain score >5)
• Tachycardia
• ↑ respiratory rate
• For thoracic & abd cases
→ Inability to breathe deeply, cough, use incentive spirometer
Testing of Epidurals
• 2% lidocaine with 1:200,000 epinephrine or 0.25% bupivacaine with 1: 200,000 epinephrine
• Give 3 mL of either via epidural → check BP, motor block & pain relief
• May repeat 3 mL after 3–5 min
• Consider replacing epidural if no pain relief after 8 mL of test dose over 10 min
“Splitting” Epidural with IV PCA
• Technique: Add IV PCA in addition to epidural infusion (must simultaneously remove opioids from epidural infusion)
• May be necessary for
• Pt with opioid dependence
• Incomplete incisional coverage from epidural
• Upper & lower body surgeries (trauma victims)
• Large surgical incision
• Lower level epidural catheter placement
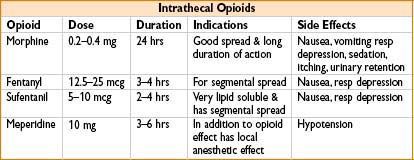
Intrathecal Opioids
• Act on substantia gelatinosa of the spinal cord
• Potent analgesia due to central localization of receptors
• Side effects are mediated by mu receptors (in brain & brainstem)
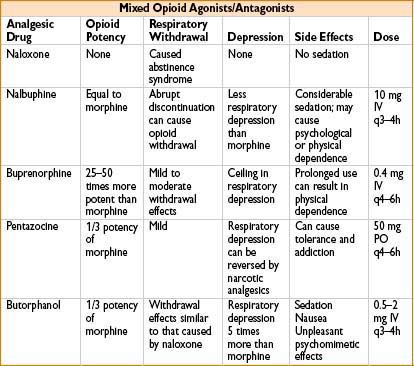
Mixed Agonists/Antagonists
• Block effects of high doses of morphine-like drugs
• By competing with morphine-like drugs to bind to mu opioid receptor
• Produce partial agonist effects at κ (kappa) and/or δ (delta) opioid receptors
< div class='tao-gold-member'>









