Chapter 4 Pain
INTRODUCTION
Headache and neck pain are extremely common and the ability to influence the pain symptom is a major aspect of treatment. Massage can be an extremely effective option for pain management, used either as a supportive treatment in conjunction with other treatments as described in Chapter 3, or as a primary treatment method.
WHAT IS PAIN?
Pain is caused by the stimulation of nociceptors. These receptors are usually stimulated by chemicals such as substance P, bradykinin, and histamine, which excite the nerve endings. Pain is elicited by three different classes of stimuli: mechanical, chemical, and thermal. Soft tissue pain is caused by the chemicals released from illness, injury, or from mechanical irritation caused by cumulative stress, microinflammation, or extreme heat or cold. Emotional or psychological stress, called autonomic disturbances, can trigger pain by causing an increase in motor tone of muscles – changes in fascial tone and shifts in fluid flow affecting oxygen and nutrient delivery and waste removal.
ORIGINS AND CLASSIFICATION OF PAIN
• Acute pain is an appropriate response to injury or illness. It is easy to control with short-term use of medication, ice, heat, or counterirritants (i.e., medical-based ointments).
• Chronic pain is an inappropriate and ongoing perception of pain. It can be managed with careful use of medication but is best addressed using a multidisciplinary approach supporting lifestyle changes from dependency and side effects.
• Intractable pain is dominant and very hard to control.
• Phantom pain is experienced in an area of amputation.
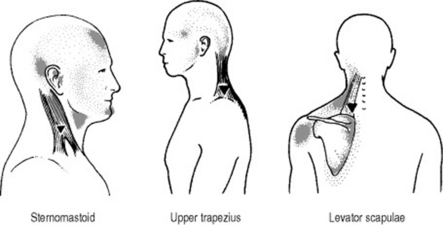
• Referred pain is when an organ or other tissue projects pain sensation to another area of the body. Trigger point pain is a type of referred pain (Figures 4.1 and 4.2).
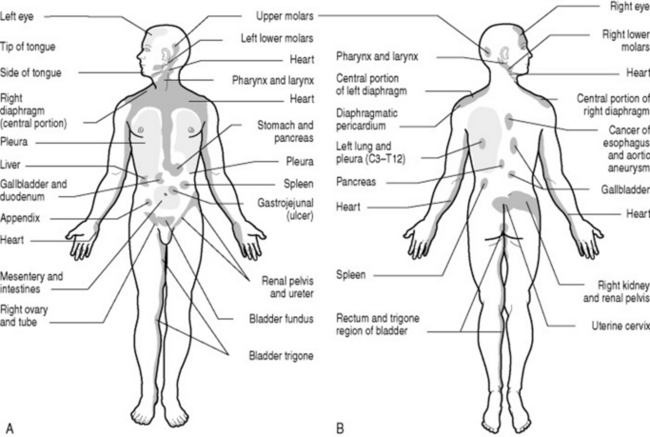
Figure 4.1 Pain referred from viscera. A: Anterior view. B: Posterior view.
(Adapted from Rothstein et al 1991.)
Peripheral nerves
There are millions of nociceptors in the skin, bones, joints and muscles, and in the protective membranes around the internal organs. Nociceptors are concentrated in areas more prone to injury, such as the fingers and toes. There may be as many as 1300 nociceptors in just 1 square inch of skin. Skin stimulation during massage that is intense enough to stimulate the ‘good hurt’ response causes the nociceptors to fire. This is one of the mechanisms of counterirritation. This is also a major component of massage benefits for pain management.
When nociceptors detect a harmful stimulus, they relay their pain messages in the form of electrical impulses along a peripheral nerve to the spinal cord and brain. Sensations of severe pain are transmitted almost instantaneously. Dull, aching pain – such as an upset stomach, earache, or joint aching – is relayed on fibers that transmit at a slower speed.
Spinal cord
Nerve cells in the spinal cord also release chemicals such as endorphins that diminish or substance P that amplifies the strength of a pain signal that reaches the brain for interpretation. Massage appears to influence these chemical responses, although research has not yet identified the exact mechanism (see Chapter 5).