CHAPTER 35
Otitis Media, Acute
Presentation
In acute otitis media (AOM), adults and older children will complain of ear pain. There may or may not be accompanying symptoms of upper respiratory tract infection. In the younger child or infant, parents may report irritability, decreased appetite, and sleeplessness, with or without fever or pulling at the ears. The real diagnosis comes not from symptoms or history but from tympanic membrane (TM) findings (Figures 35-1 and 35-2). The TM may show marked redness, but contrary to what many clinicians were taught during training, erythema of the TM is the least specific finding for AOM.
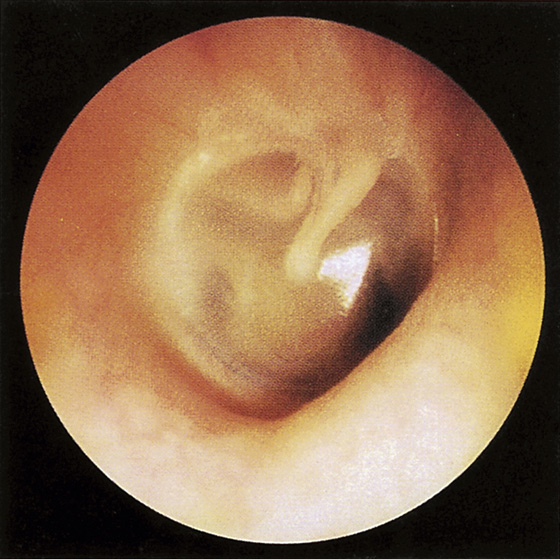
Figure 35-1 Normal right tympanic membrane and middle ear. (From Meniscus Educational Institute: Otitis media: management strategies for the 21st century. Bala Cynwyd, Pa, 1998.)
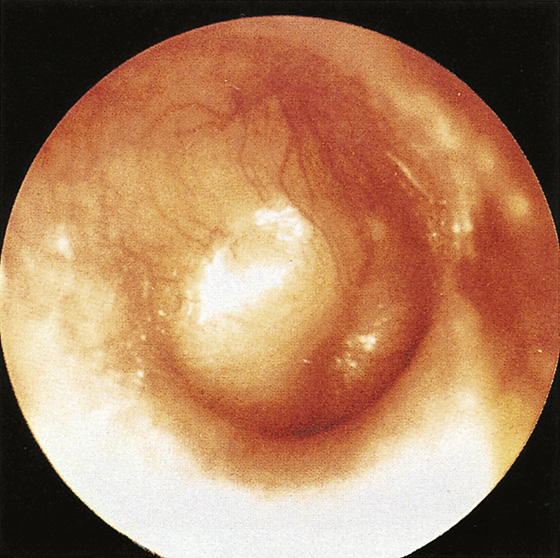
Figure 35-2 Bulging right tympanic membrane in acute otitis media. (From Meniscus Educational Institute: Otitis media: management strategies for the 21st century. Bala Cynwyd, Pa, 1998.)
Expanding middle-ear effusion volume and intense inflammation produce the key TM findings that are essential for an AOM diagnosis. These findings point to fullness or a bulging TM, with decreased clarity of the bony landmarks and decreased mobility on pneumatic otoscopy. A normal TM snaps briskly like a sail filling with air from a sudden breeze. With fluid behind the TM, there will be either sluggish or no movement at all. A diagnosis of AOM also can be established if the TM has perforated and acute purulent otorrhea is present that is not attributable to otitis externa (see Chapter 34).
Note that increased vascularity or erythema is not sufficient to diagnose AOM but does strengthen the diagnosis by providing the identification of possible TM inflammation. Keep in mind that a child’s vigorous crying is a common cause of an erythematous TM that otherwise has normal findings. Therefore, under these circumstances, avoid diagnosing AOM if erythema of the TM is the only finding suggesting AOM.
What To Do:
 Investigate for any other underlying illness. When clinical evidence of AOM is obscure or absent, consider other sources of ear pain, such as dental or oral disease, temporomandibular joint dysfunction, or disorders of the mastoid, pharynx, or larynx.
Investigate for any other underlying illness. When clinical evidence of AOM is obscure or absent, consider other sources of ear pain, such as dental or oral disease, temporomandibular joint dysfunction, or disorders of the mastoid, pharynx, or larynx.
 There are many antibiotics available for the treatment of AOM. Amoxicillin remains the treatment of choice according to the guidelines of the American Academy of Pediatrics, based on efficacy, palatability, side-effect profile, and cost. High-dose amoxicillin at 80 mg/kg/day dosed bid provides better coverage of resistant organisms than standard 40 mg/kg/day dosing. Amoxicillin should not be used if
There are many antibiotics available for the treatment of AOM. Amoxicillin remains the treatment of choice according to the guidelines of the American Academy of Pediatrics, based on efficacy, palatability, side-effect profile, and cost. High-dose amoxicillin at 80 mg/kg/day dosed bid provides better coverage of resistant organisms than standard 40 mg/kg/day dosing. Amoxicillin should not be used if
(1) There has been treatment failure with amoxicillin in the past 30 days.
(2) Concurrent purulent conjunctivitis is present (usually caused by Haemophilus influenzae).
(3) The patients are already on chronic suppressive therapy with amoxicillin.
 For those patients in whom an alternative to amoxicillin is needed and there is no penicillin allergy, choices include amoxicillin-clavulanate (Augmentin) 90 mg/kg/day dosed bid (maximum dose 3 g/day), Cefpodoxime 10 mg/kg dosed once daily (maximum dose 800 mg/day), or Cefuroxime 30 mg/kg/day dosed bid (maximum dose 1 g/day).
For those patients in whom an alternative to amoxicillin is needed and there is no penicillin allergy, choices include amoxicillin-clavulanate (Augmentin) 90 mg/kg/day dosed bid (maximum dose 3 g/day), Cefpodoxime 10 mg/kg dosed once daily (maximum dose 800 mg/day), or Cefuroxime 30 mg/kg/day dosed bid (maximum dose 1 g/day).
 For patients allergic to penicillin, the best choice is erythromycin plus sulfisoxazole (Pediazole) 75 mg/kg/day of the erythromycin component dosed qid (maximum dose 2 g erythromycin component). Azithromycin and trimethoprim-sulfamethoxazole have significant problems with resistance.
For patients allergic to penicillin, the best choice is erythromycin plus sulfisoxazole (Pediazole) 75 mg/kg/day of the erythromycin component dosed qid (maximum dose 2 g erythromycin component). Azithromycin and trimethoprim-sulfamethoxazole have significant problems with resistance.
 Studies suggest that 10 days of oral therapy for AOM is more effective than shorter courses in children less than 2 years of age. After 2 years of age, consideration may be given to shorter courses of 5 to 7 days.
Studies suggest that 10 days of oral therapy for AOM is more effective than shorter courses in children less than 2 years of age. After 2 years of age, consideration may be given to shorter courses of 5 to 7 days.
 Ceftriaxone (Rocephin) can be used in a dose of 50 mg/kg IM once daily for 1 to 3 days when compliance problems are anticipated. A three-dose regimen of IM ceftriaxone may be more efficacious than a single dose for patients with nonresponsive AOM.
Ceftriaxone (Rocephin) can be used in a dose of 50 mg/kg IM once daily for 1 to 3 days when compliance problems are anticipated. A three-dose regimen of IM ceftriaxone may be more efficacious than a single dose for patients with nonresponsive AOM.
 When there is reliable follow-up and the parents are responsible, mild cases of AOM may be treated initially with analgesics alone, adding antimicrobials as an option if symptoms persist or worsen. All children younger than 6 months and all those with moderate to severe ear pain and fever greater than 39° C in the past 24 hours, bilateral disease or otorrhea, should be treated immediately.
When there is reliable follow-up and the parents are responsible, mild cases of AOM may be treated initially with analgesics alone, adding antimicrobials as an option if symptoms persist or worsen. All children younger than 6 months and all those with moderate to severe ear pain and fever greater than 39° C in the past 24 hours, bilateral disease or otorrhea, should be treated immediately.
 Parents can be very satisfied with a wait-and-see approach, in which an antibiotic is prescribed, but the parents are asked to wait 72 hours before filling it. They are to have the prescription filled only if their child still has substantial ear pain or fever at that point or if he is not starting to get better. Provide follow-up by telephone or office visit within 3 days to reassess.
Parents can be very satisfied with a wait-and-see approach, in which an antibiotic is prescribed, but the parents are asked to wait 72 hours before filling it. They are to have the prescription filled only if their child still has substantial ear pain or fever at that point or if he is not starting to get better. Provide follow-up by telephone or office visit within 3 days to reassess.
 Provide pain and fever control with acetaminophen or ibuprofen elixir. Additional pain relief may be obtained using antipyrine, benzocaine, oxyquinoline, and glycerin (Auralgan Otic) drops if perforation or tympanostomy tubes are not present.
Provide pain and fever control with acetaminophen or ibuprofen elixir. Additional pain relief may be obtained using antipyrine, benzocaine, oxyquinoline, and glycerin (Auralgan Otic) drops if perforation or tympanostomy tubes are not present.
 Advise parents that pacifier use, exposure to tobacco smoke, and bottle feeding an infant in a reclining rather than an upright position all increase the risk for AOM. Daycare with more than five attendees has been shown to be the most powerful risk factor for frequent AOM. Children who have one or more parents or siblings who experienced frequent AOM or who had pressure-equalizing tubes also will often have frequent AOM or need pressure-equalizing tubes.
Advise parents that pacifier use, exposure to tobacco smoke, and bottle feeding an infant in a reclining rather than an upright position all increase the risk for AOM. Daycare with more than five attendees has been shown to be the most powerful risk factor for frequent AOM. Children who have one or more parents or siblings who experienced frequent AOM or who had pressure-equalizing tubes also will often have frequent AOM or need pressure-equalizing tubes.
 Recommend a 10-day follow-up examination for all patients younger than 2 years of age, in those cases in which the parents do not believe that the infection has resolved or the child’s symptoms persist, and when there is a family history of recurrent otitis or the accuracy of the parental observations may be in doubt.
Recommend a 10-day follow-up examination for all patients younger than 2 years of age, in those cases in which the parents do not believe that the infection has resolved or the child’s symptoms persist, and when there is a family history of recurrent otitis or the accuracy of the parental observations may be in doubt.
 Because otitis media is much less common in adults, these patients should also have follow-up in 2 weeks, with possible otolaryngologic consultation.
Because otitis media is much less common in adults, these patients should also have follow-up in 2 weeks, with possible otolaryngologic consultation.
 Middle-ear effusion will often persist after resolution of acute infection. Persistence of this effusion without symptoms does not indicate need for further antibiotics.
Middle-ear effusion will often persist after resolution of acute infection. Persistence of this effusion without symptoms does not indicate need for further antibiotics.
What Not To Do:
 Do not overlook underlying illnesses, such as meningitis.
Do not overlook underlying illnesses, such as meningitis.
 Do not prescribe antihistamines or decongestants. These drugs do not decrease the incidence or hasten the resolution of AOM. The American Academy of Pediatrics recommends that over-the-counter cough and cold medications should not be given to children younger than 2 years of age because of the risk of life-threatening side effects.
Do not prescribe antihistamines or decongestants. These drugs do not decrease the incidence or hasten the resolution of AOM. The American Academy of Pediatrics recommends that over-the-counter cough and cold medications should not be given to children younger than 2 years of age because of the risk of life-threatening side effects.
Discussion
AOM is primarily a disease of children younger than 3 years of age, although AOM is not totally unexpected up to age 5. Age-related factors that directly cause AOM are the result of immature anatomy and immature immune systems coupled with excessive exposure to pathogens. The main reasons for AOM are not bacterial, although bacteria are the final ingredients. Bacterial AOM pathogens merely take advantage of the main cause of AOM (i.e., dysfunction of the middle-ear-flushing mechanism, the eustachian tube). Eustachian tubes are dysfunctional to some degree in every young child but gradually become fully functional by age 5.
Most AOM is caused by a viral infection, and most patients do well regardless of the antibiotic chosen. Some 50% to 80% of cases of AOM will spontaneously clear without antibiotics. (Older children with infrequent AOM are more likely to experience spontaneous clearing, whereas more severe AOM or AOM occurring soon after a previous episode is less likely to clear spontaneously.) Because AOM usually occurs secondary to acute viral infections (respiratory syncytial virus, influenza, and rhinovirus), rapid initiation of antibiotic treatment may result in eradication or reduction of the susceptible organisms in both the middle-ear fluid and the nasopharynx, permitting the overgrowth of the nasopharyngeal flora organisms that are not susceptible to the drug. Because the predisposing condition (the viral infection causing ciliary and mucosal damage, plus overproduction of secretions) may still be present, a new infection of the middle ear may then take place with the newly selected resistant pathogen. Despite the increase in antimicrobial resistance of community-acquired Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis and the plethora of alternative antibiotics available, amoxicillin remains the drug of choice in the treatment of uncomplicated AOM.
Bullous myringitis is the result of acute bacterial infection of the tympanic membrane, producing intraepithelial fluid collections. These patients present with bullae on the TM and can have severe pain. They respond well to anesthetic otic drops (Auralgan), oral antibiotics, corticosteroids, and analgesia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



