Chapter 4 Other systems
Dental anaesthesia
Standards and Guidelines for General Anaesthesia for Dentistry
The Royal College of Anaesthetists 1999
Introduction
Background
Techniques
Cartwright D.P. Death in the dental chair. Anaesthesia. 1999;54:105-107.
Department of Health. General anaesthesia, sedation and resuscitation in dentistry (Poswillo Report). London: HMSO, 1990.
Flynn P.J., Strunin L. General anaesthesia for dentistry. Anaesth Intens Care Med. 2005;6:263-265.
Royal College of Anaesthetists. Standards and guidelines for general anaesthesia and dentistry. London: RCA, 1999.
Worthington L.M., Flynn P.J., Strunin L. Death in the dental chair: an avoidable catastrophe? Br J Anaesth. 1998;80:131-132.
Anaesthesia for ear, nose and throat surgery
General anaesthetic problems
Ear surgery
Nasal surgery
Throat surgery
Tonsillectomy
Extubate awake (protective reflexes), with head-down in left lateral position.
There are two approaches to induction:
Peritonsillar abscess (quinsy)
National Patient Safety Agency
Reducing the Risk of Retained Throat Packs after Surgery, April 2009
Anaesthesia and liver disease
Physiological changes in liver disease
Haematology. Anaemia, thrombocytopenia, coagulopathy.
GI. Oesophageal varices, delayed gastric emptying. Increased gastric volume and acidity.
CNS. Encephalopathy, cerebral oedema.
Pharmacokinetic and pharmacodynamic changes
Assessment of surgical risk
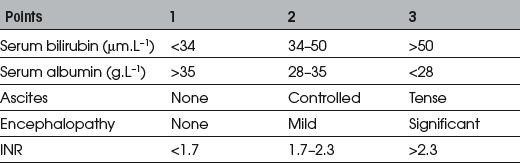
Child’s (1963) classification assessed risk using albumin and bilirubin. Modified by Pugh et al (1973) (see Table 4.1). Perioperative mortality A<5%, B≈︀25%, C>50%.
Specific drugs
Anticholinergics. Little change in pharmacokinetics. Use normal doses.
Barbiturates. Increased sensitivity and prolonged excretion of thiopentone. Use <3–4 mg/kg.
Propofol. Increased sensitivity. Use 2 mg/kg for induction.
Anticholinesterases. Normal doses of neostigmine may be used.
Fabbroni D., Bellamy M. Anaesthesia for hepatic transplantation. Contin Edu Anaesth, Crit Care Pain. 2006;6:171-175.
Hartog A., Mills G. Anaesthesia for hepatic resection surgery. Contin Edu Anaesth, Crit Care Pain. 2009;9:1-5.
Lai W.K., Murphy N. Management of acute liver failure. Contin Edu Anaesth, Crit Care Pain. 2004;4:40-43.
 scatter and ↑ shunting, together with impaired respiration from ascites, causing hypoxia.
scatter and ↑ shunting, together with impaired respiration from ascites, causing hypoxia.