18 Osteopathic Manipulative Medicine
A Functional Approach to Pain
“Nature applies to you the switch of pain when her mandates are disregarded, and when you feel the smarting of her switch, do not pour drugs into your stomachs, but let a skillful engineer adjust your human machine, so that every part works with Nature’s requirements.”1
History of Osteopathy
Truly an American practice of medicine, osteopathy began on June 22, 1874 in Kansas when Andrew Taylor Still, MD “flung to the breeze the banner of osteopathy”1 and “like an explorer trimmed [his] sail…”.1 A.T. Still was born in 1828 in Jonesboro, Virginia, but he grew up in Missouri as the son of a Methodist minister. Many stories surround the early years of Dr. Still, but little historical evidence is documented. As a Methodist minister, his father was a “circuit rider,” a preacher who would travel out to the edges of the frontier, settle his family, and provide religious service to the pioneers of that day. Although he would also do some missionary work to the indigenous people, conversion was rarely successful. Young Andrew was known to have spoken with the Native Americans around his father’s settlement and was said to have learned about the practice of herbal medicine from them. He was also known to have taken some skeletal remains from the burial grounds and with them began his study of anatomy. As he grew older and the debate around slave states and free states grew, he was a noted abolitionist and later joined the Kansas militia as sides were taken in the early days of the Civil War.
Following his tour of duty in the Kansas militia, he returned home and began the study of medicine as it was practiced in the late 1800s. Practices such as bleeding, administration of purgatives and cathartics, including arsenic and mercury, were common and considered standard of care at that time. This “heroic medicine” was mainly directed at suppressing symptoms and was practiced prior to the advent of the microbial orientation of disease or the understanding of much of the pathophysiology that we take for granted today. He became an accomplished physician by apprenticeship as was the custom and was awarded the title of Medical Doctor. An important event occurred in 1864 when a meningitis outbreak took the lives of three of Still’s children. This devastated Andrew and he “blamed the gross ignorance of the medical profession for the deaths of his children.”2 This tragedy created an alarming sense of helplessness in Andrew and from then on he was determined to find better methods of healing.2
After a prolonged episode of depression and fasting, along with meditation and prayer, he came to the realization that the human form was a perfect reflection of the divinity that created it with the further realization that all of the natural elements of healing were present in the human body, and needed a physician only to release them. He reasoned that any being so created would have contained within it all of the substances it needs to heal itself and that the mechanical structure of the body must have a significant impact on its function. As Still’s most prominent quote said “To find health should be the object of the doctor. Anyone can find disease.”3 It was also the object of the physician to understand every aspect of human anatomy because it is only through understanding of anatomy that an accurate assessment of the healthy functioning of the body could be ascertained. This new science, Dr. Still called “osteopathy”, because it was the study of the relationship that the osseous structure and its interrelationships had on health. He advocated abandoning all use of drugs in favor of dietary, spiritual, and mechanical functional treatment.
Because of this growing success, A.T. Still began to attract the attention of other physicians who wanted to learn this skill that seemed to be healing those who were previously found to be beyond repair. In 1892, he started the American School of Osteopathy in Kirksville, Missouri, and began teaching the first class of 17 students, of which notably three were women. The major system of study was anatomic dissection and the study of manual therapies designed to improve the overall functioning of the human body, allowing it to move toward its natural state of health. One of these first 17 students was Arthur Hildreth, a friend of the Still family, who went on to great success and eventually wrote a book about his great teacher. In the book he says of Dr. Still: “I wish it were in my power to describe in a simple, practical way some of his most outstanding technics. Not only the methods he used but also his own individual way of explaining what he did,” also, “Dr. Still’s technique was marvelous, often beyond our comprehension. He seemed to do everything so easily we wondered how he could accomplish so much.”4 This same Dr. Hildreth was the pioneer who led the charge in many states to gain practice rights for this new method of healing called ”osteopathy”.
Principles of Osteopathic Medicine
Diagnostic Principles
Because osteopathic manipulative treatment is aimed at restoration of function, the diagnosis of dysfunction within the somatic system is a crucial starting point. As Dr. Still’s writing was ripe with concepts and barren with practice, the clarification and development of these topics is ongoing within the osteopathic profession.
The primary structural diagnosis in osteopathic manipulative medicine is “somatic dysfunction.” This is defined by the AOA glossary of terms as “impaired or altered function of related components of the somatic (body framework) system: skeletal, arthrodial, and myofascial structures and their related vascular, lymphatic, and neural elements.”5 This broad definition is important for two reasons: (1) it creates a definitive concept around a palpatory experience and (2) it extends the scope of dysfunction to a zone greater than that of the neuromusculoskeletal system, that of the visceral and cellular functioning of the human organism.
Diagnostic Process
In addition to conventional medical diagnostic procedures, palpatory examination leading to segmental diagnosis of somatic dysfunction is essential to the practice of osteopathic manipulative medicine. Typically, the process of coming to a diagnosis usually involves some measure of palpatory screen, scan, and finally, segmental definition. Screening is the process of palpation and movement designed to answer the question, “Is there a problem?” Scanning answers the question, “Where is the problem?” and segmental definition answers the question, “What is the problem?”6
The scanning examination is one that narrows the finding of somatic dysfunction to a segment, rib, or joint. This is accomplished by a more focused palpation over the region assessing changes in tissue texture that are more specific to the region involved. For instance in the thoracic spine, palpation along the zone of the transverse processes, segment by segment, will help to identify the segment that is dysfunctional, usually by noting a firmness of the surrounding tissue as compared to the segmental transverse process above and below it. This finding is then confirmed through motion testing by initiating passive side-bending or rotation in the thoracic spine and then observing the tissue response to that motion and comparing that response to motion in the segments above and below it. For example, after screening the thoracic spine and finding it to be dysfunctional, a scan is performed and the 5th thoracic segment displays increased tissue tension at the region of the transverse process when compared to the transverse processes above and below it. With the patient’s arms crossed (to eliminate unconscious external stabilization), the trunk is side-bent to the left and an assessment of ease or bind at the 5th thoracic segment is identified as compared to the segments above and below. If restriction to motion is identified with left side-bending, there will be ease to right side-bending of the thoracic spine. Typically, a restriction to motion is more easily appreciated on palpation, but conventionally, the segment is always described in its direction of ease; therefore, the 5th thoracic segment with restriction to side-bending to the left is described as “side-bent right.” The choice of side-bending as a test is completely arbitrary here and passive rotation could just as easily have been demonstrated. The findings of segmental tissue texture change and motion asymmetry determine a positive scan and the next step, segmental definition, must be accomplished if any treatment is to be considered (Fig. 18-1).
Segmental definition is the process of finely tuning one’s scan and focusing palpation and motion testing to account for all possible motion characteristics that occur at the particular segment or joint. To continue our example of the 5th thoracic vertebrae, we identified that motion ease is palpated in lateral side-bending to the right.3 Additionally, we must further check rotation right and left, flexion and extension, anterior or posterior translation, cephalad or caudad translation, or ease in response to the respiratory cycle of inhalation or exhalation. Again, this testing is done passively with the operator moving the patient in all of the aforementioned planes of motion with a palpating hand checking for tissue response to that movement. This provides the most accurate and detailed type of definition for a vertebral segment. Segmental definition of joints of the extremities is a natural extension of the scan for that region. Because motion restriction is detected asymmetrically in the extremities, that motion is more definitively described according to the major motions, but also the minor or secondary motions, such as glide and translation. While these secondary motions are significant in the vertebral column, these subtler motions in the extremities often hold the key to defining dysfunction and, hence, treating it.
Treatment
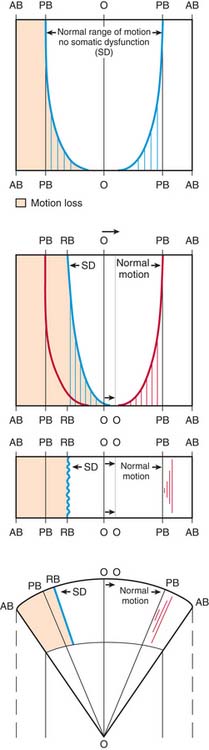
Inherent in these descriptions is the barrier concept. This much debated concept is a direct result of palpatory experience in segmental definition (Fig. 18-2). One model of the barrier concept states that there exists within any segment or joint, a neutral zone in which all of the forces that normally impinge on that segment or joint are equal and balanced. There is a zone around that neutral area that represents the entirety of the normal range of motion that segment or joint possesses. Any motion that segment or joint performs is met with increasing resistance as it approaches its endpoint of motion or barrier. Some definitions of the barrier include distinctions of motion that describe the barrier to passive motion versus the barrier to active motion, or the barrier that exists between the endpoint of passive motion and the barrier that occurs at the limitation of bony resistance of the skeleton. Another important part of the barrier concept is that of a pathologic neutral. When a joint or segment is functioning fully, its neutral position of rest is balanced within its endpoints of motion. When one of the functional endpoints of motion or barriers have been changed through dysfunction, then a new balance point is established that is still neutral in relation to its total potential of function. That change in the neutral is palpable in structural diagnosis as somatic dysfunction. The restriction to motion in one or more planes of motion creates palpatory findings that are commensurate with the definitions of dysfunction.
Muscle Energy Treatment: Lumbar
Muscle energy treatment was developed by Fred Mitchell, Sr., DO, as a way to approach problems directly without high-velocity, low-amplitude thrusting.7 This is a direct technique in which the operator moves the dysfunctional segment toward its restrictive barrier and then stabilizes it while the patient applies an isometric contraction away from the barrier. This contraction is held for 3 to 5 seconds and the patient is instructed to discontinue the contraction. At that point, the operator readjusts the position of the segment to accommodate for the muscle relaxation and lengthening that has occurred, and moves the segment into a new barrier. This sequence is repeated until maximum improvement in the segmental findings is achieved. The advantage of this technique is that the force that is applied is generated by the patient and monitored by the physician. Dr. Fred Mitchell, Jr, DO, who wrote extensively about his father’s technique, explained that the anatomy in a patient’s own (body) was more precisely and intimately known to the patient’s muscles than they could be to any examiner. For this reason he said, his father chose to use the energy of the patient’s muscles instead of his own for the corrective forces.7 This alleviates the danger or unnecessarily overzealous application of an externally applied force. Difficulties with this procedure usually surround the localization of force by the practitioner, lack of stabilization against the isometric contraction on the part of the physician, and too great a force applied by the patient. The force applied need only be great enough to engage the tissues at the level of the localized, treated segment. Too great a force can become too diffuse and difficult to localize around the segment, it may also be too strong to oppose by the physician. The treated segment must be stabilized in its position against the barrier and if that stabilization is compromised because the physician is trembling against the force of the patient, it will be impossible to maintain a stable position at the barrier. Muscle energy technique, when properly applied, should not look like a wrestling match.
The lumbar spine is identified as the lower five vertebrae resting on the sacrum. These are large vertebrae with no rib attachments. Primary motions at these segments include flexion, extension, side-bending, and rotation. The intervertebral discs support the vertebrae, providing both a cushion for shock absorption and a stable, yet flexible interface between the segments, allowing for movement. The remainder of the vertebrae include a pedicle and spinous process creating the spinal canal; transverse processes bilaterally and articular processes above and below the transverse process that create functional joints with the spinal segments superior and inferior to it. These processes form the zygapophyseal or facet joints, true synovial joints in the lumbar spine. Between the pedicles of each of the vertebral segments course the peripheral spinal nerve roots.8
Pain in the lumbar spine is common and multifactorial.9 It is beyond the scope of this chapter to discuss all of the possible causes of back pain; more importantly, there is much speculation about the true etiologies of any of these types of pain. Common pathologies occurring in the lumbar spine that can easily affect the function of the region include: osteoarthritis, herniated nucleus pulposus, inflammatory arthropathy, spondylolisthesis, spondylosis, and ligamentous strain. Although each of these problems has its unique presentation, they each have the capacity to express themselves as a functional limitation of that region, exhibiting signs of somatic dysfunction. Disruption of the normal integrity of the musculoligamentous structures of the axial spine in any location can result in muscular hypertonicity. Because this hypertonicity is usually asymmetrical and is generally restrictive in motion of the spine, diagnosis of tissue texture differences and resultant motion asymmetry is quickly identified. Important in the diagnosis of somatic dysfunction at any location is the appreciation of the anatomic and subsequent physiologic influences any dysfunction can have at local, adjacent regions or distal regions, whether by myofascial continuity or neural irritability.
Important influences that extend from lumbar dysfunction include regional influences. Lumbar dysfunction with its requisite biomechanical changes can affect segments locally adjacent. Because of the physiologic differences between the regions of the axial spine, dysfunction in the lumbar region can influence the appearance of dysfunction in the thoracic spine and sacropelvis and vice versa. As a result of normal physiologic relationships within the viscera and their relationship to the lumbar region anatomically, functions of those viscera can be affected, especially the viscera of the lower pelvis including the large intestine, sigmoid colon, rectum, and pelvic organs. Although this is partly due to the direct effect that a change in normal biomechanics can have on involuntary motions such as those associated with respiration, some of the effect is due to a reflex influence of the somatic system on the autonomic nervous system in the levels of the spine that are affected. In this case, T12 to L2 are most closely associated with the sympathetic cell bodies that provide autonomic influence to the colon below splenic flexure and other pelvic organs. In this way, osteopathic manipulative medicine extends beyond the realm of musculoskeletal pain management and becomes part of a complete system of medicine in which its application begins to influence the visceral function and ultimately the metabolic health of the organism.10 At this point the encompassing definition of “somatic dysfunction” becomes actualized in its application of treatment.
The physician grasps the opposite shoulder by placing his arm across the anterior cervical thoracic junction of the patient and holds the patient snugly. He moves the patient’s trunk passively until the position of restriction is palpated at the previously identified segmental level, which in this case means rotating her trunk to the left and side-bending to the left with lumbar extension until the force of these motions is palpated at L4. The accuracy of the localization of these forces is crucial to the effective application of these techniques (Fig. 18-3). Too little motion and the forces will be localized superior to the segmental region, too much motion and the forces will be directed at a level inferior to the dysfunctional segment. When localization is achieved, the patient is asked to attempt to side-bend and rotate away from the position that she has been put into by the physician. In this case, the patient is directed to, “gently turn to the right.” Generally, only one direction of motion is necessary to activate the force sufficiently to achieve an effect at the dysfunctional segment. Because of normal spinal mechanics, motion in one of the cardinal directions of the spine will affect motion in all the other planes where motion is engaged, so by asking the patient only to rotate, side-bending and flexion are normally engaged. The force of the isometric contraction must be palpated at the level of the dysfunctional segment. The localized isometric contraction is held for 3 to 5 seconds and then the patient is asked to stop turning, or to relax. A moment is given to appreciate the relaxation in the tissues and then the segment is moved into its next restrictive barrier, in this case, slightly further rotated left, side-bent left, and extended. This sequence is repeated as many times as it is needed to effect maximal change, but generally this occurs within five repetitions. At that point, the patient is slowly and gently returned to physiologic neutral, and the dysfunctional segment is checked again for improvement in tissue texture and motion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree