Objectives/indications
Children often present to the emergency department with orthopedic pathologies, such as bone fractures and joint effusions. Ultrasound can serve as a useful adjunct to the physical examination and radiography, in the assessment and management of pediatric orthopedic conditions. In order to identify a potential fracture or effusion, the current standard of practice is to obtain plain radiographs. If a reduction in the emergency department is necessary, either fluoroscopy or serial radiographs are utilized to confirm appropriate alignment of the reduced bone. All of these involve the exposure to ionizing radiation. However, ultrasound has the potential to decrease radiation exposure associated with the assessment and reduction of fractures.
Forearm fractures account for almost half of all pediatric fractures, with two-thirds of all forearm fractures located distally. The most common mechanism of injury is a fall on an outstretched hand, otherwise known as a “FOOSH.” Children are also more at risk for forearm fractures than adults, since they have a relatively large amount of cartilage and collagen, which reduces the tensile strength of bone. This leads to certain fractures, such as greenstick fractures and torus fractures, that are not observed in adults. In addition, the presence of growth plates (physes) can be associated with fractures that are not readily visible on initial radiographic studies. These are referred to as Salter–Harris Type I fractures. It is likely that, for this reason, investigations have focused on using ultrasound to assess forearm fractures in children. Other reported sites for assessment by ultrasonography include ankle fractures, rib fractures, clavicle fractures, and even skull fractures. There are, however, limitations with ultrasound in reliably detecting compound injuries, fractures adjacent to joints, fractures involving the small bones of the hands and feet, non-displaced epiphyseal fractures (Salter–Harris I), or small injuries with a fracture line of less than 1 mm.
In addition to identifying fractures, ultrasound guidance may be helpful for fracture reductions. Ultrasound guidance offers several potential advantages over fluoroscopy or blind reduction. Most notably, there is no ionizing radiation involved. Portable ultrasound units are smaller and easier to set up, when compared to traditional, large fluoroscopy units. Finally, repeated studies can be performed relatively quickly without involving further radiation. The use of ultrasound is especially helpful in departments that do not have access to fluoroscopy, since real-time ultrasound guidance allows for the evaluation of the adequacy of reduction, obviating the need to obtain additional radiographs, which are often required with blind reductions. This is especially helpful in austere environments and developing countries, where radiographs may be limited or unavailable.
In addition, the emergency physician often encounters a child with a potential hip or knee effusion. Hip effusions may be seen in benign conditions, such as toxic synovitis, or pathologic conditions, such as with septic arthritis. When faced with a child with a suspected hip or knee effusion, it is crucial to expeditiously evaluate the child for septic arthritis, since, when left untreated, it rapidly progresses to the destruction of cartilage. The synovial fluid should be obtained for analysis and culture, which often requires irrigation in the operating room and intravenous antibiotics. Ultrasound guidance has the potential to identify such effusions, and allow for improved success and decreased complications associated with arthrocentesis.
In this chapter, we discuss the key components of point-of-care ultrasound for orthopedic injuries: the assessment and reduction of fractures, and the identification and aspiration of joint effusions.
Fractures: assessment and reduction
Background
The literature has described point-of-care ultrasound as being an accurate modality to diagnose long-bone fractures. There have been several studies investigating forearm fractures. Chinnock et al. found similar overall success rates of ultrasound-guided distal forearm fracture reductions, when compared with traditional fracture reduction (83 vs. 80%). When compared with post-reduction radiographs, the emergency department physician-performed post-reduction ultrasound had a sensitivity of 94% and specificity of 56%. Interestingly, four patients in the traditional group required further sedation for repeat reduction, whereas there were none in the ultrasound group.
The use of point-of-care ultrasound for pediatric orthopedic emergencies is a relatively new modality, with most of the research in the emergency setting having been published within the last few years. The majority of pediatric studies have focused on utilizing ultrasound to diagnose and to guide reductions for forearm fractures, since it is the most common fracture with which children present. Point-of-care ultrasound performed by trained emergency medicine physicians is both a reliable and a convenient method to diagnose and guide the reduction of forearm fractures in children. Chen et al. found that ultrasound revealed the correct type and location of a fracture in 96% of patients. When compared with radiographs, the sensitivity and specificity for ultrasound in the detection of forearm fractures was 97% and 100% respectively. For subjects that underwent ultrasound-guided fracture reduction, 92% had adequate alignment on post-reduction radiographs after the first attempt. Due to the severity and displacement of fractures, it was unclear whether the physical examination influenced the ultrasound results. Therefore, Chaar-Alvarez et al. evaluated non-angulated distal forearm fractures. When compared with traditional radiographs, ultrasound had an overall accuracy of 94%, and a sensitivity and specificity of 96% and 93% respectively. Ultrasound was actually less painful, when compared with obtaining traditional radiographs (mean Wong-Baker FACES® score 1.7 vs. 1.2, P = 0.004).
Further studies have shown that point-of-care ultrasound for extremity long-bone injuries may be comparable to radiography for fracture identification, in predicting the need for reduction, and in assessing adequacy of reduction. Ultrasound has been used to identify occult fractures not seen on radiographs. Performing ultrasound directly over regions of pain and swelling can be useful for diagnosing occult fractures of immature bones in pediatric-aged children. Sites of occult fractures included the elbow, knee, ischium, distal fibula, proximal femur, and humeral shaft. Ultrasonography clearly demonstrated cortical discontinuity in 92% of these cases. Indirect signs of fracture that were appreciated on ultrasound included step-off deformities, bone fragment avulsions, double-line appearance of cortical margins, and irregularities of bony surfaces. In addition, this technique has been introduced as a potential screening tool for long-bone fractures in pediatric trauma patients. A small study showed that the sensitivity was 89%, specificity 100%, with positive and negative predictive values of 100% and 97% respectively in detecting fractures. Further, ultrasound can aid in the assessment of need for fracture reduction. Barata et al. evaluated both upper- and lower-extremity fractures. Ultrasound detected long-bone fractures with a sensitivity of 95.3% and specificity of 85.5%. Ultrasound identified the need for reduction with a sensitivity of 100% and specificity of 97.3%. A recent study even suggests that point-of-care ultrasonography can be utilized for the evaluation of elbow fractures. Rabiner et al. showed a sensitivity of 98% and specificity of 70%, when ultrasound is compared with conventional radiographs. Overall, these studies suggest that ultrasound may play a larger role in decreasing the number of radiographs pediatric patients are exposed to in the future. It is also a helpful modality in situations where radiographs are of limited availability. Further studies need to be performed in order to assess the impact of this technology on actual clinical practice.
Technique
Transducer selection and orientation
When performing an assessment of long-bone fractures, a linear-array, high-frequency (5–10 MHz) transducer is typically preferred (Figure S3.3a). When the suspected injury is near a joint (such as the wrist), the conventional method for longitudinal image acquisition is to have the indicator oriented towards the direction of the closest joint.
Patient position and preparation
The patient should be in a position of comfort. Adequate analgesia should be given prior to performing ultrasonography. In order to further decrease pain, a liberal amount of ultrasound gel should be applied to the suspected fracture site, in order to minimize the degree of contact between the transducer and the injured extremity.
Ultrasound imaging
Longitudinal and transverse images should always be obtained (Figure 19.1). There are benefits to obtaining an additional “orthogonal” view during transverse image acquisition. First, this additional view allows for a more complete, multidimensional evaluation. Second, it can help guide and expedite the proper orientation for longitudinal image acquisition. Third, it may provide useful information such as the angle and direction of distal fragment displacement, providing a more complete assessment when determining the adequacy of fracture reduction.

Figure 19.1 Distal forearm fracture. (a) Transducer orientation along the long-axis of the bone, with the indicator oriented distally towards the wrist. (b) Transducer orientation along the short-axis or transverse view of the bone. (c) Longitudinal ultrasound image showing a disruption in the bony cortex, consistent with a fracture site and displacement of the distal fragment. The metaphysis (*), with the echogenic epiphysis, is adjacent to the fracture site. (d) Forearm radiographs performed later confirmed the presence of both a distal radius and ulna fracture.
Once the transducer is oriented in the correct position, the following findings suggest the presence of a long-bone fracture:
Ultrasound-guided procedure
Ultrasound may be performed during, and following the reduction of fractures. Dynamic imaging throughout the reduction provides a real-time visualization and reassessment of the reduction technique (Figure 19.2).
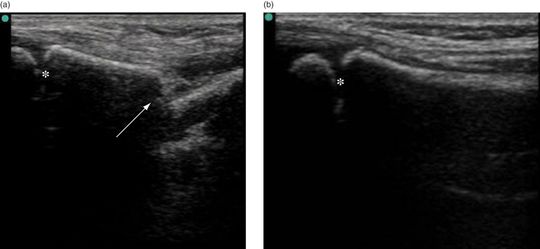
Figure 19.2 Distal radius fracture reduction. (a) Longitudinal ultrasound images of a distal radius fracture (arrow). (b) Longitudinal view of the radius, following a closed reduction. Note that the cortical discontinuity (arrow) in the pre-procedural ultrasound is not evident on the post-reduction image. The physis is visible on both images with the epiphysis (*).
Training and education
Training and competency for emergency physicians in ultrasound-guided fracture identification and fracture reduction should be established. Until proper credentialing standards are in place, point-of-care ultrasound for these types of injuries should be verified with a confirmatory study by the radiology department. A collaborative approach with the institution’s orthopedic surgery and radiology departments should be undertaken and will help ensure that high-quality images are obtained and interpreted by experienced providers in a timely fashion for the betterment of patient care.
Specific scanning techniques
Forearm
Anatomy
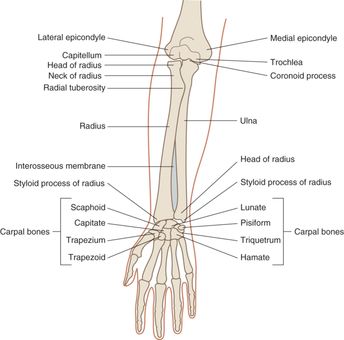
The forearm comprises the radius and ulna running in parallel and held together by an interosseus membrane and a network of various flexor and extensor muscles (Figure 19.3).
Technique
A short-axis, or transverse view is obtained by placing the transducer perpendicular to the bone (Figure 19.4a). Longitudinal views in the volar, lateral, and dorsal planes may be required to best localize and characterize the fracture site.
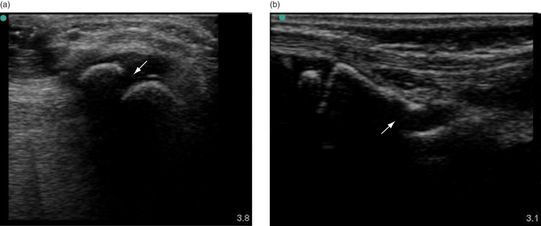
Figure 19.4 Forearm fracture. (a) Short-axis or transverse view of the radius. (b) Long-axis or longitudinal view of the radius. Note the disruption and displacement of the hyperechoic bony cortex (arrow) consistent with a fracture.
Lower extremity
Anatomy
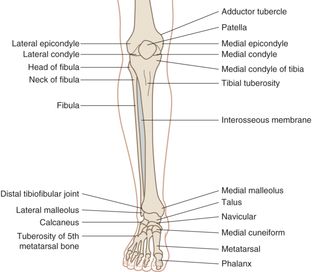
The lower extremity comprises the tibia and fibula running in parallel. Like the forearm, there is an intraosseous membrane (Figure 19.5).
Technique
At least two views of the lower-extremity long bones should be obtained. Position the transducer parallel to the long-axis of the bone and scan above and below the suspected fracture site. Then, orient the transducer perpendicular to the bone, in order to obtain the short-axis view. Again, scan above and below the suspected site of fracture. Disruption of the bony cortex may be visualized as a “step off” of the hyperechoic bone cortex (Figure 19.6).
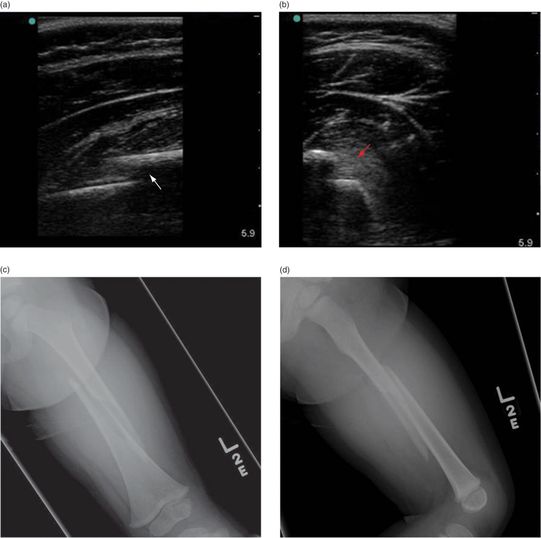
Figure 19.6 Femur fracture. (a) Longitudinal ultrasound view of the femur, with a notable deep discontinuity of the hyperechoic line (arrow), representing a fracture. (b) The fracture site (arrow) is again visible on the transverse view. (c,d) Corresponding AP and lateral radiographs of the mid-shaft, spiral femur fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








