Fractures are common in childhood.
Approximately 2% to 3% of children suffer a fracture treated in the emergency room within a given year.
Many isolated fractures heal readily with simple or no treatment.
Multiple fractures during childhood are common.
Cartilagenous growth plates persist in the growing skeleton as soon as secondary centers of ossification form at the ends of the long bones.
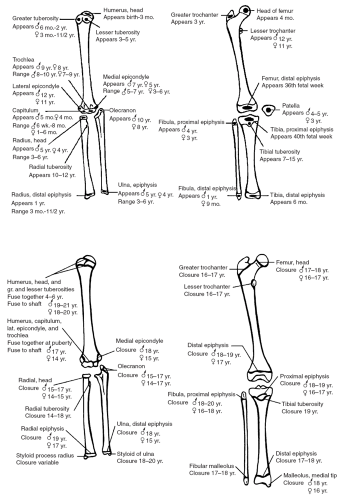
Average ages at which secondary centers of ossification appear and fuse to the skeleton are shown in Figure 12-1.
Growth plates account for the longitudinal growth of bones.
Growth plates are weaker in tension than the nearby bone and are commonly involved in fractures.
Most growth plate injuries heal rapidly and do not cause permanent alterations in longitudinal or angular growth.
Injuries with the potential to cause permanent growth arrests are:
Higher-energy injuries.
Injuries to the distal femoral physis.
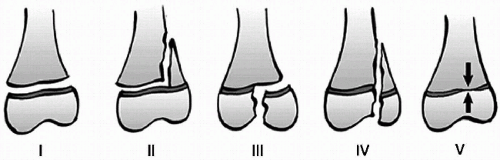
Injuries with higher numerical classification in the Salter-Harris scheme (Fig. 12-2).
Radiographic interpretation of the growing skeleton can be difficult due to:
Presence of growth plates.
Variations in the appearance of secondary ossification centers.
For example, the elbow has six secondary ossification centers.
Radiographic interpretation can be assisted by:
Referring to normal radiographs.
Taking comparison x-rays of the contralateral uninjured limb.1
Periosteum around children’s bones is much thicker, tougher, and more active than that around adult bones, because it is continually contributing to bone circumferential appositional growth.
Periosteum is often torn on the side of the bone that failed in tension (usually the direction the apex of angulation points) and is often intact on the opposite, compression side.
Intact periosteum confers stability after fracture reduction, but must be accommodated in performing the reduction maneuver.
Have a high index of suspicion for inflicted injury as the risk for re-injury and fatality is high.
The diagnosis remains a clinical one, using all information from history, physical findings, and radiographic and ancillary tests.2,3
Risk factors include:
Injuries inappropriate to the child’s developmental level (e.g., long bone fractures prior to walking age).
Delayed presentation.
Inconsistent history.
Unwitnessed injuries.
Multiple injuries.
Injuries at different stages of healing.
Inappropriate parent—child dynamics.
Specialized pediatric services or teams exist to provide comprehensive medical assessment in cases where inflicted injury is a possibility.
The legal responsibility to report suspected child abuse to governmental authorities (Children’s Aid Society) rests with the primary physician.
See Chapter 19 on Nonaccidental Injury for further details.
High—energy fractures are associated with more:
Nerve injuries.
Vascular injuries.
Skin injuries or open fractures.
Swelling or compartment syndromes.
Growth plate damage.
Delayed healing.
Permanent disability.
Additional fractures in the same limb or elsewhere.
Systemic injuries.
Central nervous system injuries.
Requirement for operative reduction and stabilization.
High-energy mechanisms include:
Motor vehicle occupant.
Pedestrian struck by motor vehicle.
Cyclist struck by motor vehicle.
Falls from heights (more than twice the child’s standing height).
Motorized sports and recreation.
High-speed activities (e.g., skiing, snowboarding).
Low-energy mechanisms include:
Sports and leisure injuries.
Team sports, field sports.
Playground injuries.
Falls.
Fractures can occur in the:
Diaphysis (shaft).
Metaphysis (flare).
Physis (growth plate).
Epiphysis (secondary center of ossification).
Metaphyseal and growth plate fractures heal in half the time of diaphyseal fractures of the same bone.
Intra-articular fractures are often accompanied by growth plate fractures in children (see the description of the Salter-Harris classification below).
Require accurate reduction and stabilization to prevent posttraumatic arthritis.
Fracture pattern reveals the type and direction of force.
Spiral fracture = twisting around long axis of bone.
Transverse fracture = bending force.
Transverse fracture with butterfly fragment = higher peak bending force, butterfly fragment is on concave (compression) side of the bent bone.
Oblique fracture = bending in compression.
Avulsion fracture = tensile force.
Five different anatomic patterns of growth plate injury.4
Risk of permanent damage to the growth plate is determined by:
The energy of the fracture.
The specific growth plate involved.
The fracture pattern.
Upper-extremity growth plates commonly have low-energy injuries.
Results in type I and II fracture patterns.
Almost never have permanent problems.
Lower-extremity growth plates are much stronger.
Even type I or II injury of the distal femur has a high risk of growth arrest.
Early orthopedic consultation is suggested for all growth plate injuries in the lower extremity, and for high-grade (Salter-Harris III or IV) or high-energy and displaced injuries in the upper extremity.
Risk factors for infection include:
High-energy trauma.
More extensive soft-tissue damage.
Contamination.
Circulatory impairment.
Delay prior to surgical debridement.
Antibiotic and tetanus administration depend on extent of injury and contamination.
Grade I and clean grade II injuries require gram-positive coverage.
Contaminated grade II and all grade III injuries require:
Gram-positive and gram-negative coverage.
May require anaerobic coverage if:
– Gross amounts of soil or fecal material are present.
– A lot of dead or devitalized tissue is present.
– Tetanus toxoid and/or immune globulin may be indicated for patients whose immunity is not up to date (Table 12-2).
TABLE 12-1 Gustillo Classification of Open Fractures | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Cervical spine protection must be maintained until bony or ligamentous injury has been excluded.
See Chapter 9 on C-spine Injuries.
Cervical spine held in neutral position with combination of:
Appropriately sized cervical collar.
Sandbags or rolled towels secured against the side of the head.
In infants, the larger head flexes the neck if supine on a flat surface. (Fig. 12-3)
For children <4 years, maintain the neck in neutral position with one of the following:
A hollow beneath the head.
A folded towel or small blanket under the shoulders.
Consider cervical spine injury:
In all cases of head injury.
If patient complains of neck pain.
Patients with any neurologic deficit.
Bind the pelvis circumferentially with a sheet to decrease its internal volume.
Prompt orthopedic consultation is required, as external fixation of the pelvis is part of the resuscitation for patients with pelvic fracture and excessive blood loss.
Concomitant abdominal injury may require laparotomy.
Can be performed at the same operative session as pelvic stabilization.
There is little proven role for angiographic embolization of pelvic bleeding in children until pelvic stabilization has been achieved.
Femoral fractures can contribute to blood loss (500 mL to 1 L per femoral fracture, or 20% of blood volume), but an isolated femoral fracture is unlikely the cause of hemodynamic instability, so other causes should be sought.1
Open wounds with ongoing visible blood loss are best managed by direct pressure over the bleeding point. Avoid attempts to clamp vessels blindly.
Intravenous lines placed peripherally should be put into uninjured or less injured limbs to ensure that infused fluids and drug reach the central circulation.
Impaired circulation in a deformed limb can be substantially improved by realigning and splinting the limb in near-anatomic position.
TABLE 12-2 Guide to Tetanus Prophylaxis in Routine Wound Management in Children and Adolescents | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree