Orthopedic Injuries
Suzan Schneeweiss
Introduction
Pediatric Differences
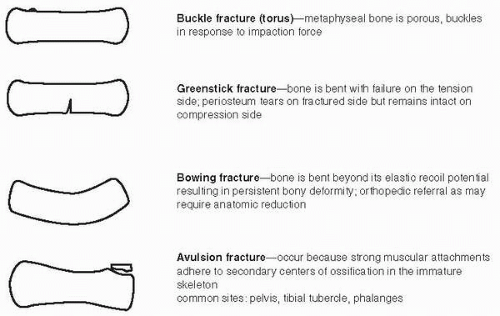
Bones more porous and pliable → bend, buckle, or break (greenstick fracture)
Thick periosteum:
Often remains partially or entirely intact despite fracture; helps in reduction and maintenance of reduction
Highly vascular, role in bone formation and fracture healing
Growth plate injuries common as growth plate (physis) cartilaginous, weaker than ligaments
Sprains are diagnoses of exclusion
Fractures heal more rapidly; therefore, less immobilization time
Clinical Presentation
Children do not localize pain well, must examine entire limb
Mechanism of injury may be difficult to obtain: need to consider common pediatric fracture patterns
Child abuse can produce any type of fracture or injury; consider if:
Undisplaced avulsion fractures at metaphyses (corner or bucket handle fractures)
Spiral fractures in children < 2 years
Posterior rib fractures
Mechanism of injury does not fit with injury sustained
Delay in seeking medical attention
Children only complain if something is wrong; immobilizing extremity should reduce pain; if persistent crying or pain, consider tight cast with nerve compression or compartment syndrome
Investigations
Good-quality X-rays
Selectively X-ray opposite limb if uncertainty regarding radiolucent line, growth plate, center of ossification vs avulsed fragment
Management
Splint prior to X-ray for comfort and to minimize soft-tissue trauma
Analgesia (see Chapter 64)
If in doubt, immobilize extremity (see Chapter 62 for casting instructions)
Crutches: only for children > 8 yrs
Soft-tissue injuries
RICE: Rest, Ice, Compression, and Elevation
Return to function as tolerated
Avoid rigorous physical activity × 3 weeks
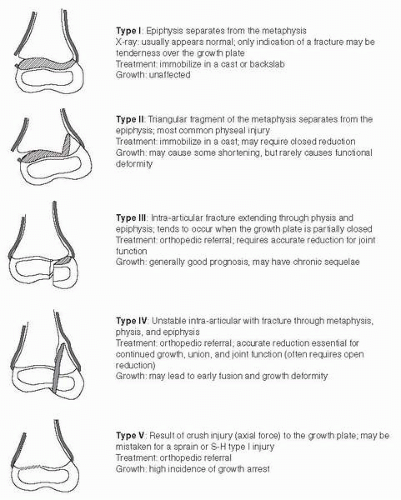
Salter-Harris Fractures
Account for 10-15% of childhood fractures
Most heal in 3-6 weeks
Damage to growth plate has the greatest potential for producing deformity: progressive angular deformity, limb-length discrepancy or joint incongruity
Common Injuries
Shoulder and Arm
Clavicular Fracture
Commonly from fall onto tip of shoulder
Treatment is supportive: immobilize in sling (figure of eight sling is not indicated)
Toddler 7-10 days, younger child 2-3 wks, older child 3-4 wks
Consider orthopedic referral: fractures of the distal clavicle (equivalent to acromioclavicular separation), tenting of skin
Shoulder Dislocation
Rare in children < 12 yrs
> 95% are anterior dislocations
Physical examination: arm held in adduction with slight internal rotation, sharp shoulder contour, prominent acromion
Document axillary nerve function, distal pulses
X-ray to confirm diagnosis and post reduction films to confirm anatomic placement: AP, lateral, axillary views if possible
Treatment
Procedural sedation
Multiple techniques for reduction
Traction-countertraction technique:
Assistant applies countertraction with a sheet wrapped around chest
Operator exerts linear traction on the arm, then slight lateral traction to reduce the proximal humerus
Immobilize in sling for comfort and refer to orthopedics for follow-up
Can resume full activity within 2-3 weeks
Proximal Humeral Fracture
Most are S-H type II injuries and can be simply treated with a sling
Large degree of angulation is generally accepted because of the tremendous remodeling potential
Humeral Shaft Fracture
Most caused by high-energy direct blow (transverse fracture)
If fracture with minimal trauma, consider pathologic fracture (common location for bone cysts and other benign lesions): present with localized pain, swelling, deformity
Spiral fracture: produced by a twisting motion
Consider child abuse in an infant or toddler
Treatment: Velpeau sling because most reduce themselves by gravity
Orthopedic referral if > 15-20° angulation or rotational deformity
Complications: radial nerve injury
Elbow
Normal X-ray Features
Obtain two views: AP in extension and lateral in 90° flexion
Need to consider stages of ossification: use mnemonic
Age at ossification | |
|---|---|
C: Capitellum | 1-2 years |
R: Radial head | 3 years |
I: Internal or medial epicondyle | 5 years |
T: Trochlea | 7 years |
O: Olecranon | 9 years |
E: External or lateral epicondyle | 11 years |
Anterior Fat Pad
Posterior Fat Pad
Radiolucency posterior to distal humerus and adjacent to olecranon fossa
Not visualized on a normal lateral X-ray; if present, then abnormal
Anterior Humeral Line
Line drawn from the anterior cortex of the humerus intersects the capitellum in its middle third
Posteriorly displaced supracondylar fracture: anterior humeral line passes through anterior third of capitellum or may miss it entirely
Radial Axial Line
Line drawn along the axis of the radius passes through the center of the capitellum in all projections
Figure-of-Eight
Seen on true lateral elbow X-ray
If disrupted, may indicate fracture
Supracondylar Fracture
Most common between ages 3-10 years
Most common elbow fracture (60%)
Usually results from fall on outstretched hand with elbow hyperextended (e.g., fall from monkey bars)
Present with localized swelling and tenderness of elbow
Essential to ensure intact neurovascular status
Complications include nerve injury, compartment syndrome with Volkmann’s ischemia, and cubitus varus (“gunstock” deformity)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree