Figure 35.1
Beginning dissection of the posterior sheath. The posterior sheath is incised 1 cm lateral to the linea alba and grasped with an Aliss clamp to aid in retraction

Figure 35.2
Complete posterior sheath dissection. Retractors are on the rectus abdominis muscle
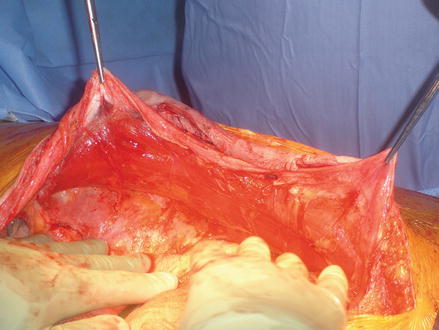
Figure 35.3
Perforating neurovascular bundles can be seen laterally at the linea semilunaris
After the posterior sheath dissection is complete, the posterior sheath is closed using a running 2-0 Polydiaxanone (PDS) suture (Ethicon, Cincinnati, OH) (Fig. 35.4). Sponge and needle counts should be completed at this time as the abdomen will be essentially closed at this point. The retrorectus space is then measured and an appropriately sized piece of mesh is selected. There are a wide variety of mesh products that can be utilized in this space. For all clean cases, we prefer a midweight macroporous synthetic mesh. This mesh is cut to fit the retrorectus space and 0 PDS sutures are preplaced on the mesh at the top, bottom, and along both sides at regular intervals. As there is limited room for the mesh to migrate 6-8 sutures are generally all that is needed for adequate fixation. The mesh is then placed in the retrorectus space and the sutures are passed transfascially through separate stab incisions using the Reverdin suture passer (Figs. 35.5 and 35.6). Once all of the sutures have been passed, they are tied down and a 15 Fr closed suction drain is placed on top of the mesh in order to prevent seroma formation. The anterior sheath is then closed with a running 0 PDS suture using small, frequent bites (Fig. 35.7). The incision is then closed with staples on interrupted nylon sutures and a dry sterile dressing is placed over the wound.










