Figure 5.1
The patient is placed in the lateral position. The operating table is then broken to maximize the space between the costal margin and the iliac crest. The bean bag is then aspirated to firmness to secure the patient in place
Preoperative Preparation
Pre-operative workup is essential to diagnose a functional adrenal tumor. The common syndromes that require evaluation are Conn’s syndrome, pheochromocytoma, Cushing’s syndrome, and functional adrenocortical carcinoma, which usually has Cushing-virilizing features. Open adrenalectomy is usually reserved for large pheochromocytomas or functional and non-functional adrenocortical carcinomas [5, 6].
A full preoperative workup for hyperaldosteronism, Cushing’s syndrome and pheochromocytoma is reviewed in detail by Young [5] and Sidhu et al. [7].
At induction, patients should have DVT prophylaxis with subcutaneous fractioned heparin or equivalent, pneumatic calf compressors as well as an indwelling bladder catheter and a nasogastric tube.
Positioning
The patient is placed in the lateral position with the operating table placed in maximal flexion to accentuate the space between the costal margin and the iliac crest. A bean bag is useful to secure the patient in position and appropriate strapping is provided (Fig. 5.1).
Description of Procedure
Right Sided Adrenalectomy
The costal margin is palpated and a subcostal incision two fingerbreadths below the costal margin is performed from the mid-clavicular line medially to the mid-axillary line posteriorly. This incision can be extended down to the midline anteriorly if required. The skin and underlying fat along this line are incised. The external oblique, internal oblique and transverse abdominal muscles are divided using cautery. The peritoneum is then entered sharply exposing the peritoneal cavity. At this point, full palpation of the peritoneal cavity is required to exclude metastatic disease.
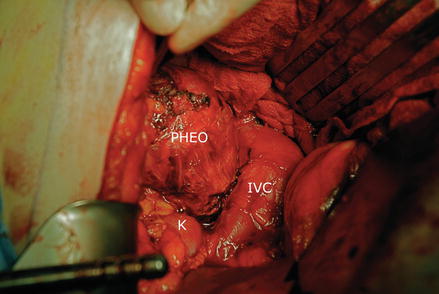
The hepatic flexure of the colon is mobilized and retracted inferiorly. The duodenum can then be kocherized to allow better access to the IVC. The liver is mobilized medially and superiorly by dividing the right triangular ligament (Fig. 5.2). Morrison’s pouch is then entered by incising the peritoneum below the liver and overlying the adrenal gland. The superior margin of the adrenal tumor is identified. The lower margin of the tumor and the renal vein are identified inferiorly (Fig. 5.3). Medial to the tumor, the IVC can then be identified by a combination of sharp and blunt dissection after incising the overlying peritoneum. We aim to triangulate the dissection onto the adrenal vein from below and above (Fig. 5.4). With the patient in the lateral position, the adrenal vein is encountered as the IVC is passing under the liver. Once the adrenal vein is secured, the tumor is lifted off from the retroperitoneum and the feeding arteries, which arise from the inferior phrenic, the aorta and the renal arteries are ligated and divided with a thermal sealing device.
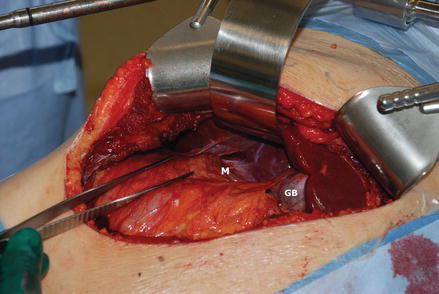
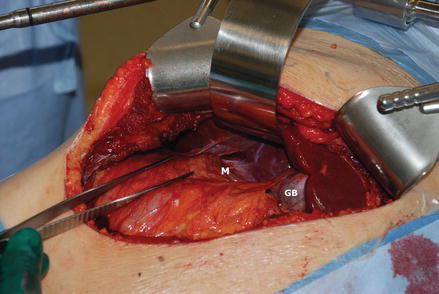
Figure 5.2
A subcostal incision is made, the muscle layer is divided and the peritoneal cavity entered. The triangular ligament is divided, the liver retracted superiorly and the peritoneum of the hepatorenal pouch is divided to gain access to the upper border of the adrenal tumor (M). GB gallbladder