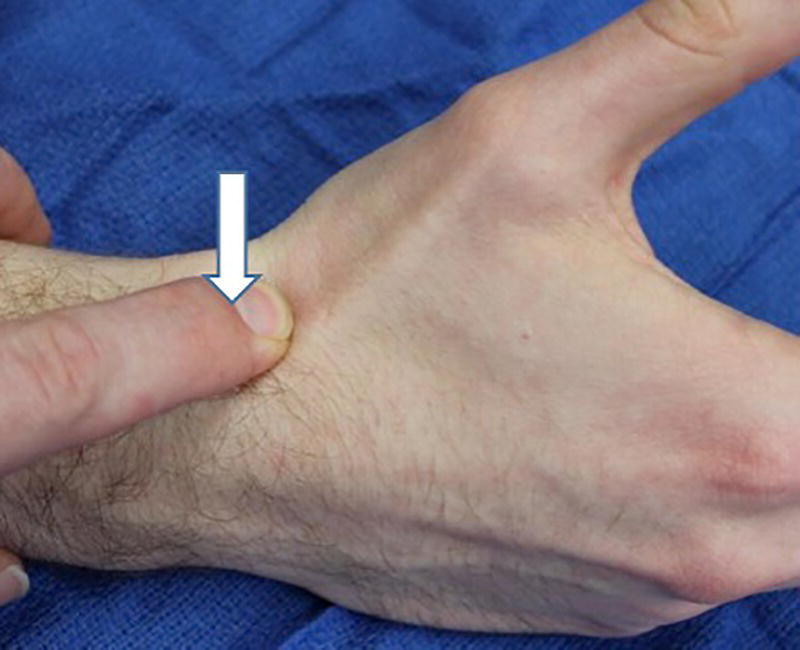
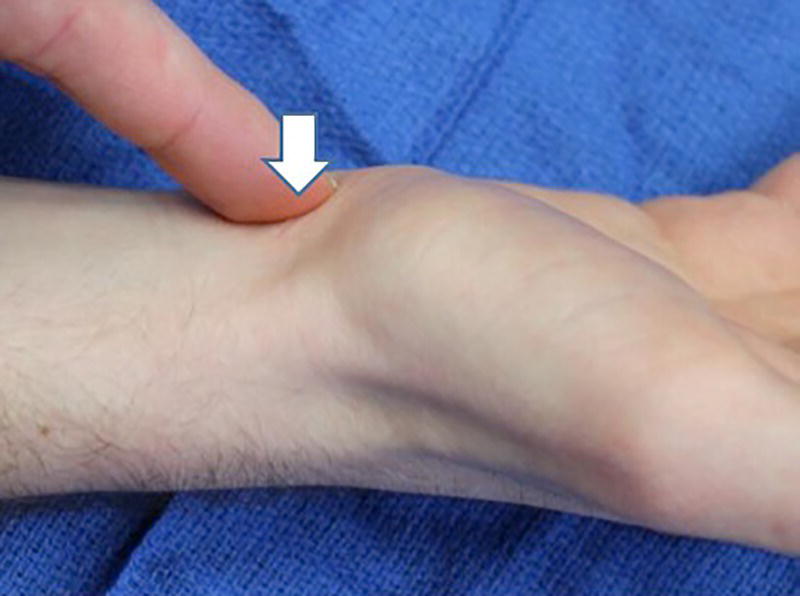
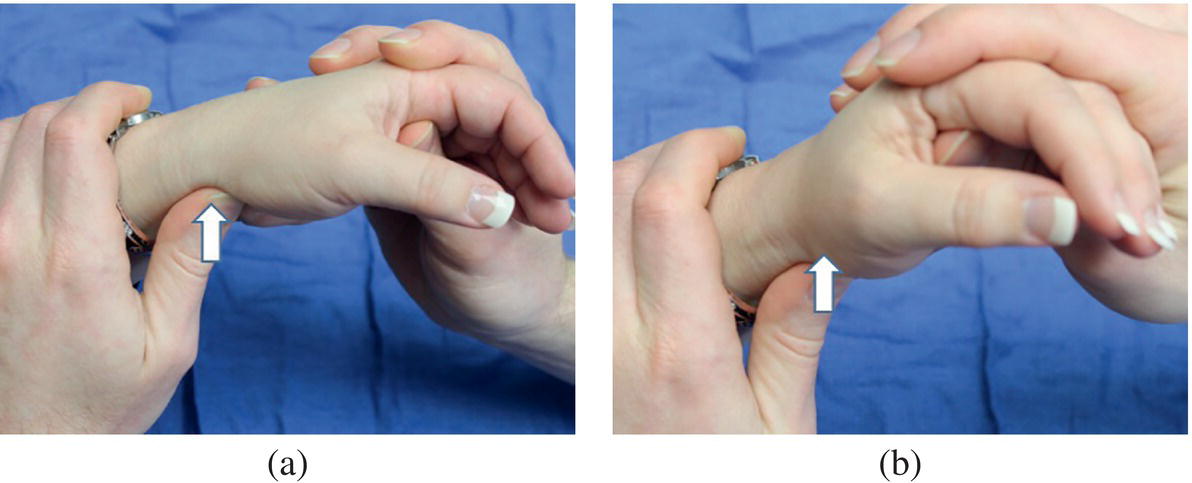
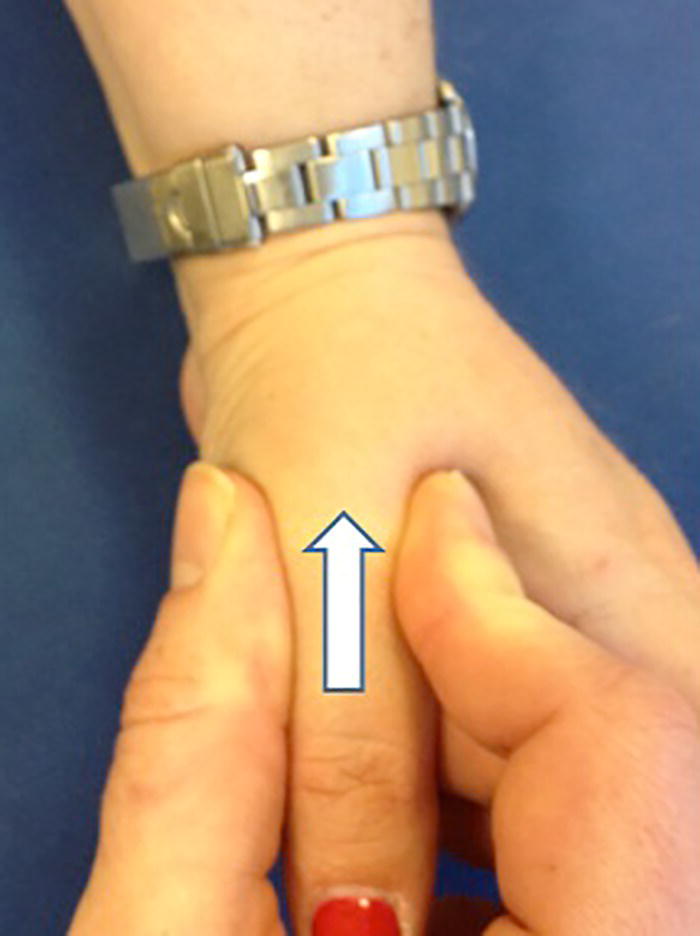
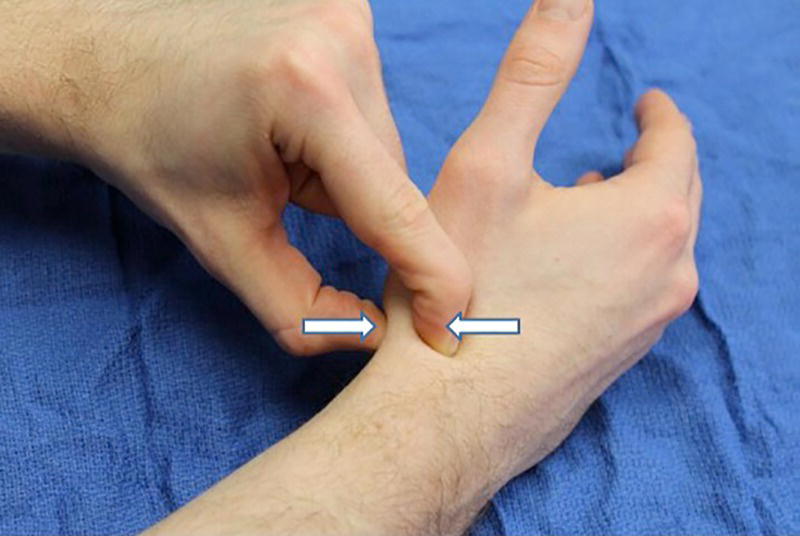
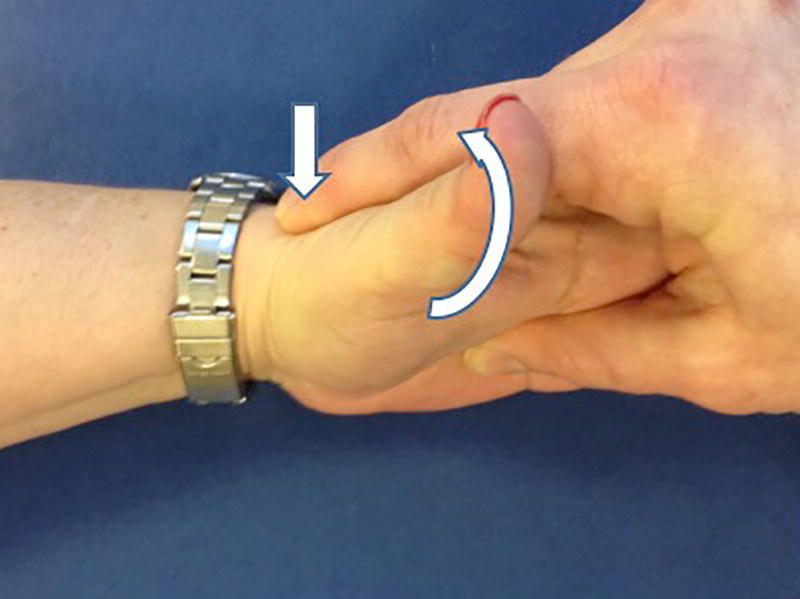
Christopher R. Carpenter1 and Ali S. Raja2 1 Department of Emergency Medicine, Washington University School of Medicine, St. Louis, MO, USA 2 Department of Emergency Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA Scaphoid fractures account for 70% of all carpal fractures presenting to the emergency department (ED). Missed scaphoid injuries represent an uncommon but expensive source of malpractice risk.1 The most common reasons for litigated missed scaphoid fractures include failure to obtain an X‐ray and inadequate return instructions.2 In ED studies of adult patients with suspicious acute wrist injuries, the prevalence of a scaphoid fracture ranges from 12% to 57%.3 The differential diagnosis of scaphoid fracture includes other fractures, ligamentous injuries, or arthritis (Box 16.1). Suspicion of a scaphoid fracture is based largely on a patient’s mechanism of injury, classically a fall on an outstretched hand. Scaphoid fractures are most common in adolescents and young adults. Various physical examination tests exist for scaphoid fracture (Figures 16.1–16.6).3 Clinicians should maintain a high level of suspicion either when a compatible mechanism is described or if any of the associated signs are elicited on exam for patients with acute wrist trauma and pain. As the scaphoid bone has a retrograde blood supply, failure to diagnose a scaphoid fracture in the ED can increase the risk of avascular necrosis, nonunion, and delayed union, all of which can lead to varying degrees of degenerative osteoarthritis and arthrosis. Once a scaphoid fracture is diagnosed, referral to a hand surgeon and prompt immobilization of the wrist are therefore imperative. Treatment in the ED should include immobilizing the suspected injury with a thumb spica (or other similar) splint. Figure 16.1 Anatomical snuffbox tenderness. Dorsal wrist tenderness in the anatomic snuffbox elicited between the extensor pollicis longus (EPL) and extensor pollicis brevis (EPB) tendons. Figure 16.2 Scaphoid tubercle tenderness. Tenderness over the distal scaphoid tubercle is elicited on the palmar surface at the level of the wrist flexion crease. Figure 16.3 Scaphoid shift (Watson’s test). Scaphoid shift test is performed with the examiner placing one thumb under the distal scaphoid tubercle distally and using the other hand to hold the patient’s hand. Gentle ulnar and radial deviation makes the scaphoid tubercle identifiable as it becomes more prominent with radial deviation. Figure 16.4 Starting in ulnar deviation, the examiner puts pressure under the distal scaphoid pushing dorsally as the wrist is radially deviated. If the scapholunate ligament is incompetent then scaphoid flexion is blocked and the proximal scaphoid subluxes over the dorsal radius rim and then reduces with a clunk as pressure is released from the volar scaphoid. A positive test must reproduce pain and result in the palpable subluxation and reduction of the scaphoid. Figure 16.3 is in ulnar deviation and this figure is in radial deviation as the maneuver is completed. Figure 16.5 Axial load (thumb compression test). To axial load the scaphoid, the examiner grasps the patient’s thumb and provides axial compression to reproduce pain over the scaphoid. Figure 16.6 Clamp sign. The clamp sign is demonstrated when asking the patient to point to the location of pain and they will clasp the scaphoid with the opposite hand pinching between the dorsal and volar scaphoid waist. While plain radiography is typically used as the initial imaging modality for suspected scaphoid fractures (Figure 16.7), the first ED X‐ray has a positive likelihood ratio (LR+) of only 2.4 (95% confidence interval [CI] 0.84–6.6) and negative likelihood ratio (LR−) of 0.23 (95% CI 0.08–0.70).4,5
Chapter 16
Occult Scaphoid Fractures
Background
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






