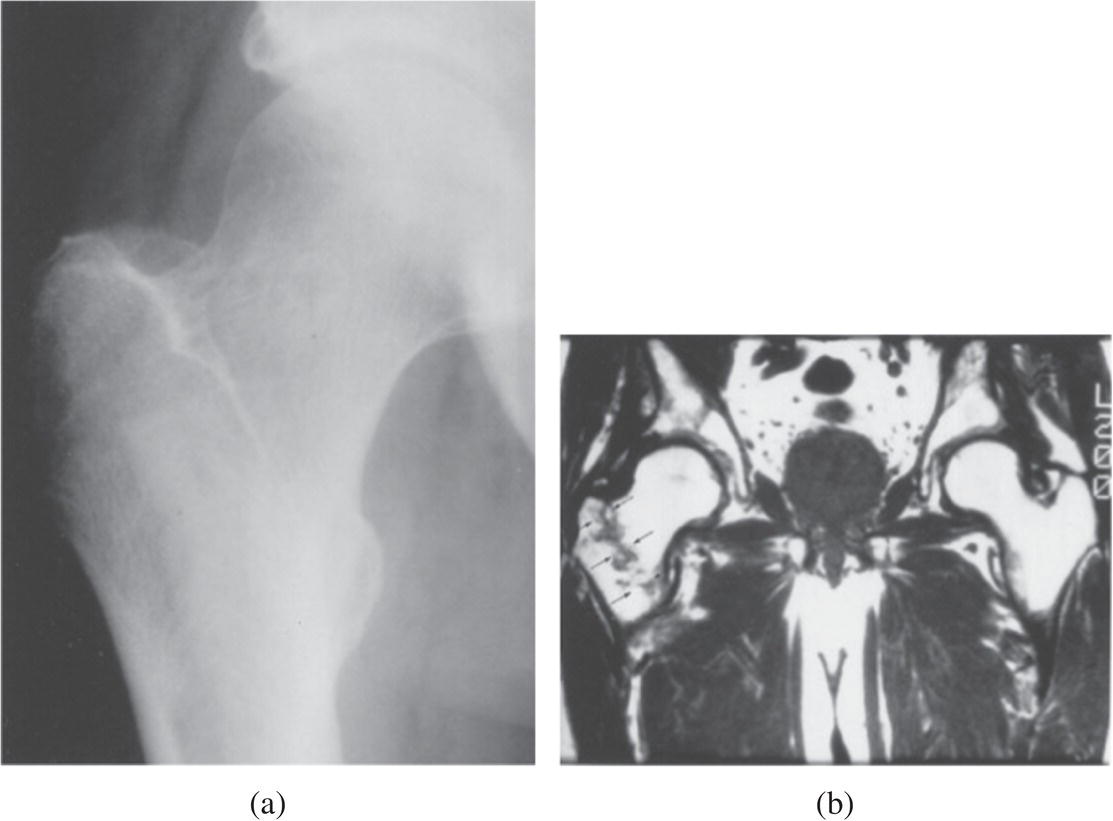
Ali S. Raja1 and Jesse M. Pines2,3 1 Department of Emergency Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA 2 US Acute Care Solutions, Canton, OH, USA 3 Department of Emergency Medicine, Drexel University, Philadelphia, PA, USA Hip fractures are common in geriatric adults, and the incidence is increasing with aging global populations. It is estimated that the incidence of hip fracture will rise from 1.66 million in 1990 to 6.26 million by 2050, with incidence varying significantly by country.1,2 Many patients with hip fractures will present to the emergency department (ED) for evaluation and treatment, typically following a fall or other acute traumatic injury. The diagnosis of hip fracture is typically not a diagnostic dilemma because plain radiographs are often diagnostic, particularly in patients with classic anatomic deformities (Figure 14.1). However, a small proportion of patients with hip fracture (2–9%) will have initially negative plain films.3 These occult hip fractures are more common in the elderly because of the high prevalence of osteoporosis in this age group.4 Delayed surgical treatment has been associated with increased mortality, suggesting that delays in diagnosis may worsen outcomes.5 Emergency physicians, therefore, face a diagnostic dilemma when treating a patient in whom they have a high suspicion for hip fracture based on physical examination or history but whose plain radiographs are negative or equivocal. The classic case is an older adult patient who has fallen, has hip tenderness, and cannot bear weight on the affected leg. A missed diagnosis of hip fracture can place older adults at substantial risk of fracture displacement, avascular necrosis, and the need for more involved surgical procedures. Figure 14.1 Hip fractures. This illustration depicts the different types of proximal hip fractures. (Knoop et al. Atlas of Emergency Medicine 2nd edition, 2002). Approaches to the diagnosis of occult hip fractures have evolved over the last several decades. Previously, repeat plain films or bone scans were recommended. Bone scans will typically become positive after 24–72 hours following an acute fracture. More recently, clinicians have increasingly used computed tomography (CT) or magnetic resonance imaging (MRI) in this setting (Figure 14.2).6 Certain historical factors can predict the presence of hip fractures in patients with acute traumatic hip pain, such as the inability to ambulate. Patients whose ambulatory status cannot be assessed require further imaging to exclude occult hip fracture. MRI has been advocated as the test of choice due to its extremely high sensitivity. However, this modality is frequently unavailable in acute settings or limited by contraindications to MRI in older adults with implanted devices such as pacemakers, or behavioral issues such as dementia. Clinicians will often be faced with the dilemma of which advanced imaging modality to obtain: CT or MRI? Figure 14.2 Occult hip fracture. (a) Anteroposterior radiograph of a 65‐year‐old patient on steroids who had right hip pain after a fall. No fracture is evident. (b) A T1‐weighted coronal MRI of the same hip clearly demonstrates a nondisplaced hip fracture (thin arrows). (Reproduced from Tintanelli et al. (2004), with permission of McGraw Hill Education, Inc.) In patients with hip injury and normal X‐ray, can the clinical exam reliably exclude significant fractures? One small retrospective single‐center study attempted to examine the value of various clinical signs in relation to this question.7
Chapter 14
Occult Hip Fracture
Background
Clinical question
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






