Normal and abnormal CTGs.
A normal cardiotocograph trace. The baseline is 135 beats/min variability 25 beats/min accelerations present and no decelerations.
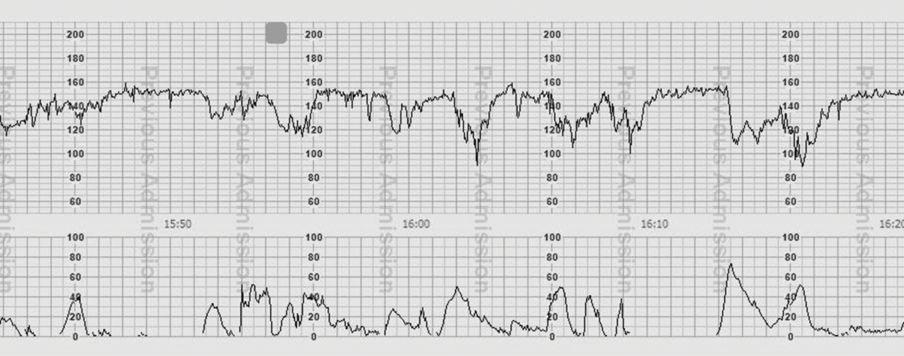
A pathological cardiotocograph trace demonstrating late decelerations. The radar of the deceleration and the peak of contraction are marked with arows.
| Feature | Baseline (bpm) | Variability (bpm) | Decelerations | Accelerations |
|---|---|---|---|---|
| Reassuring | 110–160 | ≥5 | None | Present |
| Non-reassuring | 100–109 161–180 | <5 for 40–90 minutes | Typical variable decelerations with over 50% of contractions, occurring for over 90 minutes Single prolonged deceleration for up to 3 minutes | The absence of accelerations with otherwise normal trace is of uncertain significance |
| Abnormal | <100>180 Sinusoidal pattern ≥10 minutes | <5 for >90 minutes | Either atypical variable decelerations with over 50% of contractions or late decelerations, both for over 30 minutes Single prolonged deceleration for more than 3 minutes |
| Category | Definition |
|---|---|
| Normal | An FHR trace in which all four features are classified as reassuring |
| Suspicious | An FHR trace with one feature classified as non-reassuring and the remaining features classified as reassuring |
| Pathological | An FHR trace with two or more features classified as non-reassuring or one or more classified as abnormal |
Baseline rate
The normal fetal heart rate is 110–160 bpm, with the mean tending to fall as gestation progresses. A low baseline (100–110 bpm) or a tachycardia (160–180 bpm), where accelerations are present and no other adverse features appear is not regarded as suspicious. This may represent a baseline reduction following opiate administration, or a tachycardia with an active fetus, both of which may eventually settle. FHR is affected by maternal pyrexia and/or tachycardia and usually rises by 10–15 bpm. A slow rise in baseline over the duration of a labour may indicate increasing fetal acidosis and should be regarded as suspicious. A baseline rate of <100 or >180 is always abnormal.
Variability
Variability is defined as the beat-to-beat variation, and should be greater than 5 bpm; it represents the fetal autonomic nervous system function. A reduction in variability for up to 40 minutes may be normal with the fetal sleep cycle. A reduction in variability has low sensitivity but high specificity for fetal acidosis.
Accelerations
The presence of accelerations in the FHR of greater than 15 bpm for 15 seconds is a reassuring feature suggesting fetal activity. The presence of accelerations has a high specificity for excluding fetal acidosis, although the absence of accelerations does not denote a suspicious or pathological CTG trace.
Decelerations
The presence of decelerations is a non-reassuring or abnormal feature on a CTG, and is classified according to the type (early, late and variable), duration and frequency. Early decelerations are uniform in size, shape and duration and are likely to represent head compression in the late first or second stages of labour rather than hypoxia. Critically, early decelerations start with uterine contractions and the FHR has normally returned to baseline as the contraction finishes.
Late decelerations are so called because the deceleration in FHR starts to occur after the uterine contraction peaks, and persists after the contraction finishes. Late decelerations are more indicative of fetal hypoxia.
Variable decelerations are more common, accounting for more than 80% of decelerations seen. They are defined as a reduction from the baseline more than 15 bpm for 15 seconds with varying length, amplitude and uniformity. Commonly as a result of cord compression, variable decelerations are sub-classified into typical (which may be found near the end of the second stage of labour) or atypical. Atypical variable decelerations are more concerning and may show a loss of shouldering (accelerations before and after the deceleration), a smooth decline, with a slow recovery to baseline which may overshoot, or be biphasic in shape.
When a CTG is normal the baby is very likely to be well, but the majority of abnormal CTGs occur in babies who are not distressed. A suspicious CTG requires review by an obstetrician for a management plan, which will depend on the overall clinical picture and the duration of concern. For example, the presence of variable decelerations in early labour is of more concern than near delivery. Suspicious features may respond to simple measures that can be performed to optimize placental perfusion.
These techniques may include:
Changing of maternal position
Adequate hydration with intravenous crystalloid fluid
Avoiding uterine hyperstimulation by judicious use of oxytocin
Reduction of maternal pyrexia by paracetamol and/or antibiotics.
If suspicious features persist, then consideration of further assessment with fetal blood sampling should be made. Unlike a CTG classified as suspicious, a pathological CTG requires action. This may mean expediting birth by instrumental delivery if imminent or by further assessment of fetal wellbeing by fetal blood sampling. If labour is not advanced enough to permit this (<3 cm dilated), or is contraindicated, then delivery by emergency caesarean section is required if pathological features persist.
Fetal blood sampling (FBS)
As an abnormal CTG has a relatively low positive predictive value (PPV) for acidosis, FBS is performed in most UK units in an attempt to reduce false positive diagnosis of fetal compromise and corresponding unnecessary intervention. Fetal blood sampling provides current fetal pH and base excess.
Serious adverse sequelae in the newborn period are rare after birth with umbilical cord pH greater than 7.0 or base excess less than −12 mmol/L.
FBS should be performed with the consent of the mother with full understanding that the subsequent result may influence the mode and urgency of delivery or that the FBS may need repeating should the CTG continue to be pathological. FBS is ideally performed in the left lateral position to optimize placental perfusion. Contraindications to FBS include gestation earlier than 34 weeks, maternal blood-borne infection (HIV, active hepatitis B and C) and potential inherited fetal bleeding disorders. Should there be a pathological trace where FBS is contraindicated, technically impossible due to dilatation, a failure of collection or the mother refuses the FBS, delivery should be expedited on the presumption of fetal acidosis.
FBS results should be interpreted in the context of the progress of labour (Table 6.2). FBS should not be performed with obvious fetal compromise as indicated by prolonged (>4 minutes) bradycardia or when vaginal delivery can be easily achieved using ventouse or forceps. In these cases immediate delivery should be expedited.
| FBS result (pH) | Interpretation | Appropriate action |
|---|---|---|
| ≥7.25 | Normal | Appropriate sampling should be repeated no more than 60 minutes later if the FHR trace remains pathological, or sooner if there are further abnormalities |
| 7.21–7.24 | Borderline | Sampling should be repeated no more than 30 minutes later if the FHR trace remains pathological, or sooner if there are further abnormalities |
| ≤7.20 | Abnormal | Consultant obstetric advice should be sought, with a view to an urgent birth |
An abnormal FBS result requires urgent delivery. The delivery should be performed by the fastest and safest mode relevant to the operators’ skill and experience.
Classification of urgency of delivery
The Sentinel Caesarean Section Audit suggested that in cases such as cord prolapse, a decision-to-delivery interval (DDI) of 15 minutes was feasible. However, in many Category 1 decisions, delivery within 30 minutes was not achieved. Once a decision to deliver has been made, delivery should be carried out with the urgency appropriate to the risk for that baby and the safety of its mother (Tables 6.3 and 6.4). Evidence suggests that delay is often associated with transfer to theatre.
| Category | |
|---|---|
| 1 | Immediate threat to the life of the woman or fetus |
| 2 | Maternal or fetal compromise that is not immediately life-threatening |
| 3 | No maternal or fetal compromise but needs early delivery |
| 4 | Delivery timed to suit woman or staff |
| Category | Time from decision to delivery |
|---|---|
| 1 | 30 minutes |
| 2 | 75 minutes |
| 3 | 24 hours |
| 4 | Timed to suit patient and staff |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






